Abstract
Introduction
Lymphoma tissue biopsies cannot fully capture genetic features due to accessibility and heterogeneity. We aimed to assess the applicability of circulating tumor DNA (ctDNA) for genomic profiling and disease surveillance in classic Hodgkin lymphoma (cHL), primary mediastinal large B-cell lymphoma (PMBCL), and diffuse large B-cell lymphoma (DLBCL).
Methods
Tumor tissue and/or liquid biopsies of 49 cHLs, 32 PMBCLs, and 74 DLBCLs were subject to next-generation sequencing targeting 475 genes. The concordance of genetic aberrations in ctDNA and paired tissues was investigated, followed by elevating ctDNA-based mutational landscapes and the correlation between ctDNA dynamics and radiological response/progression.
Results
ctDNA exhibited high concordance with tissue samples in cHL (78%), PMBCL (84%), and DLBCL (78%). In cHL, more unique mutations were detected in ctDNA than in tissue biopsies (P < 0.01), with higher variant allele frequencies (P < 0.01). Distinct genomic features in cHL, PMBCL, and DLBCL, including STAT6, SOCS1, BTG2, and PIM1 alterations, could be captured by ctDNA alone. Prevalent PD-L1/PD-L2 amplifications were associated with more concomitant alterations in PMBCL (P < 0.01). Moreover, ctDNA fluctuation could reflect treatment responses and indicate relapse before imaging diagnosis.
Conclusions
Lymphoma genomic profiling by ctDNA was concordant with that by tumor tissues. ctDNA might also be applied in lymphoma surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymphomas are a heterogeneous group of hematological malignancies that arise from the lymphatic system, including two main types: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) [1]. Classic Hodgkin lymphoma (cHL) is the most prevalent HL subtype, accounting for approximately 95% of HL cases; however, the age-standardized incidence rate of HL is as low as between 2 and 3 per 100,000 persons per year [2, 3]. Primary mediastinal large B-cell lymphoma (PMBCL) is a rare NHL subtype rising from thymic medullary B cells, with incidence rate of 0.04 per 100,000 persons per year [4]. PMBCL accounts for 2–3% of all NHL cases and is more frequently observed in young females [5]. By contrast, diffuse large B-cell lymphoma (DLBCL) is the most prevalent NHL subtype, accounting for 20.0–63.9% of NHL cases, with incidence ranging from 2.3 to 23.8 cases per 100,000 persons per year [6].
PMBCL was initially categorized as a subtype of DLBCL based on clinicopathologic features [7], whereas it is now recognized as a distinct entity and separated from DLBCL by the World Health Organization [8, 9]. Interestingly, recent studies on gene expression profiles have revealed that PMBCL displays shared molecular features with cHL, including activated JAK/STAT [10,11,12,13,14,15], and Nuclear Factor Kappa B (NF-ƙB) pathways [10, 15, 16], as well as PD-L1 and PD-L2 mediated immune evasion [11, 15, 17].
cHL is characterized by the presence of malignant lymphoid cells, called Reed-Sternberg cells, which comprise few malignant cells in HL tissue [18]. While tissue biopsy has traditionally been used to assess the genetic landscape of cHL, a study has highlighted the limited ability of this approach to capture clonal diversity and intra-tumoral heterogeneity [19]. On the other hand, due to the advantage of liquid biopsy, circulating tumor DNA (ctDNA) extract from plasma has shown promise in capturing the genetic profiles of cHL and overcoming the shortage of tissue biopsy. For example, previous studies have demonstrated high concordance between ctDNA and tumor tissue biopsy-based next-generation sequencing (NGS) approaches [20, 21] in cHL. Similarly, ctDNA has also been shown to fully capture the mutational landscape of PMBCL and DLBCL [22,23,24]; however, in previous studies, genetic profile comparison between tumor tissue and plasma samples were based on relatively small NGS panels. The assessment of liquid biopsy applicability in these three types of lymphomas has not been comprehensively investigated using a large NGS panel.
In this study, we retrospectively investigated the mutational profiles of cHL, PMBCL, and DLBCL in a Chinese population using an NGS panel covering 475 hematopoietic and lymphoid neoplasm related genes. By utilizing both tissue and liquid biopsies, we aimed to provide a more comprehensive and accurate picture of the genomic landscape of these lymphomas and facilitate disease diagnosis and classification.
Materials and methods
Patients and study design
Patients diagnosed with lymphomas between March 2018 and May 2022 were retrospectively enrolled at Cancer Hospital of Shantou University Medical College. The inclusion criteria were as follows: (1) initially diagnosed with cHL, PMBCL or DLBCL; (2) having treatment-naïve/post-treatment tumor tissue and/or plasma samples meeting quality control standards for genomic DNA or ctDNA extraction; (3) undergoing genomic profiling using an NGS panel targeting 475 hematopoietic and lymphoid neoplasm related genes (Supplementary Table 1); (4) with at least one detectable somatic alteration in tumor tissue and/or ctDNA. This study was approved by Ethics Committee of the Cancer Hospital of Shantou University Medical College (No. 2,023,059). All patients signed informed consent forms prior to enrollment and sample collection.
Among patient having both tumor tissue and plasma samples, the tissue sample was defined as a paired sample if it was collected within three months before/after collecting the plasma sample and systemic therapy was not provided during the three-month period. To assess the applicability of ctDNA testing in lymphomas, we compared the performance of ctDNA with the paired tissue biopsies, including the concordance of detected genetic alterations, the number of unique alterations defined as the alterations exclusively identified in ctDNA and tumor tissue, and the difference of variant allele frequency (VAF). Additionally, the genomic profiles were studied to assess the utility of ctDNA for lymphoma classification, and three publicly available external datasets of cHL [20], PMBCL [25], and DLBCL [26] were used to validate our findings.
DNA extraction, library preparation, and NGS
Tumor genomic DNA from formalin-fixed, paraffin-embedded (FFPE) samples was extracted using QIAamp DNA FFPE Tissue Kit (QIAGEN, Dusseldorf, Germany). 10 mL peripheral blood was collected and centrifuged (1800× g, 10 min, at room temperature) within two hours to separate plasma, from which ctDNA was extracted using QIAamp Circulating Nucleic Acid Kit (QIAGEN, Dusseldorf, Germany). Oral swab DNA was prepared by QIAamp DNA Mini Kit (QIAGEN, Dusseldorf, Germany) as control for germline mutations. Sequencing libraries were prepared using the KAPA Hyper Prep Kit (KAPA Biosystems, Wilmington, MA, USA). Briefly, fragment genomic DNA underwent end-repairing, A-tailing, adapter ligation, size selection, polymerase chain reaction amplification, and purification, sequentially. Target enrichment was performed using customized xGen lockdown probes panel targeting 475 hematopoietic and lymphoid neoplasm related genes (Hemasalus™, Nanjing Geneseeq Inc., Nanjing, China). All procedures were conducted following the manufacturers’ instructions. Enriched libraries were sequenced on Illumina Hiseq4000 NGS platforms (Illumina, San Diego, CA, USA). The average sequencing depth of tissue and liquid biopsies were 1203X and 4554X, respectively.
Sequencing data processing and mutation retaining
FASTQ file quality control was performed using Trimmomatic, and leading/trailing low quality (reading < 15) or N bases were removed [27]. Sequencing data were aligned to the reference human genome (build hg19) and then processed using the Picard suite and the Genome Analysis Toolkit (GATK) [28, 29]. Germline mutations were filtered out by comparing to the oral swab controls. One somatic mutation was retained if it had VAF ≥ 0.5% and at least three unique reads on different strands with good quality scores, after filtering for common single nucleotide polymorphisms. Gene fusions and copy number variations (CNV) were analyzed using FACTERA and ADTEx [30, 31], respectively, followed by manual review in Integrative Genomics Viewer Software (IGV, Broad Institute, Cambridge, MA, USA). CNV with a fold change ≥ 1.6 and ≤ 0.6 was identified as CNV amplification and deletion, respectively.
Variables and statistical analysis
Patient age was categorized into four subgroups, including < 18 years, 18–45 years, > 45 years, and unknown. Frequencies of independent subgroups were compared using Fisher’s exact test. Median and mean comparison were performed using Wilcoxon signed-rank test and two-sample t test, respectively. All quoted P-values were two-tailed, and P-values < 0.05 were considered to be statistically significant. Data were analyzed using R software (version 4.0.3).
Results
Patient characteristics
A total of 155 patients with lymphoma having tumor tissue and/or plasma samples were enrolled, including 49 cHLs, 32 PMBCLs, and 74 DLBCLs. Within our cohort, 110 patients had treatment-naive samples, 33 had post-treatment samples with active disease at the time of sampling and a median of 108 days since the start of treatment (range: 1 to 829 days), and for 12 patients, the treatment status of the samples was unknown. Details on tumor content of tissue samples and ctDNA concentration of plasma samples are summarized in Supplementary Fig. 1. One hundred and eleven patients with paired tissue and plasma samples were included in the paired analyses (22 cHLs, 15 PMBCLs, and 74 DLBCLs, Fig. 1A). The clinical and demographic characteristics of the patients were summarized in Supplementary Table 2. Patients with cHL appeared to have a relatively high proportion of males in comparison to the PMBCL or DLBCL group (63.3% vs. 53.8%, P = 0.30). In contrast, patient age varied significantly across three groups (P < 0.01). 26.5% of cHLs were < 18 years, while most of PMBCLs and DLBCLs were adults at least 18 years old. Patients aged 18–45 years accounted for 13.5% of DLBCLs, which was significantly lower than the proportion in PMBCLs (87.5%, P < 0.01) and cHLs (46.9%, P < 0.01). Disease stage at diagnosis, lactate dehydrogenase level, and bulky site size, were also presented in Supplementary Table 2 despite a relatively large proportion of patients with missing values.
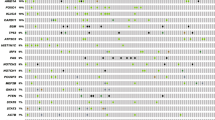
Genomic features comprehensively captured by ctDNA
The concordance of detected genetic alterations between tumor tissue and plasma samples was investigated in cHL, PMBCL, and DLBCL separately. Among 22 cHLs with paired samples, 78% of tissue-based genetic aberrations were captured by ctDNA, with relatively frequently detected SOCS1, STAT6, and TNFAIP3 alterations in ctDNA (Fig. 2A). Notably, PD-L1 and PD-L2 CNV amplifications were exclusively identified by ctDNA. B2M mutations, which were the most prevalent alterations observed, had similar detection rates in two biopsy types, with four and two mutations exclusively identified in plasma and tissue samples respectively (Fig. 2A). Moreover, unique mutations were more common in cHL plasma samples than in paired tissue samples (P < 0.01, Fig. 2B), with higher VAFs observed in ctDNA (P < 0.01, Fig. 2C). Increased VAFs of shared mutations were also observed in ctDNA compared to paired tissue samples (P = 0.06, Fig. 2C). When assessing the applicability of liquid biopsies in 15 PMBCL and 74 DLBCL patients, we observed a high concordance of detectable alterations between ctDNA and paired tissue samples (agreement: PMBCL, 84%; DLBCL, 78%, Fig. 2D, E). Our data also demonstrated that the number of unique mutations appeared to be comparable between ctDNA and tumor tissues in PMBCL (Supplementary Fig. 2A) and DLBCL (Supplementary Fig. 2B).
ctDNA concordance in 22 cHLs, 15 PMBCLs and 74 DLBCLs with paired samples. (A) The oncoplot of 22 cHL patients with paired plasma and tissue samples. (B) The number of unique genetic alterations observed in plasma and tissue biopsies of cHL. (C) Boxplots comparing the unique mutation VAFs, and shared mutation VAFs in plasma and tissue sample of cHL. (D, E) The oncoplot of 15 PMBCLs and 74 DLBCLs with paired plasma and tissue samples
ctDNA assisting in lymphoma identification and classification
As considerable genetic alterations were detected in plasma samples alone, we then investigated if plasma-unique features could assist in distinguishing PMBCL from cHL and DLBCL. Thus, the mutational landscapes based on tissue and liquid biopsies were combined and summarized in Supplementary Fig. 3 for further analyses. Within 19 cHLs having paired samples, the most frequently altered gene was SOCS1 (64%, Supplementary Fig. 3), followed by B2M (59%), STAT6 (59%), and TNFAIP3 (59%). Mutated STAT6 genes were also commonly identified in 15 PMBCLs with paired samples (P > 0.99, Fig. 3A); however, STAT6 mutations were rare in DLBCL when compared to PMBCL (P < 0.01, Fig. 3A). Similar to STAT6, the prevalence of SOCS1 mutation was comparable between cHL and PMBCL (P > 0.99, Fig. 3B), whereas SOCS1 mutations were less common in DLBCL (P < 0.01, Fig. 3B). SOCS1 mutation subtypes exhibited a huge diversity, with considerable truncating variants (black dots, Fig. 3C). Both cHL and PMBCL were rarely detected with BTG2 mutations compared to DLBCL (P = 0.01, Fig. 3D). In contrast, similar proportions of PMBCL and DLBCL patients were detected with PIM1 mutations (P = 0.57, Fig. 3E), whereas few cHL patients carried PIM1 mutations (P = 0.10, Fig. 3E), suggesting the possible similarity between PMBCL and DLBCL in molecular features. Moreover, PD-L1 and PD-L2 CNV amplifications were observed in patients with PMBCL and cHL (Supplementary Fig. 3), suggesting potentially high PD-L1 and PD-L2 expression. When compared to patients with wild-type PD-L1 and PD-L2, the number of concomitant alterations was significantly higher in patients harboring PD-L1 and/or PD-L2 CNV amplification (P < 0.01, Fig. 3F), and no obvious differences were observed between plasma and tissue samples. In DLCBL, BCL6 fusions were detected in 36.5% of patients with paired samples. Although most of these fusions involved immunoglobulin (Ig) genes (Supplementary Fig. 3), multiple non-Ig chromosomal loci were identified as partners, including LAMP3, RPIA, GRHPR, IKZF1, SMC4, RHOH, EIF4A2, HSP90AA1, and H2BC12 (Fig. 3G).
Shared and unique genomic features in three kinds of lymphomas (A) Comparison of STAT6 mutations prevalence in cHL, PMBCL, and DLBCL. (B) Comparison of SOCS1 mutations prevalence in DLBCL, PMBCL, and cHL. (C) Lollipop plots revealing that no obvious hotspots SOCS1 mutations. (D) Comparison of BTG2 mutations prevalence in cHL PMBCL, and DLBCL, with cHL exhibiting significantly lower BTG2 mutation rates than DLBCL. (E) Comparison of PIM1 mutations prevalence in cHL PMBCL, and DLBCL, with cHL exhibiting potentially lower PIM1 mutation rates than PMBCL and DLBCL. (F) The boxplot comparing the number of concomitant alterations for carriers and non-carriers of PD-L1 and/or PD-L2 CNV amplification. (G) BCL6 fusions detected in DLBCL
Next, we evaluated the utility of ctDNA for lymphoma classification by identifying typical genetic alterations that were discovered in paired samples. STAT6 mutations was more common in PMBCL than in cHL, and patients with DLBCL exhibited the lowest STAT6 mutation prevalence (P < 0.01, Fig. 4A). Comparable prevalence of STAT6 mutations was observed in ctDNA when compared to tissue biopsies. Similar results in the prevalence of SOCS1 mutations were also observed, even though ctDNA appeared to capture more SOCS1 mutations in comparison to tissue samples (Fig. 4B). The characteristics of mutated BTG2 (Supplementary Fig. 4A) and PIM1 (Supplementary Fig. 4B) profiled using ctDNA alone did not show obvious differences in comparison to those using paired samples. Based on plasma samples alone, PMBCL patients harboring PD-L1 and/or PD-L2 CNV amplifications still had higher concomitant mutation numbers than PD-L1 and PD-L2 wild-type patients (P = 0.07, Fig. 4C).
Genetic features of lymphomas based on ctDNA alone. (A) The prevalence of mutated STAT6 genes in three lymphomas. (B) The prevalence of mutated SOCS1 genes in three lymphomas. (C) The boxplot comparing the number of concomitant alterations for carriers and non-carriers of PD-L1 and/or PD-L2 CNV amplification in PMBCL
ctDNA performance validation by comparing to external datasets
To further confirm the performance of ctDNA and the NGS panel applied in this study, the prevalence of multiple genetic alterations in our lymphoma patients with plasma samples were compared to that in external datasets. The prevalence of cHL related genes in our study was similar to the external cHL dataset including 106 tissue/plasma samples; however, some genes were not covered by the NGS panel used in the external cHL cohort, such as SOCS1, ACTB, KMT2C, BTG2 (Supplementary Table 3). The detection rates were also comparable between our study cohorts and external cohorts in PMBCL and DLBCL; however, intriguingly, BTG2 mutations were significantly more frequently identified in our DLBCL cohort than in the external dataset consisting of 79 DLBCL plasma samples (43.2% vs. 6.3%, P < 0.01, Supplementary Table 3).
Lymphoma disease surveillance by serial ctDNA
Finally, we explored the utility of ctDNA for lymphoma disease surveillance by analyzing the correlation between ctDNA positivity and responses to treatment or disease progression. Herein, we presented a patient receiving multiple liquid biopsies since the initial diagnosis of cHL in February 2020 (Fig. 5). When the patient was pathologically diagnosed with stage IIA cHL, several genetic alterations were detected in ctDNA, with VAF ranging approximately 1.5–5%. The patient underwent chemotherapy (ABVD: adriamycin, bleomycin, vinblastine, plus dacarbazine) for six cycles. At the cycle 3 (Month 3), complete response was achieved, with no detectable mutations observed by ctDNA test, which suggested that ctDNA positivity could reflect the chemotherapy treatment efficacy. Also, ctDNA status remained negative in Month 6 and 9. However, considerable mutations were identified by the ctDNA test in Month 19, suggesting the possible disease progression which was further confirmed as relapsed stage IV cHL. After immune-based therapy of which the best of response was complete response, ctDNA clearance was observed in Month 21.
Discussion
In this study, we assessed the applicability of ctDNA in lymphomas, and our data demonstrated a high concordance of genetic alterations identified in paired tumor tissue and plasma samples. More alterations were detected exclusively in cHL plasma than in tissue samples, highlighting liquid biopsies as a valuable supplementary approach for genomic profiling in lymphomas. Compared to DLBCL, the genomic characteristics of PMBCL were more similar to cHL, even though these three lymphomas had their unique features. Our data also confirmed the feasibility of serial ctDNA for disease surveillance during chemotherapy and immune-based therapy.
The good concordance between tumor tissue and liquid biopsies in our cohort revealed the promise of ctDNA in lymphoma research. STAT6, SOCS1 and TNFAIP3, which were frequently mutated genes, were more likely to be identified in cHL plasma samples than in tissue samples, suggesting that potential driver mutations of cHL could be captured more sensitively by ctDNA. A recent study has highlighted that DNASE1L3, which is an enzyme breaking down multinucleosomal DNA molecules, shows elevated activity in cHL compared to large B cell lymphomas. The increased activity potentially leading to greater ctDNA release by HRS cells, suggesting a more comprehensive method for lymphoma genomic profiling through plasma ctDNA [32]. A previous study by Spina et al. also demonstrated the utility of ctDNA in profiling genomic features, investigating clonal evolution, and detecting residual disease in cHL [20]. However, a relatively small panel covering 77 genes was applied by Spina et al., and several critical genes, such as SOCS1, PD-L1 and PD-L2, were not included. Consistent with our results, STAT6N417Y and STAT6N419N were identified as potential hotspot mutations by both NGS and allele-specific polymerase chain reaction; however, STAT6N419H, which was commonly observed in our cHL patients, was not identified by Spina et al. A study by Tiacci et al. defined STAT6N419H as a potential hotspot mutation of cHL by whole-exome sequencing, and, interestingly, they also successfully detected STAT6N421S in cHL patients harboring STAT6N417Y simultaneously [33]. For PMBCL and DLBCL, although previous studies tried assessing the applicability of ctDNA, comprehensive analyses based on paired tissue and liquid biopsies, as well as large NGS panels have not been well performed. For instance, mutational landscape of liquid biopsy was highly consistent with that of tissue biopsy, with sensitivity of 69% (95% confidence interval: 60–78%) in a customized 112-gene panel [25]. In DLBCL, measured mutant molecules per mL, which was calculated using ctDNA and an approximately 320Kb panel including recurrently mutated DLBCL genes, was used to stratify patients with inferior progression-free survival and overall survival [34]. Therefore, based on previous studies and our study, findings on both HL and NHL systemically demonstrated that liquid biopsy would be a promising approach to genomic profiling in lymphomas.
Our data showed that mutated SOCS1 and STAT6 genes were common in both cHL and PMBCL. Previous studies revealed that SOCS1 inactivating mutations, CNV deletions, and inactivating fusions could negatively regulate the JAK-STAT signaling pathway, and further leaded to the overexpression of STAT proteins [35]. Moreover, it is believed that STAT6 mutations could also cooperated with SOCS1 disruption [33]. Consistent with these previous findings, our data demonstrated that STAT6 might be an oncogene with hotspot mutations related to gain-of-function, and SOCS1 truncating mutations were observed. Although we did not observe a co-occurrence pattern in alterations between these two genes, considerable cHL and PMBCL patients harbored them simultaneously. Noerenberg et al.’s study revealed no significant co-occurrence (q = 0.18) between STAT6 and SOCS1 mutations and their minimal impact on progression-free survival and overall survival in PMBCL patients [36]. However, it might be interesting to compare the prognosis of cHL patients with both SOCS1 and STAT6 mutations and prognosis of patients with only one of them. Noerenberg et al. also highlighted the prognostic significance of DUSP2 and CD58 mutations in PMBCL. We observed high alignment for DUSP2 (100%, 3 of 3) and substantial agreement for CD58 (67%, 4 of 6) mutations between ctDNA and tissue biopsies, underscoring ctDNA’s utility in predicting patients’ outcomes [36]. GNA13, a tumor suppressor inhibiting AKT phosphorylation, was also a frequently mutated gene in our patients with cHL, which was consistent with previous studies [37, 38]. GNA13 mutations related to loss of function were considered to be associated with STAT6 aberrations [35]; however, our data did not show a statistically significant co-occurrence pattern between mutated GNA13 and STAT6 genes, which might be rationalized by the relatively small sample size.
In our PMBCL cohort, considerable patients were identified with CNV amplification of PD-L1 and PD-L2 genes, and these patients also carried more concomitant alterations than those without PD-L1 or PD-L2 amplifications. In the phase IB KEYNOTE-013 and the phase II KEYNOTE-170 trials, relapsed or refractory PMBCLs with high PD-L1 scores could achieve better responses and efficacy under pembrolizumab treatment than those with low PD-L1 scores [39]. Similarly, our data suggested that immunotherapy might be a potentially good option to PMBCL detected with PD-L1 or PD-L2 amplifications. Notably, we were not able to identify prevalent PD-L1 or PD-L2 amplifications in our cHL cohort, whereas PD-L1 and/or PD-L2 amplifications were considered as a defining feature of cHL. A fluorescent in situ hybridization (FISH) assay was used to characterize 9p24.1 PD-L1 and/or PD-L2 alterations in 108 cHL patients, and 56% and 36% patients were classified as copy gain and amplification, respectively [40]. Moreover, 97 of 108 patients had concordant alterations of PD-L1 and PD-L2. By contrast, Vranic et al.’s study including 11 cHL patients revealed that all three cHL patients with positive FISH results were not NGS-positive under a panel covering 592 genes [41], which resembles our findings that the prevalence of PD-L1 and PD-L2 CNV amplification was not as high as expected. Vranic et al. believed that there might be unknown mechanism involved in cHL PD-L1 upregulation and overexpression when given the fact that a fraction of immunohistochemically positive cHLs were NGS and/or FISH negative; however, we supposed that our relatively low PD-L1 and PD-L2 CNV amplification prevalence could be partially rationalized by clinical stage, as the FISH amplification detection rate increased when clinical stage getting advanced [40]. Owing to a lack of clinical stage data in our cHL cohort, further studies are required.
This study has limitations. As a retrospective study, there were considerable missing values for patients’ clinical information, such as clinical stage, bulky disease, lactate dehydrogenase level, treatment history, survival data, etc., resulting in the difficulty in defining whether our study cohort was comparable to the cohorts of other studies. Also, the sample size of each lymphoma cohort was limited, especially when paired tissue and plasma samples were analysed. Moreover, the sample size of our study cohort might limit the ability to draw definitive conclusion regarding the sensitivity of ctDNA genotyping, and studies with larger study populations are required. Finally, samples included in this study were not completely treatment-naïve, which means that there might be secondary mutations acquired due to resistance.
In conclusion, liquid biopsy was a promising approach to genomic profiling and disease surveillance in cHL, PMBCL, and DLBCL, with highly concordant alterations identified by tissue biopsies and good agreement with response to treatment. Despite some distinctive molecular features, PMBCL had more genetic abnormalities like cHL than DLBCL. Further analyses using large cohorts for the independent use of liquid biopsies in disease surveillance are warranted.
Data availability
The lists of mutations identified in 155 tumor tissue and/or liquid biopsy samples are provided as supplementary tables. Other datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- cHL:
-
classic Hodgkin lymphoma
- CNV:
-
copy number variations
- ctDNA:
-
circulating tumor DNA
- DLBCL:
-
diffuse large B-cell lymphoma
- FFPE:
-
formalin-fixed paraffin-embedded
- HL:
-
Hodgkin lymphoma
- Ig:
-
immunoglobulin
- VAF:
-
variant allele frequency
- NGS:
-
next-generation sequencing
- NHL:
-
non-Hodgkin lymphoma
- PMBCL:
-
primary mediastinal large B-cell lymphoma
References
Jamil A, Mukkamalla SKR, Lymphoma (2022) StatPearls [Internet]: StatPearls Publishing
Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O et al (2010) Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. J Am Soc Hematol 116(19):3724–3734
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al (2008) WHO classification of tumours of haematopoietic and lymphoid tissues. International agency for research on cancer Lyon
Ahmed Z, Afridi SS, Shahid Z, Zamani Z, Rehman S, Aiman W et al (2021) Primary mediastinal B-cell lymphoma: a 2021 update on genetics, diagnosis, and novel therapeutics. Clin Lymphoma Myeloma Leuk 21(11):e865–e75
Martelli M, Ferreri A, Di Rocco A, Ansuinelli M, Johnson PW (2017) Primary mediastinal large B-cell lymphoma. Crit Rev Oncol/Hematol 113:318–327
Garg M, Takyar J, Dhawan A, Saggu G, Agrawal N, Hall A et al (2022) Diffuse large B-Cell lymphoma (DLBCL): a structured literature review of the Epidemiology, Treatment guidelines, and real-world treatment patterns. Blood 140(Supplement 1):12106–12107
Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML et al (1994) A revised european-american classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood 84(5):1361–1392
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, de Oliveira Araujo IB, Berti E et al (2022) Correction:The 5th edition of The World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms Leukemia. ; 36 (7): 1720–1748. Leukemia. 2023;37(9):1944-51
Campo E, Jaffe ES, Cook JR, Quintanilla-Martinez L, Swerdlow SH, Anderson KC et al (2022) The international consensus classification of mature lymphoid neoplasms: a report from the clinical advisory committee. Blood J Am Soc Hematol 140(11):1229–1253
Joos S, Otaño-Joos MI, Ziegler S, Bruderlein S, Du Manoir S, Bentz M et al (1996) Primary mediastinal (thymic) B-cell lymphoma is characterized by gains of chromosomal material including 9p and amplification of the REL gene
Twa DD, Chan FC, Ben-Neriah S, Woolcock BW, Mottok A, Tan KL et al (2014) Genomic rearrangements involving programmed death ligands are recurrent in primary mediastinal large B-cell lymphoma. Blood J Am Soc Hematol 123(13):2062–2065
Joos S, Küpper M, Ohl S, Von Bonin F, Mechtersheimer G, Bentz M et al (2000) Genomic imbalances including amplification of the tyrosine kinase gene JAK2 in CD30 + Hodgkin cells. Cancer Res 60(3):549–552
Viganò E, Gunawardana J, Mottok A, Van Tol T, Mak K, Chan FC et al (2018) Somatic IL4R mutations in primary mediastinal large B-cell lymphoma lead to constitutive JAK-STAT signaling activation. Blood. J Am Soc Hematol 131(18):2036–2046
Jones D, Windham J, Stewart B, Fayad L, Rodriguez A, Hagemeister FB (2009) Differential JAK-STAT pathway activation in primary Mediastinal large B-Cell lymphoma: two subgroups with Differential Cytokine activation patterns and predicted responses to kinase inhibitors. Blood 114(22):968
Weniger MA, Küppers R (2021) Molecular biology of Hodgkin lymphoma. Leukemia 35(4):968–981
Schmitz R, Hansmann M-L, Bohle V, Martin-Subero JI, Hartmann S, Mechtersheimer G et al (2009) TNFAIP3 (A20) is a tumor suppressor gene in Hodgkin lymphoma and primary mediastinal B cell lymphoma. J Exp Med 206(5):981–989
Shi M, Roemer MG, Chapuy B, Liao X, Sun H, Pinkus GS et al (2014) Expression of programmed cell death 1 ligand 2 (PD-L2) is a distinguishing feature of primary mediastinal (thymic) large B-cell lymphoma and associated with PDCD1LG2 copy gain. Am J Surg Pathol 38(12):1715
Schnitzer B (2009) Hodgkin lymphoma. Hematol Oncol Clin N Am 23(4):747–768
Santisteban-Espejo A, Bernal-Florindo I, Perez-Requena J, Atienza-Cuevas L, Moran-Sanchez J, Fernandez-Valle MC et al (2022) The need for standardization in next-generation sequencing studies for classic Hodgkin lymphoma: a systematic review. Diagnostics 12(4):963
Spina V, Bruscaggin A, Cuccaro A, Martini M, Di Trani M, Forestieri G et al (2018) Circulating tumor DNA reveals genetics, clonal evolution, and residual disease in classical Hodgkin lymphoma. Blood J Am Soc Hematol 131(22):2413–2425
Camus V, Viennot M, Lequesne J, Viailly P-J, Bohers E, Bessi L et al (2021) Targeted genotyping of circulating tumor DNA for classical Hodgkin lymphoma monitoring: a prospective study. Haematologica 106(1):154
Kamaeva IA, Novikova IA, Lysenko IB, Timoshkina NN, Nikolaeva NV, Kapuza EA et al (2022) Newly identified molecular and genetic characteristics of primary mediastinal large B-cell lymphoma. American Society of Clinical Oncology
Lauer EM, Mutter J, Scherer F (2022) Circulating tumor DNA in B-cell lymphoma: technical advances, clinical applications, and perspectives for translational research. Leukemia 36(9):2151–2164
Pang D, Jiang X, Huang L, Teng Y, Liu S, Chen F et al (2020) Ctdna monitoring in predicting relapse of primary mediastinal B-Cell lymphoma. Blood 136:36
Rivas-Delgado A, Nadeu F, Andrade-Campos M, López C, Enjuanes A, Mozas P et al (2022) Cell-free DNA for genomic analysis in primary Mediastinal large B-Cell lymphoma. Diagnostics 12(7):1575
Rivas-Delgado A, Nadeu F, Enjuanes A, Casanueva-Eliceiry S, Mozas P, Magnano L et al (2021) Mutational landscape and tumor burden assessed by cell-free DNA in diffuse large B-cell lymphoma in a population-based study. Clin Cancer Res 27(2):513–521
Bolger AM, Lohse M, Usadel B (2014) Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30(15):2114–2120
DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C et al (2011) A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet 43(5):491–498
Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows–Wheeler transform. Bioinformatics 25(14):1754–1760
Amarasinghe KC, Li J, Hunter SM, Ryland GL, Cowin PA, Campbell IG et al (2014) Inferring copy number and genotype in tumour exome data. BMC Genomics 15(1):1–12
Newman AM, Bratman SV, Stehr H, Lee LJ, Liu CL, Diehn M et al (2014) FACTERA: a practical method for the discovery of genomic rearrangements at breakpoint resolution. Bioinformatics 30(23):3390–3393
Alig SK, Shahrokh Esfahani M, Garofalo A, Li MY, Rossi C, Flerlage T et al (2024) Distinct Hodgkin lymphoma subtypes defined by noninvasive genomic profiling. Nature 625(7996):778–787
Tiacci E, Ladewig E, Schiavoni G, Penson A, Fortini E, Pettirossi V et al (2018) Pervasive mutations of JAK-STAT pathway genes in classical Hodgkin lymphoma. Blood J Am Soc Hematol 131(22):2454–2465
Herrera AF, Tracy S, Croft B, Opat S, Ray J, Lovejoy AF et al (2022) Risk profiling of patients with relapsed/refractory diffuse large B-cell lymphoma by measuring circulating tumor DNA. Blood Adv 6(6):1651–1660
Brune MM, Juskevicius D, Haslbauer J, Dirnhofer S, Tzankov A (2021) Genomic landscape of Hodgkin lymphoma. Cancers 13(4):682
Noerenberg D, Briest F, Hennch C, Yoshida K, Hablesreiter R, Takeuchi Y et al (2024) Genetic characterization of primary mediastinal B-cell lymphoma: pathogenesis and patient outcomes. J Clin Oncol 42(4):452–466
Wienand K, Chapuy B, Stewart C, Dunford AJ, Wu D, Kim J et al (2019) Genomic analyses of flow-sorted Hodgkin Reed-Sternberg cells reveal complementary mechanisms of immune evasion. Blood Adv 3(23):4065–4080
Desch A-K, Hartung K, Botzen A, Brobeil A, Rummel M, Kurch L et al (2020) Genotyping circulating tumor DNA of pediatric Hodgkin lymphoma. Leukemia 34(1):151–166
Armand P, Rodig S, Melnichenko V, Thieblemont C, Bouabdallah K, Tumyan G et al (2019) Pembrolizumab in relapsed or refractory primary mediastinal large B-cell lymphoma. J Clin Oncol 37(34):3291
Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H et al (2016) PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol 34(23):2690
Vranic S, Ghosh N, Kimbrough J, Bilalovic N, Bender R, Arguello D et al (2016) PD-L1 status in refractory lymphomas. PLoS ONE 11(11):e0166266
Acknowledgements
The authors thank all the patients who participated in this study.
Funding
This study was supported by Medical Science and Technology Foundation of Guangdong Province (no.A2021426, to Zhao Wang), Medical Scientific Research Foundation of Guangdong Province (NO.B2022161, to Hongbiao Wang), National Natural Science Foundation of China (nos.81872902, 82073917, to Zhi-Ming Li), National Natural Science Foundation of Guangdong Province (no.2023A1515011525, to Zhi-Ming Li), and the Lymphoma Research Fund of China Anti-Cancer Association and the Sun Yat-sen University Cancer Center Clinical Research 308 Program (nos. 2014-fxy-106 and 2016-fxy-079, to Zhi-Ming Li).
Author information
Authors and Affiliations
Contributions
Z-M Li and H Yang conceived and design the study. H Wang, Z Wang, S Zhu, Z Li, H Yang, P Sun, L Shen, M Zhu, X Zhao, and Q Ou analyzed data and interpreted results. M Zhu, L Shen, and X Zhao were responsible for data visualization. All authors wrote, revised, and reviewed the manuscript. Z-M Li and H Yang supervised the whole project. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
M Zhu, X Zhao, L Shen, and Q Ou are employees of Nanjing Geneseeq Technology Inc., China. The remaining authors have nothing to disclose.
Ethical approval and consent to participate
This study was approved by Ethics Committee of the Cancer Hospital of Shantou University Medical College (No. 2023059). All patients signed informed consent forms prior to enrollment and sample collection.
Conflict of interest
M Zhu, X Zhao, L Shen, and Q Ou are employees of Nanjing Geneseeq Technology Inc., China. The remaining authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Wang, Z., Zhu, S. et al. Circulating tumor DNA assisting lymphoma genetic feature profiling and identification. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05782-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05782-0