Abstract
Response to BH3 mimetics in multiple myeloma (MM) correlates with CCND1-rearrangement or expression of anti-apoptotic molecules, particularly Bcl-2 and Mcl-1. Our study investigates the relationship between cytogenetic abnormalities (CGAs) and intracellular Bcl-2 and Mcl-1 expression in myeloma plasma cells (MPCs) using flow cytometry (FCM). We measured median fluorescence intensity (MFI) of Bcl-2 and Mcl-1 in 163 bone marrow samples (143 MM, 20 controls) across various cell types. Both Bcl-2MFI and Mcl-1MFI were significantly higher in MPCs compared to other cells, with Bcl-2 MFI exceeding Mcl-1 MFI in MPCs. Bcl-2 expression peaked in CCND1-rearranged cases, while Mcl-1 expression was highest in cases with 1q21 gain/amplification. Notably, 65–74% of cases with other CGAs exhibited moderate to strong Bcl-2 or Mcl-1 expression, indicating potential utility of BH3 mimetics in this group, while 25% showed dim to absent expression of one or both markers, suggesting potential futility in these patients. Our study highlights FCM’s potential for rapid Bcl-2 and Mcl-1 quantification, surpassing traditional methods. We propose that direct measurement of Bcl-2 and Mcl-1 expression in PCs by FCM, combined with cytogenetic characterization, could improve therapeutic decision-making regarding the use of BH3 mimetics in MM, potentially enhancing outcomes and overcoming resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is a malignancy of terminally differentiated plasma cells (PC) and is associated with a complex genetic landscape [1] that determines response or resistance to therapy and outcomes. Clonal plasma cells (CPCs) are associated with an upregulation of anti-apoptotic proteins, leading to increased resistance to the intrinsic pathway of apoptosis at the time of diagnosis or during relapse [2]. The key anti-apoptotic members are Bcl-2, Mcl-1, Bcl-XL, Bcl-B, and Bcl-W, which sequester pro-apoptotic BH3-only proteins, resulting in cell survival. Dysregulation of apoptosis leads to the proliferation of neoplastic cells, with Bcl-2 and Mcl-1 playing significant roles in various studies [3]. These anti-apoptotic proteins show heterogeneous expression in mediating resistance.
Recent studies have focused on newer targets in myeloma cells as part of ongoing efforts to improve outcomes in MM. Among several potential biomarkers, apoptosis regulators, especially Bcl-2 and Mcl-1, have been identified as potential therapeutic targets in MM. Bcl-2 is targetable by BH3 mimetics, which bind to apoptotic proteins and ultimately lead to apoptosis activation. Venetoclax is an oral BH3 mimetic drug that targets only Bcl-2 and is helpful in the management of refractory or relapsed MM with Bcl-2 overexpression. However, co-expression of Bcl-2 with high Mcl-1 can lead to resistance to Venetoclax monotherapy [4]. Venetoclax may only be effective in a subset of patients with relatively high Bcl-2 and low Mcl-1. This opens up the possibility of simultaneously targeting both Mcl-1 and Bcl-2 [5,6,7].
Several studies have shown a relationship between t(11;14) or CCND1 rearrangement and high Bcl-2 overexpression [7,8,9,10]. The presence of CCND1 rearrangement is considered a bio-marker to predict response to Venetoclax or similar therapies. However, it is not clear if all cases with CCND1 rearrangement overexpress Bcl-2. The relationship between other cytogenetic abnormalities and the expression of Bcl-2 and Mcl-1 also needs to be systematically studied. Since cytogenetic abnormalities (CGA) often occur in combinations, their influence on the expression of Bcl-2/Mcl-1 may also vary. These situations suggest the utility of measuring Bcl-2 or Mcl-1 expression directly instead of relying on surrogate cytogenetic markers before starting these targeted therapies.
Previous studies have used BH3 profiling and ex-vivo sensitivity to predict response to therapy or have used immunohistochemistry (IHC), Western blotting, or real-time quantitative PCR (RT-qPCR) to study Bcl-2 and Mcl-1 expression, all of which face challenges during routine use and interpretation. Flow cytometry (FCM) provides a rapid and easily quantifiable method for measuring the expression of Bcl-2 and Mcl-1 in CPCs at diagnosis. We aimed to correlate the intracellular expression of Bcl-2 and Mcl-1 in PCs by FCM with CGA and outcomes.
Methodology
A prospective study was conducted over a period of one and a half years between July 2021 and January 2023. In all cases suspected of MM, samples were collected in EDTA for morphological and FCM studies and in sodium heparin for cytogenetic studies. FCM analysis was performed on the BM sample to evaluate the immunophenotype and clonality of PCs, and further for intracellular Bcl-2 and Mcl-1 expression, as discussed below.
Interphase fluorescence in situ hybridization (iFISH)
iFISH testing was performed on PCs enriched using a CD138-magnetic bead-based cell separation kit [EasySep™ Human CD138 positive selection kit II; Stemcell Technologies Inc, Canada] for deletion 17p13/TP53, t(4;14)(IgH::FGFR3), t(14;16)(IGH::MAF), CCND1 rearrangement, t(14;20)(IGH::MAFB), and 1q21/1p32 (CSK1B/CDKN2C) abnormalities using dual-color FISH probes (XL probes, Metasystems, Germany). At least 100 PCs were counted, and a cut-off of 10% was used for translocations (with both break-apart and dual fusion probes) and 20% for numerical abnormalities when assessing CGA using FISH, according to the European Myeloma Network recommendations [11].
Evaluation of clonality of PCs and further Bcl-2 and Mcl-1 expression by FCM
The EDTA-anticoagulated BM sample was processed within 24 h using the bulk lyse-stain-wash method. The clonality of PCs was tested using two tubes, each with ten antibodies: Tube 1 with CD45, CD38, CD138, CD19, CD200, CD27, CD56, CD81, surface kappa, and surface lambda light chains. Tube 2 with CD45, CD38, CD138, CD19, CD117, CD27, CD56, CD28, cytoplasmic kappa, and cytoplasmic lambda light chains. Samples with CPCs were further tested using two tubes with antibodies against CD45, CD38, CD138, CD19, CD3, anti-Bcl-2, and anti-Mcl-1. The panel used in the assay is summarized in Supplementary Table S1. The cells were first surface-stained with the antibodies mentioned above, except for anti-Bcl-2 and anti-Mcl-1. After surface staining, the cells were permeabilized with the perm solution (FIX & PERM™ Cell Permeabilization Reagents; Invitrogen by ThermoFisher, USA) as per the manufacturer’s protocol. A small quantity of this surface-stained-permeabilized sample was used as a “negative tube”; the rest of the sample was used for intracellular staining with Alexa Fluor® 647 conjugated anti-Bcl-2 Antibody (clone 100; Biolegend, San Diego, California) and PE-conjugated anti-human Mcl-1 antibody (clone LVUBKM; eBioscience™, ThermoFisher, USA). At least 1 million events were acquired using the Navios Ex flow cytometer (Beckman Coulter, USA), and the analysis was performed using Kaluza analysis software version 2.1 (Beckman Coulter, USA).
The PCs were sequentially gated and identified using a combination of CD38, CD138, CD45, and side scatter (SSc). The percentage of Myeloma PCs (MPCs) positive for Bcl-2 and Mcl-1 was determined based on the cut-off established using the “negative tube”. T cells were gated using CD3(positive), B cells were gated based on CD19(positive) and CD138(negative), and neutrophils were gated based on CD45 and SSc after excluding all mononuclear cells, including PCs, B cells, and T cells. The gating strategy is shown in Fig. 1. The expression levels of Bcl-2(Bcl-2MFI) and Mcl-1(Mcl-1MFI) on PCs, T cells, and neutrophils were estimated using median fluorescence intensity (MFI). The ratios of MFI expression of Bcl-2 and Mcl-1 on PCs and T cells (Bcl-2MFIPC/T, Mcl-1MFIPC/T) and their ratios (Bcl-2MFIPC/Mcl-1MFIPC) were also studied.
In addition, the study included 20 control samples, which consisted of lymphoma staging marrows and reactive bone marrows with plasmacytosis, but FCM showed non-clonal plasma cells (NPCs).
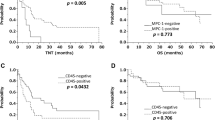
The various Bcl-2 and Mcl-1 parameters (Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T ratio, Mcl-1MFIPC/T ratio, and Bcl-2MFIPC/Mcl-1MFIPC ratios) were compared between MPCs and NPCs and also with iFISH cytogenetics (CG) using the Mann-Whitney U test or Kruskal-Wallis test. The expression levels were also categorized into dim, moderate, and strong, depending on MFI as < 25th percentile, between ≥ 25th and ≤ 50th percentile, and > 50th percentile (of the values in our MM cohort), respectively. Overall survival (OS) and progression-free survival (PFS) were calculated using Kaplan-Meier Survival Curve analysis for cases with dim, moderate, and strong Bcl-2 and Mcl-1 expression levels on MPCs. A two-tailed p-value < 0.05 was considered statistically significant for all tests.
All methods were conducted in accordance with the Declaration of Helsinki, and ethical clearance was obtained from the Institutional Ethics Committee (intramural) vide reference number: INT/IEC/2021/SP71618.
Results
During the study, FCM was performed in 143 BM samples (103 newly diagnosed MM/NDMM cases, 40 relapsed/refractory MM/RRMM cases). The clinical and cytogenetic characteristics at diagnosis of MM cases is summarized in Table 1.
Comparison of Bcl-2MFI and Mcl-1MFI between MPCs, T cells, B cells, and neutrophils in MM samples
Bcl-2MFI (median 43,289; IQR 23,162 − 88,418) was significantly higher in MPCs compared to T cells (median 24,055; IQR 16,924 − 30,763; p < 0.001), B cells (median 20,609; IQR 11,301 − 29,739; p < 0.001), and neutrophils (median 2,405; IQR 1,552-3,467; p < 0.001). Similarly, Mcl-1MFI (median 6,481; IQR 4,050 − 9,998) was significantly higher in MPCs than in T cells (median 1,456; IQR 1,098 − 2,035; p < 0.001), B cells (median 1,247; IQR 942-1,836; p < 0.001), and neutrophils (median 2,755; IQR 2,040 − 3,420; p < 0.001). Median Bcl-2MFI and Mcl-1MFI were lowest in neutrophils and B lymphocytes, respectively (Supplementary Table S2 and Fig. 1).
Flow cytometric analysis showing sequential gating strategy used in the analysis of intracellular Bcl-2 and Mcl-1 expression in plasma cells/PC, T lymphocytes and polymorphs. Bivariate dot plots “a” to “e” demonstrate the initial gating strategy to identify the purified plasma cells (PCs) based on the CD45, CD38, CD138 and side scatter. “f and g”: B and T lymphocytes are identified based on CD45 positive with low side scatter and bright expression of CD19 and CD3, respectively. “h”: Polymorphs are identified by using boolean gate Viable AND (NOT MNCs). In bivariate dot plots “i” and “k” FMO threshold is applied on PCs unstained for Bcl-2 and Mcl-1. Dot plots “j” and “l” show expression of Bcl-2 and Mcl-1 on PCs based on FMO applied on unstained PCs. Histograms “m” to “r” represent median fluorescence intensity (MFI) of expression of Bcl-2 and Mcl-1 on PCs, T-cells, and polymorphs, respectively. MNC-mononuclear cells, FMO-fluorescence minus one, PC-plasma cells
Comparison of Bcl-2MFI versus Mcl-1MFI in PCs in MM samples
A median of 6.05 × 10^5 events (IQR: 3.04 × 10^5 to 12.6 × 10^5) were acquired. The percentage of CPCs among all viable cells, as measured by FCM, ranged from 0.06 to 89.8% (median: 9.13%; IQR: 3.4-24.1%). The median percentage of MPCs expressing Bcl-2 and Mcl-1 was 96.9% (IQR: 89.6-99.1%) and 78.8% (IQR: 33-96%), respectively. Additionally, more than 90% of MPCs expressed Bcl-2 in 74% (n = 106) of cases and Mcl-1 in 39.2% (n = 56) of cases. The median (IQR) of Bcl-2 MFI and Mcl-1 MFI in MPCs was 43,289 (23,162 − 88,418) and 6,481 (4,050 − 9,998), respectively. Bcl-2 MFI was significantly higher than Mcl-1 MFI (p < 0.001) in MPCs.
Comparison of Bcl-2MFI and Mcl-1MFI, and various ratios between control samples and MM samples
Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T, Mcl-1MFIPC/T, and Bcl-2MFIPC/Mcl-1 MFIPC were compared between MPCs in MM samples and NPC in controls. Bcl-2MFI (median: 43,289 vs. 22,355; p = 0.011), Bcl-2MFIPC/T (1.9 vs. 0.9; p = 0.002), Mcl-1MFIPC/T (4.3 vs. 3; p = 0.002), and Bcl-2MFIPC/Mcl-1MFIPC (7.1 vs. 3.2; p = 0.010) were significantly higher in MPCs compared to NPCs. However, there was no statistically significant difference in Mcl-1MFI between MPCs and NPCs (median: 6,481 vs. 6,273; p = 0.829). Overall, Bcl-2 and Mcl-1 expression was significantly higher in MPCs than in NPCs, and the ratio of Bcl-2 to Mcl-1 expression (Bcl-2MFIPC/Mcl-1MFIPC) was also significantly different in MPCs compared to NPCs (Supplementary Table S3 and Fig. 2, plot a-e).
Box and Whisker plots comparing the Bcl-2MFI PC, Mcl-1MFI PC, Bcl-2MFIPC/T, Mcl-1MFI1PC/T, Bcl-2MFIPC/Mcl-1MFIPC among various categories. Plots “a” to “e” compare Bcl-2MFI PC, Mcl-1MFI PC, Bcl-2MFIPC/T, Mcl-1MFI1PC/T, Bcl-2MFIPC/Mcl-1MFIPC in myeloma PCs/MPCs in MM cases and non-clonal PCs/NPC in control cases. Plots “f” to “j” shows impact of isolated cytogenetic abnormalities (FGFR3-r, MAF-r, CCND1-r, delTP53, gain1q21, 1q21amp and del1p32) on Bcl-2MFI PC, Mcl-1MFI PC and various ratios. Plots “k” to “o” compare the Bcl-2MFI PC, Mcl-1MFI PC, Bcl-2MFIPC/T, Mcl-1MFI1PC/T, Bcl-2MFIPC/Mcl-1MFIPC in MPCs in cases with and without CCND1-r. Plots “p” to “t” compare these parameters in cases with and without gain1q21
Comparison of Bcl-2MFI and Mcl-1MFI, and various ratios between NDMM and RRMM cases
Bcl-2MFI (median 43,711 vs. 42,699; p = 0.51), Mcl-1MFI (median 6,542 vs. 6,450; p = 0.84), Bcl-2MFIPC/T (1.9 vs. 2.1; p = 0.68), Mcl-1MFIPC/T (4.2 vs. 4.4; p = 0.96), and Bcl-2MFIPC/Mcl-1MFIPC (7.9 vs. 5.2; p = 0.27) did not show significant differences between NDMM and RRMM cases.
Impact of isolated CG abnormalities on Bcl-2MFI, Mcl-1MFI, and various ratios
We studied the frequencies of CCND1-rearrangement (CCND1-r), IGH::FGFR3 (FGFR3-r), IGH::MAF (MAF-r), gain1q21, del1p32, and delTP53 occurring as isolated CGA or in combinations. Patients had zero, one, two, and three CG abnormalities in 40 (29.97%), 59 (41.25%), 37 (25.87%), and 7 (4.89%) cases (Supplementary Table S4). First, we restricted the analysis to cases with a single CG change to eliminate the influence of multiple CG abnormalities.
We had only one case with isolated MAF-r, and PCs in that case showed very high values for Bcl-2MFI (132,699), Bcl-2MFIPC/T (5.3), and Bcl-2MFIPC/Mcl-1MFIPC (63.5); and very low Mcl-1MFI (2,088).
After isolated MAF-r, cases with isolated CCND1-r (n = 4) had the highest median values for Bcl-2MFI (50,117), Bcl-2MFIPC/T (2.5), and Bcl-2MFIPC/Mcl-1MFIPC (9.8); while cases with isolated FGFR3-r (n = 5) had the lowest values for Bcl-2MFI (19,307), Bcl-2MFIPC/T (0.8), and also showed a lower Bcl-2MFIPC/Mcl-1MFIPC (5.9). MPCs with only gain1q21 (n = 41) had the highest Mcl-1MFI (6,462) and Mcl-1MFIPC/T (4.4), and the lowest Bcl-2MFIPC/Mcl-1MFIPC (5.3). The cases without any of the six mentioned CG changes had values comparable to those with CCND1-r: Bcl-2MFI (56,633), Bcl-2MFIPC/T (2.4), and Bcl-2 MFIPC/Mcl-1MFIPC (9.6).
Thus, after excluding a single case with MAF-r, Bcl-2 expression was highest in CCND1-r, lowest in FGFR3-r, while Mcl-1 expression was highest in isolated gain1q21 (Supplementary Table S5 and Fig. 2, plot f-j).
Impact of the association of gain1q21 with CCND1-r and FGFR3-r
We studied the impact of the association of gain1q21, a secondary CG abnormality, with a standard (CCND1-r) and a high-risk CG abnormality (FGFR3-r). FGFR3-r with gain1q21 was seen in 21 cases (Out of 21 cases, three cases each also showed either delTP53 or del1p32). Bcl-2MFI (median 88,418 vs. 21,752; p = 0.024), Mcl-1MFI (median 10,223 vs. 4,499; p = 0.005), Bcl-2MFIPC/T (2.6 vs. 1.2; p = 0.028), and Mcl-1MFIPC/T (5 vs. 3.6; p = 0.013) showed significantly higher values in MPCs from cases with FGFR3-r plus gain1q21 (n = 21) compared to MPCs in FGFR3-r cases without gain1q21 (n = 8). Bcl-2MFIPC/Mcl-1MFIPC (8 vs. 6.2; p = 0.626) was also higher in FGFR3-r plus gain1q21 cases (Supplementary Table S6). Thus, FGFR3-r cases with associated gain1q21, have significantly higher expression of Bcl-2 and Mcl-1 than FGFR3-r cases without associated gain1q21. CCND1-r with gain 1q21 was seen in 3 cases (1 case also showed additional delTP53). However, none of the MFI parameters showed significant differences between MPCs of cases with CCND1-r with (n = 3) or without gain1q21 (n = 5) (Supplementary Table S7).
Overall impact of CG abnormalities on Bcl-2MFI and Mcl-1MFI and various ratios
Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T, Mcl-1MFIPC/T, and Bcl-2MFIPC/Mcl-1MFIPC were compared in cases without or with CGA irrespective of presence or absence of other associated abnormalities [CCND1-r (n = 8), FGFR3-r (n = 29), MAF-r (n = 3), gain1q21 (n = 76), del1p32 (n = 17), and delTP53 (n = 21)]. Bcl-2MFI (median-56,312 vs. 42,909) and Bcl-2MFIPC/T (3.1 vs. 1.9) were higher in patients with CCND1-r (versus all other CGA) though they did not show statistical significance. Mcl-1MFI (median-3,826 vs. 6,559; p = 0.020) and Mcl-1MFIPC/T (2.2 vs. 4.4; p < 0.001) were significantly lower, while Bcl-2MFIPC/Mcl-1MFIPC was significantly higher (11.9 vs. 6.8; p = 0.012) in MPCs with CCND1-r (versus all other CGA) (Fig. 2, plot k-o). Overall, the Bcl-2/Mcl-1 ratio remained higher in cases with CCND1-rirrespective of influence by other CG abnormalities.
MPCs with gain1q21 (versus all other CGA) showed significantly higher Mcl-1MFI (median-7,385 vs. 5,980; p = 0.04) compared to MPCs without gain1q21. Mcl-1MFIPC/T (4.5 vs. 3.8; p = 0.067) was higher, and Bcl-2MFIPC/Mcl-1MFIPC (5.7 vs. 8.5; p = 0.077) was lower in MPCs with gain1q21 though the difference was not significantly different. Mcl-1MFIPC/T was significantly high in MPCs with amplification of 1q21 (≥ 3 copies) (5.3 vs. 4.2; p = 0.008) (Fig. 2,plot p-t). These findings are consistent with a significantly high expression of Mcl-1 in MPCs with gain1q21/1q21 amplification. None of the MFI parameters showed significant differences between MPCs with or without FGFR3-r, MAF-r, delTP53, or del1p32 (Supplementary Table S8).
Dim, moderate, and strong expression of Bcl-2 or Mcl-1 and correlation with CG abnormalities
Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T, Mcl-1MFIPC/T, and Bcl-2MFIPC/Mcl-1MFIPC were categorized into dim, moderate, and strong, depending on MFI as < 25th percentile, between ≥ 25th and ≤ 50th percentile, and > 50th percentile, respectively in our study group. Irrespective of the parameter, 25% (n = 36) of cases showed dim Bcl-2 or Mcl-1 expression. 25% (n = 36 for Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T, and Bcl-2MFIPC/Mcl-1MFIPC, n = 37 for Mcl-1MFIPC/T) showed moderate Bcl-2 or Mcl-1 expression and rest 50% cases showed strong expression. Both dim and moderate Bcl-2 or Mcl-1 expression was seen in 25% (n = 36) cases each and rest 50% of cases showed strong expression.
Bcl-2 MFIPC/T was moderate to strong in 100% of cases with MAF-r and CCND1-r. It was moderate to strong in 75%, 69%, 66.7%, and 52.9% of cases with gain1q21, FGFR3-r, delTP53, and del1p32, respectively. Mcl-1MFIPC/T was moderate to strong in 100% of MAF-r cases and 82.4% of del1p32 cases. It was moderate to strong in 85.8%, 82.8%, 76.3%, and 25% of cases with delTP53, FGFR3-r, gain1q21, and CCND1-r, respectively (Supplementary Table S9). Considering Bcl-2 MFIPC/Mcl-1MFIPC, a moderate to strong Bcl-2 expression relative to Mcl-1 was seen in 100% of CCND1-r cases and 73.7%, 72.4%, 66.7%, 66.7%, and 64.7% of cases with gain1q21, FGFR3-r, MAF-r, delTP53, and del1p32, respectively. None of the patients in our series received Venetoclax, as it is still not an approved therapy for upfront or relapsed MM; hence, a correlation with response to Bcl-2 inhibitors was beyond the current study’s scope.
Impact of stage of MM on Bcl-2MFI and Mcl-1MFI and various ratios
The stage (as per the second revision of International Staging System/R2-ISS) [12] was known in 94/103 NDMM cases and were stages I, II, III, and IV in 2, 4, 51, and 37 cases respectively. Bcl-2 MFI and MCL-1 MFI and ratios were compared between Stage I + II vs. III + IV using the Mann-Whitney U test. Median Bcl-2 MFI (44990 vs. 41185, p = 0.60), Mcl-1 MFI (6411 vs. 6371, p = 0.84), Bcl-2 MFIPC/T (1.9 vs. 1.7, p = 0.60), Mcl-1MFIPC/T (4.3 vs. 3.2, p = 0.10) and Bcl-2 MFIPC/Mcl-1MFIPC (7.8 vs. 7.3, p = 0.86) were higher in stage III + IV compared to stage I + II cases, but the differences were not statistically significant. Similarly, there was no significant difference when stage I + II + III was compared with stage IV.
Discussion
Our study aimed to correlate the intracellular expression of Bcl-2 and Mcl-1 by FCM with cytogenetic characteristics in MM. This analysis involved NDMM, RRMM, and control samples, attempting to understand the relationship between these two targetable apoptosis regulators and disease characteristics.
The BELLINI trial demonstrated Venetoclax’s efficacy in RRMM with t(11;14) or high Bcl-2 expression [13], while another study linked its effectiveness to high Bcl-2 and low Bcl-XL or Mcl-1 levels [14]. Venetoclax is preferred for CCND1-r patients, but resistance due to Mcl-1 or Bcl-XL co-expression necessitates combining it with their inhibitors in ongoing studies [4,5,6, 14, 15].
Gupta et al. [16] demonstrated Venetoclax resistance persists after CCND1 knockdown, suggesting t(11;14) and CCND1 aren’t direct response determinants. Flow-based Bcl-2 prediction scores can identify Venetoclax-sensitive cases independently of t(11;14). Nahi et al. [8] and Kumar et al. [10] showed increased BCL2/MCL1 and BCL2/BCL2-XL ratios predict Venetoclax response, with the latter confirming this correlation in t(11;14) patients using mRNA expression ratios.
MM, being heterogeneous in terms of expression of pro and anti-apoptotic markers, is likely to have variable responses to BH3 mimetics. Thus, an objective measurement method is crucial. BH3 profiling or ex vivo Venetoclax sensitivity testing may best predict apoptotic pathway-targeted therapy responses and identify CCND1-r negative MM targetable by BH3 mimetics [17, 18]. Previous studies used IHC, Western Blot, or RT-qPCR [19], each with limitations: IHC is subjective and affected by various factors, Western blot is clinically cumbersome, and RT-qPCR measures mRNA, not protein expression. FCM has been used in chronic lymphocytic leukemia studies [19,20,21] to study apoptotic markers. We thus employed FCM to study intracellular Bcl-2 and Mcl-1 expression, correlating with CGA and focusing on the influence of multiple CGAs.
We analysed Bcl-2 and Mcl-1 expression using five FCM parameters: Bcl-2MFI, Mcl-1MFI, Bcl-2MFIPC/T, Mcl-1MFIPC/T, and Bcl-2MFIPC/Mcl-1MFIPC. The latter three reduce measurement bias and assess relative expression levels of Bcl-2 and Mcl-1 with each other [22]. Bcl-2 and Mcl-1 were significantly higher in PCs but also present in other cell types. Lowest Bcl-2 in neutrophils may explain Venetoclax-induced neutropenia [23].
MPCs showed significantly higher Bcl-2 expression than NPCs, consistent with previous studies [24, 25] and indicate aberrant upregulation of these anti-apoptotic proteins in MM. Though Mcl-1 expression was higher in MPCs (suggested by Mcl-1MFIPC/T) than in NPCs, there was a significant difference in the expression of Bcl-2 vs. Mcl-1 (suggested by Bcl-2MFIPC/Mcl-1MFIPC) in MPCs compared to NPCs, indicating the importance of targeting Bcl-2 over Mcl-1.
No significant differences were found between NDMM and RRMM, contrary to some studies [8, 26]. This discrepancy might be due to CG heterogeneity or late NDMM presentation (as suggested by a high frequency of gain1q21 in 53% of cases) in our cohort.
Bcl-2 and Mcl-1 expression varied across CG groups. When we analyzed cases with single CG abnormalities (among CCND1-r, FGFR3-r, MAF-r, delTP53, gain1q21, and del1p32), a case with MAF-r showed the highest expression of both Bcl-2 and Mcl-1. Apart from that, Bcl-2 expression was highest in CCND1-r, lowest in FGFR3-r, while Mcl-1 expression was highest in gain1q21. Further, among all cases (which will include the combined influence of all CG abnormalities), the Mcl-1 expression remained significantly lower, and Bcl-2 expression relative to Mcl-1 expression (Bcl-2MFIPC/Mcl-1MFIPC ratio) remained significantly higher in cases with CCND1-r. Overall these findings are consistent with the previous report [10].
Bcl-2 expression was highest in CCND1-r and remained so even when associated with other CG changes. A study by Cleynen et al. [27] showed no significant difference in BCL2/ MCL1 ratio in cases with and without t(11;14) but found significantly higher BCL2/ BCL2L1 ratio. However, Interestingly, they highlighted that a high BCL2/BCL2L1 ratio was also frequently seen in a subgroup of non-t(11;14) patients.
Patients with gain and amplification of 1q21 showed significantly higher median Mcl-1MFI and Mcl-1PC/T ratio, explainable by the gain of gain of MCL1 locus mapping to chromosome 1q21 [28]. Previously, Slomp et al. also showed the sensitivity of gain1q21 positive MM cells to Mcl-1 inhibitors [29]. Though FGFR3-r had the lowest Bcl-2 expression, both Bcl-2 and Mcl-1 expression increased significantly with the acquisition of gain1q21. This is probably one of the mechanisms of resistance to therapy in FGFR3-r MM.
A moderate to strong Bcl-2 relative to Mcl-1(indicated by Bcl-2MFIPC/Mcl-1MFIPC ratio) was seen in 100% of CCND1-r and 65–74% of cases with other CG abnormalities indicating potential utility of Bcl-2 inhibitors in these cases as well. At the same time, 25% had a dim Bcl-2MFI or Mcl-1MFI with uncertainty regarding the influence of either Bcl-2 or Mcl-1 inhibitors.
The straightforward and objective implementation of FCM to measure these markers facilitates the study of their expression patterns and their response to Bcl-2 or Mcl-1 targeted therapy in clinical trials. This approach is more reliable than relying solely on CG abnormalities. Such studies enhance our understanding of the utility of these therapies, especially in cases with low or absent expression of Bcl-2 or Mcl-1. Additionally, the MFI of Bcl-2 or Mcl-1 on CPCs, relative to other cells (such as neutrophils), may help guide dosage titration.
However, our study has limitations. The relatively small number of patients in most CG groups restricts a comprehensive exploration of the impact of multiple CG abnormalities on Bcl-2 or Mcl-1 expression. Though our cohort who underwent Bcl-2 and Mcl-1 testing had predominantly CPCs in bone marrow samples, MFI expression was not studied specifically on CPCs due to the lack of other immunophenotypic markers, including cytoplasmic kappa and cytoplasmic lambda, in the same tube. A recent study highlighted poor prognosis in patients with co-occurrence of del(13q) and gain(1q21) [30]. This group was also not studied as we did not test for del(13q) in our cohort. Furthermore, BH3-mimetics were not used in our patients, preventing direct correlation with Bcl-2 or Mcl-1 expression. Despite these limitations, we demonstrate the utility of FCM in objectively measuring Bcl-2 and Mcl-1 expression. While we found the highest expression of Bcl-2 in CCND1-r and Mcl-1 in gain/amplification of 1q21, these findings are not exclusive to those CG abnormalities. Moderate to strong Bcl-2 or Mcl-1 expression is also observed in 65–74% of MM cases with other CG abnormalities and 25% of cases showed dim to absent expression of one or more of these markers.
Our study highlights the potential of measuring Bcl-2 and Mcl-1 expression levels in CPCs and other cells using FCM, providing rapid quantification compared to traditional methods. Combining this approach with cytogenetic characterization could improve therapeutic decisions targeting Bcl-2 and Mcl-1, potentially improving outcomes and overcoming resistance in MM patients.
Data availability
Data shall be shared on request to the corresponding author.
References
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L et al (2015) Revised International Staging System for multiple myeloma: a Report from International Myeloma Working Group. J Clin Oncol off J Am Soc Clin Oncol 33(26):2863–2869
Slomp A, Peperzak V (2018) Role and regulation of pro-survival BCL-2 proteins in multiple myeloma. Front Oncol 8:533
Czabotar PE, Lessene G, Strasser A, Adams JM (2014) Control of apoptosis by the BCL-2 protein family: implications for physiology and therapy. Nat Rev Mol Cell Biol 15(1):49–63
Hanamura I (2021) Gain/Amplification of chromosome arm 1q21 in multiple myeloma. Cancers 13(2):256
Leverson JD, Zhang H, Chen J, Tahir SK, Phillips DC, Xue J et al (2015) Potent and selective small-molecule MCL-1 inhibitors demonstrate on-target cancer cell killing activity as single agents and in combination with ABT-263 (navitoclax). Cell Death Dis 6:e1590
Seiller C, Maiga S, Touzeau C, Bellanger C, Kervoëlen C, Descamps G et al (2020) Dual targeting of BCL2 and MCL1 rescues myeloma cells resistant to BCL2 and MCL1 inhibitors associated with the formation of BAX/BAK hetero-complexes. Cell Death Dis 11(5):1–14
Touzeau C, Dousset C, Le Gouill S, Sampath D, Leverson JD, Souers AJ et al (2014) The Bcl-2 specific BH3 mimetic ABT-199: a promising targeted therapy for t(11;14) multiple myeloma. Leukemia 28(1):210–212
Nahi H, Kashif M, Klimkowska M, Karvouni M, Wallblom A, Gran C et al (2021) Low dose venetoclax as a single agent treatment of plasma cell malignancies harboring t(11;14). Am J Hematol 96(8):925–933
Harrison S, Cavo M, De La Rubia J, Popat R, Gasparetto C, Hungria VTM et al (2019) T(11;14) and high BCL2 expression are predictive biomarkers of response to Venetoclax in Combination with Bortezomib and Dexamethasone in patients with Relapsed/Refractory multiple myeloma: biomarker analyses from the phase 3 Bellini Study. Blood 134(Supplement1):142–142
Kumar S, Kaufman JL, Gasparetto C, Mikhael J, Vij R, Pegourie B et al (2017) Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood 130(22):2401–2409
Ross FM, Avet-Loiseau H, Ameye G, Gutiérrez NC, Liebisch P, O’Connor S et al (2012) Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders. Haematologica 97(8):1272–1277
D’Agostino M, Cairns DA, Lahuerta JJ, Wester R, Bertsch U, Waage A et al (2022) Second revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: a European Myeloma Network (EMN) Report within the HARMONY Project. J Clin Oncol 40(29):3406–3418
Kumar SK, Harrison SJ, Cavo M, Rubia J, de la, Popat R, Gasparetto C et al (2020) Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol 21(12):1630–1642
Punnoose EA, Leverson JD, Peale F, Boghaert ER, Belmont LD, Tan N et al (2016) Expression Profile of BCL-2, BCL-XL, and MCL-1 predicts pharmacological response to the BCL-2 selective antagonist Venetoclax in multiple myeloma models. Mol Cancer Ther 15(5):1132–1144
Flanagan L, Coughlan A, Cosgrove N, Roe A, Wang Y, Gilmore S et al (2024) Steroid-free combination of 5-azacytidine and venetoclax for the treatment of multiple myeloma. Haematologica
Gupta VA, Barwick BG, Matulis SM, Shirasaki R, Jaye DL, Keats JJ et al (2021) Venetoclax sensitivity in multiple myeloma is associated with B-cell gene expression. Blood 137(26):3604–3615
Touzeau C, Ryan J, Guerriero J, Moreau P, Chonghaile TN, Le Gouill S et al (2016) BH3 profiling identifies heterogeneous dependency on Bcl-2 family members in multiple myeloma and predicts sensitivity to BH3 mimetics. Leukemia 30(3):761–764
Matulis SM, Gupta VA, Neri P, Bahlis NJ, Maciag P, Leverson JD et al (2019) Functional profiling of venetoclax sensitivity can predict clinical response in multiple myeloma. Leukemia 33(5):1291–1296
Marschitz I, Tinhofer I, Hittmair A, Egle A, Kos M, Greil R (2000) Analysis of Bcl-2 protein expression in chronic lymphocytic leukemia. A comparison of three semiquantitation techniques. Am J Clin Pathol 113(2):219–229
Menendez P, Vargas A, Bueno C, Barrena S, Almeida J, De Santiago M et al (2004) Quantitative analysis of bcl-2 expression in normal and leukemic human B-cell differentiation. Leukemia 18(3):491–498
Ludwig LM, Maxcy KL, LaBelle JL (2019) Flow Cytometry-based detection and analysis of BCL-2 family proteins and mitochondrial outer membrane permeabilization (MOMP). Methods Mol Biol Clifton NJ 1877:77–91
Gautam A, Sreedharanunni S, Sachdeva MUS, Rana S, Kashyap D, Bose P et al (2021) The relative expression levels of CD148 and CD180 on clonal B cells and CD148/CD180 median fluorescence intensity ratios are useful in the characterization of mature B cell lymphoid neoplasms infiltrating blood and bone marrow - results from a single centre pilot study. Int J Lab Hematol 43(5):1123–1131
Di Pasqua LG, Abdallah MM, Feletti F, Vairetti M, Ferrigno A (2024) Venetoclax-related Neutropenia in Leukemic patients: a Comprehensive Review of the underlying causes, risk factors, and management. Pharm Basel Switz 17(4):484
Miguel-García A, Orero T, Matutes E, Carbonell F, Miguel-Sosa A, Linares M et al (1998) bcl-2 expression in plasma cells from neoplastic gammopathies and reactive plasmacytosis: a comparative study. Haematologica 83(4):298–304
Puthier D, Pellat-Deceunynck C, Barillé S, Robillard N, Rapp MJ, Juge-Morineau N et al (1999) Differential expression of Bcl-2 in human plasma cell disorders according to proliferation status and malignancy. Leukemia 13(2):289–294
Spaan I, van de Stolpe A, Raymakers RA, Peperzak V (2021) Multiple myeloma relapse is Associated with increased NFκB pathway activity and upregulation of the pro-survival BCL-2 protein BFL-1. Cancers 13(18):4668
Cleynen A, Samur M, Perrot A, Buisson L, Maheo S, Fulciniti M et al (2018) Variable BCL2/BCL2L1 ratio in multiple myeloma with t(11;14). Blood 132(26):2778–2780
Craig RW, Jabs EW, Zhou P, Kozopas KM, Hawkins AL, Rochelle JM et al (1994) Human and mouse chromosomal mapping of the myeloid cell leukemia-1 gene: MCL1 maps to human chromosome 1q21, a region that is frequently altered in preneoplastic and neoplastic disease. Genomics 23(2):457–463
Slomp A, Moesbergen LM, Gong J, nan, Cuenca M, von dem Borne PA, Sonneveld P et al (2019) Multiple myeloma with 1q21 amplification is highly sensitive to MCL-1 targeting. Blood Adv 3(24):4202–4214
Terragna C, Poletti A, Solli V, Martello M, Zamagni E, Pantani L et al (2024) Multi-dimensional scaling techniques unveiled gain1q&loss13q co-occurrence in multiple myeloma patients with specific genomic, transcriptional and adverse clinical features. Nat Commun 15(1):1551
Author information
Authors and Affiliations
Contributions
SS and SRE wrote the manuscript. SS performed flow cytometry and analyzed data. SRE designed the study, obtained ethical approval and funding, and analyzed the data. AS, PB, AK, MUSS and NM supervised flow cytometry testing. AB, SRE, and PS performed and analyzed FISH. AJ, AK, GP, RD, MUSS, CS, DL, and PM provided clinical and laboratory data, reviewed it, and gave final approval for the manuscript. All authors agree to the content of the manuscript and its interpretations.
Corresponding author
Ethics declarations
Ethical approval
All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The research was carried out according to the Institutional ethics guidelines after obtaining the approval of the Institute ethics committee.
Informed consent
Written informed consent was obtained from all patients in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The results of the study were partially presented as an abstract in the American Society of Hematology conference in the year 2023.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singla, S., Sreedharanunni, S., Singh, A. et al. Flow cytometric expression of Bcl-2, Mcl-1, and their ratios correlates with primary and secondary cytogenetic changes and their combinations in multiple myeloma. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-06004-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-06004-3