Abstract
Purpose
Docetaxel and gefitinib play key roles in the treatment of non-small-cell lung cancer (NSCLC), and their combination could be of interest. Both drugs are mainly metabolized by CYP3A4, and drug–drug interactions are a major concern. This phase I dose-finding study was designed to assess the tolerability and drug–drug interactions in this combination using full pharmacokinetic (PK) samplings.
Methods
Docetaxel was intravenously administered on days 1 and 22 at a dose of 45 or 60 mg/m2. Gefitinib (250 mg/day) was orally administrated starting on day 2. Ten PK samplings of docetaxel were performed on days 1 and 22. Seven PK samplings of gefitinib were performed on day 18 ± 3 and on day 22.
Results
Twelve patients with advanced or metastatic NSCLC were enrolled without considering EGFR mutation status. The major toxicity was neutropenia. Two patients withdrew from this study due to dose-limiting toxicities; however, the toxicity profiles in this combination were generally acceptable. The docetaxel AUC0–24 and C max did not differ whether administered alone or with gefitinib, and the geometric mean ratios (GMRs) of AUC0–24 and C max (co-administrated/administrated alone) were 0.95 (90 % CI 0.85–1.06) and 0.95 (90 % CI 0.85–1.05), respectively. Furthermore, the GMRs of the steady state gefitinib AUC0–24 and C max were 0.93 (90 % CI 0.84–1.03) and 0.98 (90 % CI 0.88–1.09), respectively.
Conclusion
The tolerability of 60 mg/m2 docetaxel with 250 mg/day gefitinib was confirmed, and we observed no drug–drug interaction in this combination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is widely recognized as the leading cause of cancer-related deaths in the West and in Japan [1]. Non-small-cell lung cancer (NSCLC) constitutes about 80–85 % of lung cancers; however, more than half are diagnosed as advanced or metastatic disease. More effective and individualized treatments are needed for these advanced populations.
Platinum-based chemotherapy is a standard regimen for advanced NSCLC as a first-line treatment. The response rate and median survival time average around 30 % and 12 months, respectively, in unselected NSCLC [2]. Unfortunately, all patients show disease progression. Therefore, second-line treatment is required, and docetaxel and pemetrexed have been established as the standard of care [3].
Docetaxel has demonstrated survival advantages over the best supportive care and conventional anticancer drugs (i.e., ifosfamide and vinca alkaloids) [4, 5] and plays a key role in the treatment of advanced NSCLC. The major toxicities are hematological, including neutropenia and leukopenia, and other non-hematological toxicities include nausea, fatigue, sensory neuropathy, alopecia, and diarrhea [6]. Neutropenia is a dose-limiting toxicity that is highly correlated with docetaxel drug exposure [7]. The increasing area under the plasma concentration–time curve (AUC) correlates with increased dose of docetaxel proportionately, and docetaxel clearance (CL) is a strong independent predictor of neutropenia and febrile neutropenia [8, 9].
Gefitinib is a key drug for the treatment of epidermal growth factor receptor (EGFR)-mutant advanced NSCLC [10]. This drug binds the tyrosine kinase domain of EGFR and inhibits downstream signaling for cancer cell growth. The recommend dose of gefitinib (250 mg/day) is the minimal active dose determined by previous randomized phase II trials considering the toxicity profiles [11, 12]. In previous large-scale randomized trials, gefitinib demonstrated improved progression-free survival and response rate compared with conventional cytotoxic chemotherapies for EGFR-mutant advanced NSCLC [13, 14]. The major toxicities are rash, diarrhea, and liver dysfunction, and interstitial pneumonitis is a concern [11, 12].
Although docetaxel and gefitinib are active and important drugs for the treatment of advanced NSCLC, more effective treatments are required to improve outcomes and control cancer-related symptoms. We investigated the combination of docetaxel and gefitinib as a treatment for advanced or metastatic NSCLC. These two drugs are mainly metabolized by CYP3A4 [15, 16]. Docetaxel has a narrow therapeutic window, and drug exposure is highly correlated with neutropenia; therefore, effects on the docetaxel pharmacokinetic (PK) profile by combination with gefitinib could be a major concern. We conducted a phase I dose-finding and PK study of docetaxel and gefitinib in patients with advanced or metastatic NSCLC to assess the tolerability and the drug–drug interaction of this combination using full PK samplings.
Patients and methods
Patient selection
Patients with histologically or cytologically documented advanced or metastatic NSCLC were eligible for this study regardless of EGFR mutation status. The following eligibility criteria were included: (1) age 20–74 years; (2) ECOG performance status 0–1; (3) life expectancy ≥12 weeks; (4) no previous treatment of with docetaxel or gefitinib; (5) 4 weeks of rest since any previous anticancer therapy; and (6) adequate bone marrow (white blood cell [WBC] count ≥4000/mm3, absolute neutrophil count [ANC] ≥1500/mm3, hemoglobin ≥9.0 g/dL, and platelet count ≥100,000/mm3), renal (creatinine ≤1.5 mg/dL), hepatic (serum total bilirubin ≤1.5 mg/dL, aspartate aminotransferase [AST] ≤100 IU/L, and alanine aminotransferase [ALT ≤100 IU/L), and pulmonary (partial pressure of arterial oxygen ≥70 torr) functions. The exclusion criteria included the following: (1) current or past history of active interstitial pneumonitis; (2) concomitant medications that could strongly affect CYP3A4 metabolism; (3) uncontrolled disease that could confound study results or pose unwarranted risk to the patient; (4) a known history of hypersensitivity to preparations containing polyoxyethylene castor oil; and (5) a history of hepatitis B or C virus or human immunodeficiency virus infections.
Written informed consent was obtained from all patients before enrollment in the study. This study was approved by the institutional review board of the National Cancer Center.
Study design, dosage, and dose escalation
This study was designed to assess the tolerability of the combination of docetaxel and gefitinib in the treatment of advanced or metastatic NSCLC and whether the co-administration of gefitinib with docetaxel could influence the PK and toxicity profiles of docetaxel. The primary objective was to evaluate the tolerability in this combination up to 250 mg/day of gefitinib with 60 mg/m2 of docetaxel (recommended doses for Japanese patients with NSCLC). The secondary objectives were to assess drug–drug interactions by full PK samplings and potential antitumor activities.
The dose of docetaxel was escalated from 45 mg/m2 (Level 1) to 60 mg/m2 (Level 2) in combination with gefitinib (250 mg). The starting docetaxel dose (45 mg/m2) used here was based on a previous phase III study that compared gefitinib with docetaxel as second/third lines of treatment [17]; in the study, if the patients experienced unacceptable toxicities in the initial treatment cycle, the dose was lowered from 60 to 50 mg/m2 in the subsequent cycle of treatment. At least three patients were entered at Level 1. Three additional patients were entered at the same dose if a dose-limiting toxicity (DLT) was observed in one of the initial three patients. DLT was defined as: (1) grade 4 leukopenia or neutropenia ≥5 days; (2) grade 4 thrombocytopenia; (3) grade 4 anemia; (4) febrile neutropenia; (5) grade 3 or 4 non-hematological toxicities except for anorexia, nausea, vomiting, and alopecia; and (6) uncontrollable grade 3 or grade 4 anorexia, nausea, and vomiting despite adequate supportive treatment. If DLT was observed in less than three of the six patients at Level 1, dose escalation was allowed. The DLTs were evaluated in the initial cycle of treatment; however, the tolerability of this combination was determined up to the second cycle of treatment. In Level 2, six patients were planned to enroll in this study. If DLT was observed in less than three of the six patients at Level 2, this dose level was determined as tolerable. Intra-patient dose escalation was not allowed.
Pretreatment and follow-up evaluation
On enrollment in the study, a history and physical examination were performed, and complete differential blood cell count (including WBC count, ANC, hemoglobin, and platelets) and clinical chemistry analysis (including serum total protein, albumin [ALB], bilirubin, creatinine, AST, ALT, alkaline phosphatase [ALP], and alpha-1 acid glycoprotein [AAG]) were performed. Blood cell counts and chemistry analysis except for AAG were performed at least once per week throughout the study. Toxicity was evaluated according to the National Cancer Institute Common Toxicity Criteria (version 2.0), and the antitumor activity was evaluated every two cycles according to the Response Evaluation Criteria in Solid Tumors [18].
Treatment
Docetaxel (Taxotere, Sanofi K.K., Tokyo, Japan) and gefitinib (Iressa, AstraZeneca K.K., Osaka, Japan) were obtained commercially. Docetaxel was diluted in 250 mL of 5 % glucose or 0.9 % saline and administered by 1-h intravenous infusion. To reduce hypersensitivity reaction and emesis from docetaxel, a 5-HT3 receptor antagonist, a histamine 1 blocker, and dexamethasone were prophylactically administered as premedication.
In the initial cycle of treatment, docetaxel was administered on day 1, and gefitinib was administered orally from day 2 (Fig. 1). In the second cycle of treatment, docetaxel and gefitinib were administered on the same day. Treatment with docetaxel was repeated every 3 weeks, and gefitinib was administered once daily from day 2.
PK analysis
To assess the drug–drug interaction between docetaxel and gefitinib, we performed the full PK samplings. Blood samples were drawn just before beginning docetaxel infusion (0 h) and at 0.5, 1, 1.25, 1.5, 2, 4, 6, 9, and 24 h after the start of the infusion on days 1 and 22 (Fig. 1). Blood was drawn into sodium heparin-containing tubes, which were immediately centrifuged at 0–5°. Plasma samples were separated into cryotubes and stored at −80° until analysis. Plasma concentrations of docetaxel were measured by high-performance liquid chromatography according to previously published methods [19] with a detection limit of 10 ng/mL.
Plasma concentrations of gefitinib were determined by high-performance liquid chromatography based on previously published methods [20] with a detection limit of 20 ng/mL. In the initial cycle of treatment, blood samples of gefitinib were drawn on day 18 ± 3 to ensure steady state gefitinib PK. In the second cycle of treatment, blood samples were drawn on the same day as docetaxel treatment (day 22, Fig. 1) before administration of gefitinib (0 h) and at 1, 2, 3, 6, 9, and 24 h after administration.
The docetaxel and gefitinib PK profile were estimated by non-compartmental analysis. A weight of 1/y was used for fitting the terminal log-linear portion of the plasma concentration versus time curve to obtain the first-order terminal rate constant. All PK analyses were performed in WinNonlin (version 6.3, Pharsight Corp as part of Certara G.K., Tokyo, Japan).
Analysis of variance was performed on AUC0–24 and C max to estimate the adjusted mean differences between days 1 and 22. The docetaxel clearance, geometric mean (GM) of AUC0–24 and C max, adjusted GM ratio (GMR, i.e., the ratio of docetaxel AUC0–24 and C max on day 22 to that on day 1), and 90 % confidence intervals (CIs) of the GMR were also calculated. If the 90 % CI in GMR of AUC0–24 and C max converged within the range 0.80–1.25, no evidence of drug–drug interaction could be confirmed in the bioequivalent study [21, 22].
Results
Patient characteristics
Between September 2004 and February 2007, 12 patients were enrolled in the study, and the pretreatment characteristics of the 12 patients are listed in Table 1. The median age was 60 (range 32–72) years, and all 12 patients had ECOG performance status of 1. Although 11 of the 12 patients were diagnosed with adenocarcinoma, the status of EGFR mutation was not determined before enrollment. No patients had liver metastasis, and all 12 patients had good hepatic functions. The first six patients were enrolled in dose Level 1 (docetaxel: 45 mg/m2, gefitinib: 250 mg/day), and the next six patients were enrolled in dose Level 2 (docetaxel: 60 mg/m2, gefitinib: 250 mg/day).
Treatment and evaluation of tolerability
All 12 patients received 46 cycles (median 4, range 1–6, calculated as the number of docetaxel treatment cycles) of treatment and were assessable for safety profiles. The major adverse events are listed in Table 2. The major toxicities were neutropenia, leukopenia, and hepatic dysfunctions. At Level 1, two patients had DLTs in the initial cycle of treatment: one (patient 2, Table 1) had grade 3 febrile neutropenia, grade 3 stomatitis, and grade 3 AST and ALT increase, and the other (patient 4, Table 1) had grade 3 febrile neutropenia and grade 3 fatigue. These two patients were determined unacceptable for this combination treatment and withdrawn from the second cycle. Although two of the six patients had DLTs at Level 1, we determined this dose level to be acceptable according to the dose escalation procedure described in the study protocol and escalated to dose Level 2.
At Level 2, two patients (patients 8 and 10, Table 1) had grade 3 hepatic dysfunctions with grade 3 ALT increase just before the third cycle of treatment. One patient delayed the third cycle of treatment, and the other withdrew from the subsequent cycle of treatment because anti-tumor response was not observed. Although two patients had grade 3 hepatic dysfunction, these toxicities were observed just before the third cycle of treatment and may be solely due to gefitinib. We did not define these hepatic dysfunctions as DLTs from combination treatment and confirmed the tolerability of 60 mg/m2 docetaxel and 250 mg/day gefitinib in combination.
Docetaxel PK
Docetaxel PK data were obtained from 12 to 10 patients in the initial and second cycles of treatment, respectively, because two Level 1 patients withdrew from the second cycle of treatment due to dose-limiting febrile neutropenia. The plasma concentration–time profiles of docetaxel were biphasic decrement curves with mean alpha and beta half-lives of 1.01 min and 0.58 h, respectively. The docetaxel CL showed no difference between doses (45 or 60 mg/m2) or administration schedule (alone or with gefitinib) and was 57 ± 19 L/h (mean ± standard deviation [SD]) with a 33 % coefficient of variation. The docetaxel PK parameters administered alone and with gefitinib are summarized in Table 3. The PK profiles of docetaxel obtained in this study were consistent with a previous Japanese phase I study [23]. At Level 1, the GM AUC0–24 values (mean ± SD) were 1128 ± 287 and 1185 ± 322 ng*h/mL for docetaxel administered alone or with gefitinib, respectively, while those at Level 2 were 1827 ± 321 and 1631 ± 270 ng*h/mL, respectively.
Gefitinib PK
As for docetaxel, gefitinib PK data were obtained from 12 to 10 patients in the initial and second cycles of treatment, respectively. The steady state plasma concentration–time profiles following multiple doses of gefitinib were similar to a previous phase I study [24]. The CLs were 32.8 ± 13.2 and 35.2 ± 12.4 mL/h (mean ± SD) for gefitinib administered alone and with docetaxel, respectively (Table 3), and showed no difference between the two docetaxel dose levels. The AUC0–24 GM values at steady state for gefitinib administered alone and with docetaxel were 7611 ± 3663 and 7107 ± 2745 ng*h/mL (mean ± SD), respectively.
Evaluation of drug–drug interaction
Docetaxel PK parameters did not differ whether administered alone or with gefitinib. The GMRs of the docetaxel AUC0–24 were 1.05 (90 % CI 0.86–1.24) and 0.89 (90 % CI 0.78–1.00) at Level 1 and Level 2, respectively, and those of C max were 0.93 (90 % CI 0.70–1.16) and 0.96 (90 % CI 0.87–1.05), respectively (Table 3). For all evaluable patients (n = 10), the overall GMRs of docetaxel AUC0–24 and C max were 0.95 (90 % CI 0.85–1.06) and 0.95 (90 % CI 0.85–1.05), respectively (Fig. 2a). Furthermore, the GMRs of the steady state gefitinib AUC0–24 and C max were 0.93 (90 % CI 0.84–1.03) and 0.98 (90 % CI 0.88–1.09) when administered alone and with docetaxel, respectively (Table 3; Fig. 2b).
The changes of the docetaxel and gefitinib AUC0–24 and C max values for each patient are illustrated in Fig. 3. Although the steady state gefitinib AUC0–24 and C max decreased in one patient administered with docetaxel (Fig. 3c, d), the AUC0–24 and C max values of docetaxel and steady state gefitinib did not differ whether administered alone and in combination (Fig. 3a, b). These results provided no evidence of drug–drug interaction between docetaxel and gefitinib administered in combination.
Discussion
This study was designed to assess the tolerability of the combination of docetaxel and gefitinib in treatment for advanced or metastatic NSCLC. We confirmed the tolerability of 60 mg/m2 docetaxel and 250 mg/day gefitinib in combination and observed no evidence of drug–drug interaction between docetaxel and gefitinib.
Docetaxel and gefitinib play key roles in the treatment of NSCLC and are metabolized by CYP3A4. CYP3A4 is abundant in human liver microsomes and plays an important role in the metabolism of many drugs, including anticancer drugs. Furthermore, CYP3A4 shows about five- to tenfold inter-patient variability [25–27] in the disposition of these drugs metabolic efficiency, and intra-patient variability is widely recognized for several major inducers [28, 29] or inhibitors [30, 31].
The major concern in this combination study was the effect on docetaxel PK profiles from co-administration with gefitinib because the docetaxel AUC is a strong and independent predictor of neutropenia [7]. The PK profiles of these two anticancer drugs change when co-administered with typical CYP3A4 inhibitors (ketoconazole or itraconazole): The docetaxel CL decreased 49 % when co-administered with ketoconazole [15], and the gefitinib AUC0–24 increased 78 % when co-administered with itraconazole [16]. A previous pilot study reported drug–drug interaction between docetaxel and gefitinib in 18 patients with NSCLC, demonstrating 87 and 100 % increases in the GM AUC0–24 and C max of docetaxel, respectively, in two of ten pharmacokinetically evaluable patients [32]. Although this report suggested a drug–drug interaction between docetaxel and gefitinib, the small number of patients and sparse PK sampling points were inconclusive. We therefore investigated the existence of a drug–drug interaction between docetaxel and gefitinib using full PK samplings.
To evaluate any drug–drug interaction, we assessed the GMRs of the docetaxel and gefitinib AUC0–24 and C max when administered alone or in combination. Convergence of the 90 % CI of the GMR within the range 0.80–1.25 indicates the absence of drug–drug interactions, as established previously [22]. In our study, the 90 % CI of the GMRs of docetaxel and gefitinib AUC0-24 and C max ranged between 0.8 and 1.25 (Fig. 2). The gefitinib AUC0–24 and C max decreased in one patient when co-administered with docetaxel (Fig. 3c, d); however, we could not identify any potential pretreatment factors contributing to this change including body weight and bone marrow, hepatic, and renal functions.
The recommended dose of docetaxel for Japanese patients with NSCLC was 60 mg/m2 at the time of this study, which is still used in routine clinical practice; however, the recommended dose has been updated to 70–75 mg/m2 considering further global trials, and the higher dose is now administered as necessary. To further develop the combination of docetaxel and gefitinib, the tolerability of the dose of 70–75 mg/m2 docetaxel with gefitinib must be evaluated with PK samplings. Two of the six patients had DLTs in the initial cycle of treatment at Level 1, and the mean docetaxel AUC0–24 in these two patients was higher than that for the remaining four patients (2114 vs. 1159 ng*h/mL, respectively). In this study, we did not allow any concomitant medications that could influence CYP3A4 metabolism. Similar high docetaxel AUC0–24 values were reported in previous studies [33, 34], and the high values observed herein may be caused by docetaxel administration alone because these DLTs occurred in the initial cycle of treatment. Patients with impaired hepatic dysfunctions or massive liver metastasis were not enrolled in this study; however, evaluation of the drug–drug interaction in these populations could be of further interest.
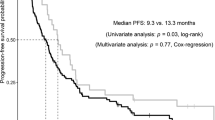
Although 5 of the 12 (41.7 %) patients achieved partial response as assessed by the Response Evaluation Criteria in Solid Tumors [18], we could not determine the efficacy of this combination because the number of evaluated patients was small and the EGFR mutation status was not considered at the time of this study [13, 35–37]. However, we remain interested in this combination because docetaxel and gefitinib are active for NSCLC, and further investigation of this combination for EGFR-mutant NSCLC is warranted.
In conclusion, the tolerability of 60 mg/m2 docetaxel and 250 mg/day gefitinib was confirmed in the treatment for advanced or metastatic NSCLC. To our knowledge, this study is the first analysis of drug–drug interactions in this combination using full PK samplings. Although we observed no drug–drug interaction, the potential interactions of anticancer drugs must be carefully considered, especially when they share a common metabolizing pathway, have narrow therapeutic or toxicity profiles, or are administered to patients with impaired organ functions.
References
Ferlay J, Soerjomataram I, Ervik M et al (2013) GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide: IARC cancer base no. 11. http://globocan.iarc.fr. Accessed 4 Jan 2015
Ohe Y, Ohashi Y, Kubota K et al (2007) Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: four-arm cooperative study in Japan. Ann Oncol 18:317–323
Hanna N, Shepherd FA, Fossella FV et al (2004) Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated with chemotherapy. J Clin Oncol 22:1589–1597
Shepherd FA, Dancey J, Ramlau R et al (2000) Prospective randomized trial of docetaxel versus best supportive care in patients with non-small-cell lung cancer previously treated with platinum-based chemotherapy. J Clin Oncol 18:2095–2103
Fossella FV, Devore R, Kerr RN et al (2000) Randomized phase III trial of docetaxel versus vinorelbine or ifosfamide in patients with advanced non-small-cell lung cancer previously treated with platinum-containing chemotherapy regimens. The TAX 320 non-small cell lung cancer study group. J Clin Oncol 18:2354–2362
Cortes JE, Pazdur R (1995) Docetaxel. J Clin Oncol 13:2643–2655
Extra JM, Rousseau F, Bruno R, Clavel M, Le Bail N, Marty M (1993) Phase I and pharmacokinetic study of Taxotere (RP 56976; NSC 628503) given as a short intravenous infusion. Cancer Res 53:1037–1042
Bruno R, Hille D, Riva A et al (1998) Population pharmacokinetics/pharmacodynamics of docetaxel in phase II studies in patients with cancer. J Clin Oncol 16:187–196
Clarke SJ, Rivory LP (1999) Clinical pharmacokinetics of docetaxel. Clin Pharmacokinet 36:99–114
Gridelli C, De Marinis F, Di Maio M, Cortinovis D, Cappuzzo F, Mok T (2011) Gefitinib as first-line treatment for patients with advanced non-small-cell lung cancer with activating epidermal growth factor receptor mutation: review of the evidence. Lung Cancer 71:249–257
Fukuoka M, Yano S, Giaccone G et al (2003) Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial) [corrected]. J Clin Oncol 21:2237–2246
Kris MG, Natale RB, Herbst RS et al (2003) Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 290:2149–2158
Inoue A, Kobayashi K, Maemondo M et al (2013) Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 24:54–59
Mitsudomi T, Morita S, Yatabe Y et al (2010) Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 11:121–128
Engels FK, Ten Tije AJ, Baker SD et al (2004) Effect of cytochrome P450 3A4 inhibition on the pharmacokinetics of docetaxel. Clin Pharmacol Ther 75:448–454
Swaisland HC, Ranson M, Smith RP et al (2005) Pharmacokinetic drug interactions of gefitinib with rifampicin, itraconazole and metoprolol. Clin Pharmacokinet 44:1067–1081
Maruyama R, Nishiwaki Y, Tamura T et al (2008) Phase III study, V-15-32, of gefitinib versus docetaxel in previously treated Japanese patients with non-small-cell lung cancer. J Clin Oncol 26:4244–4252
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Andersen A, Warren DJ, Brunsvig PF, Aamdal S, Kristensen GB, Olsen H (2006) High sensitivity assays for docetaxel and paclitaxel in plasma using solid-phase extraction and high-performance liquid chromatography with UV detection. BMC Clin Pharmacol 6:2
Faivre L, Gomo C, Mir O et al (2011) A simple HPLC-UV method for the simultaneous quantification of gefitinib and erlotinib in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci 879:2345–2350
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) (2003) Guidance for industry: Bioavailability and bioequivalence studies for orally administered drug products—General considerations. http://www.fda.gov/downloads/Drugs/Guidances/ucm070124.pdf. Accessed 4 Jan 2015
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) (2012) Guidance for industry: Drug interaction studies—Study design, data analysis, implications for dosing, and labeling recommendations. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm292362.pdf. Accessed 4 Jan 2015
Taguchi T, Furue H, Niitani H et al (1994) Phase I clinical trial of RP 56976 (docetaxel) a new anticancer drug. Gan To Kagaku Ryoho 21:1997–2005
Ranson M, Hammond LA, Ferry D et al (2002) ZD1839, a selective oral epidermal growth factor receptor-tyrosine kinase inhibitor, is well tolerated and active in patients with solid, malignant tumors: results of a phase I trial. J Clin Oncol 20:2240–2250
Guengerich FP (1989) Characterization of human microsomal cytochrome P-450 enzymes. Annu Rev Pharmacol Toxicol 29:241–264
Guengerich FP, Turvy CG (1991) Comparison of levels of several human microsomal cytochrome P-450 enzymes and epoxide hydrolase in normal and disease states using immunochemical analysis of surgical liver samples. J Pharmacol Exp Ther 256:1189–1194
Hunt CM, Westerkam WR, Stave GM (1992) Effects of age and gender on the activity of human hepatic CYP3A. Biochem Pharmacol 44:275–283
Kolars JC, Schmiedlin-Ren P, Schuetz JD, Fang C, Watkins PB (1992) Identification of rifampin-inducible P450IIIA4 (CYP3A4) in human small bowel enterocytes. J Clin Invest 90:1871–1878
Mahatthanatrakul W, Nontaput T, Ridtitid W, Wongnawa M, Sunbhanich M (2007) Rifampin, a cytochrome P450 3A inducer, decreases plasma concentrations of antipsychotic risperidone in healthy volunteers. J Clin Pharm Ther 32:161–167
Tan AR, Gibbon DG, Stein MN et al (2013) Effects of ketoconazole and esomeprazole on the pharmacokinetics of pazopanib in patients with solid tumors. Cancer Chemother Pharmacol 71:1635–1643
Mahatthanatrakul W, Sriwiriyajan S, Ridtitid W et al (2012) Effect of cytochrome P450 3A4 inhibitor ketoconazole on risperidone in healthy volunteers. J Clin Pharm Ther 37:221–225
Manegold C, Gatzemeier U, Buchholz E, Smith RP, Fandi A (2005) A pilot trial of gefitinib in combination with docetaxel in patients with locally advanced or metastatic non-small-cell lung cancer. Clin Lung Cancer 6:343–349
Yamamoto N, Tamura T, Kamiya Y, Sekine I, Kunitoh H, Saijo N (2000) Correlation between docetaxel clearance and estimated cytochrome P450 activity by urinary metabolite of exogenous cortisol. J Clin Oncol 18:2301–2308
Yamamoto N, Tamura T, Murakami H et al (2005) Randomized pharmacokinetic and pharmacodynamic study of docetaxel: dosing based on body-surface area compared with individualized dosing based on cytochrome P450 activity estimated using a urinary metabolite of exogenous cortisol. J Clin Oncol 23:1061–1069
Lynch TJ, Bell DW, Sordella R et al (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350:2129–2139
Paez JG, Janne PA, Lee JC et al (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304:1497–1500
Maemondo M, Inoue A, Kobayashi K et al (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362:2380–2388
Acknowledgments
This study was supported by the Japanese Foundation for Multidisciplinary Treatment of Cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest. This manuscript has not been submitted or published and is not under consideration for publication elsewhere. Authorship/disclosure form provided by the authors is available with the full text of this manuscript.
Rights and permissions
About this article
Cite this article
Motonaga, M., Yamamoto, N., Makino, Y. et al. Phase I dose-finding and pharmacokinetic study of docetaxel and gefitinib in patients with advanced or metastatic non-small-cell lung cancer: evaluation of drug–drug interaction. Cancer Chemother Pharmacol 76, 713–721 (2015). https://doi.org/10.1007/s00280-015-2837-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2837-1