Abstract
Natural killer (NK) cell based immunotherapy is an emerging strategy in hematologic malignancies because allogeneic NK cells can provide potent antitumor immunity without inducing graft-versus-host disease. Thus, we expanded cord blood-derived NK (CB-NK) cells ex vivo from random (MHC mismatched and KIR mismatched) donors, and investigate the feasibility and efficacy of repeated infusions CB-NK cells as maintenance therapy after autologous hematopoietic stem cell transplantation (ASCT). Thirty-one patients with acute myeloid leukemia and high-risk lymphoma received ASCT and the adoptive CB-NK cell multiple infusions for maintenance therapy. Patients received a median dose of 5.98 × 107/kg (range, 1.87-17.69 × 107/kg) CB-NK cells and 23 patients completed four infusions, 8 patients received three infusions. Only mild infusion reactions occurred in 15.5% of 116 infusions. Compared to a contemporaneous cohort of 90 patients who did not receive NK cell therapy, the adoptive transfer of CB-NK cells as maintenance treatment showed a tendency of difference in decreasing the relapse rate between CB-NK group and control group (9.7% vs 24.4%). The patients who receiving NK cell infusions had a better PFS and OS than controls (4 year PFS, 84.4 ± 8.3% vs 73.5 ± 5.4%; and 4 year OS, 100% vs 78.1 ± 5.4%) . These findings demonstrate safety and validity of maintenance therapy using CB-NK cells multiple infusions after ASCT, and it is worthy of further clinical trial verification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autologous hematopoietic stem cell transplantation (ASCT) has been recommended as an effective treatment strategy for several hematologic malignancies. Many studies demonstrated that ASCT remarkably reduced the relapse rate and increased the survival compared to chemotherapy in patients with favorable and intermediate risk acute myeloid leukemia (AML) in first complete remission (CR) and the high risk non-Hodgkin's lymphoma (NHL) [1,2,3,4,5]. Compared the clinical outcomes of ASCT with allogeneic hematopoietic stem cell transplantation (allo-HSCT) in the above disease subtypes, the results showed comparable outcomes regarding to overall survival (OS) and progress-free survival (PFS) [6,7,8]. Although ASCT have substantially improved the disease prognosis, tumor relapse still remains the major cause for the treatment failure. So it is essential to explore maintenance therapy after ASCT to mitigate relapse rate and enhance curative efficacy.
NK cells comprise an essential part of the cellular immune system, with latent capacity to rapidly kill tumor cells and virally infected cells. As in allo-HSCT, higher absolute NK cell numbers in the early posttransplant period were associated with lower relapse and improved survival, and early immune reconstitute after ASCT has been associated with prolonged survival [9, 10]. Discovery of the NK cells anti-tumor effect is perhaps one of the greatest scientific milestones of the past two decades and have helped develop cell therapy platforms based precisely on the HLA differences between donor and recipient [11]. Allogeneic NK cells that express inhibitory receptors, such as killer immunoglobulin-like receptors (KIRs), and that are not inhibited by the HLA molecules of the patient’s tumor cells cause a powerful anti-tumor effect (KIR-HLA mismatch). Many studies applied the adoptive allogeneic NK cell infusions to enhance NK cell function to prevent tumor relapse and have been primarily successful in patients with AML [12,13,14]. For the same reason, the adoptive haploidentical donor- or cord blood-derived allogeneic NK cell infusions have also been used for the ASCT patients [15, 16]. This provides the rationale for testing the use of major histocompatibility complex (MHC) mismatched and KIRs mismatched allogeneic NK cells for cellular therapy to contribute to a graft versus tumor effect, and prevent relapse after ASCT.
In this study, we hypothesized that multiple infusions of high numbers of mature, fully functional allogeneic CB-NK cells as maintenance treatment after ASCT would improve antitumor effect and reduce relapse rate in hematologic malignancies. To verify the concept, we performed a single-arm study to determine the safety and clinical efficacy of multiple infusions of CB-NK cells after ASCT.
Material and methods
Patient population
From January 2017 to December 2021, the patients with favorable- and intermediate-risk AML and high-risk NHL who received ASCT hospitalized in West China Hospital were recruited in this study. Risk stratification was carried out for AML based on European Leukemia Net (ELN) recommendations [17] and high-risk lymphomas were defined as one of the following conditions: 1) high-risk diffuse large B-cell lymphoma (DLBCL) according to Revised International Prognostic Index (R-IPI) at diagnosis [18]; 2) DLBCL with the expression of both MYC and B-cell lymphoma 2 (BCL2) proteins (double-expressor lymphoma, DEL), and B-cell lymphoma accompanied by MYC and BCL2 rearrangements (double-hit lymphoma, DHL); 3) relapsed and refractory NHL; and 4) T-NHL, including: peripheral T-cell lymphoma (PTCL) and extra-nodal NK/T-cell lymphoma (ENKTL) in the advanced stage. Other inclusion criteria involved Eastern Cooperative Oncology Group (ECOG) performance status ≤ 2, adequate cardiac function (left ventricular ejection fraction ≥ 40%), lung function (forced expiratory volume per second [FEV1]/forced vital capacity [FVC] ˃ 70%), hepatic function (alanine aminotransferase [ALT] and aspartate aminotransferase [AST] ≤ 2.5 the upper limit of normal [ULN] and total bilirubin ≤ 1.5 ULN) and renal function (creatinine clearance ≥ 50 mL/min).
All research was reviewed and approved by the Ethics Committees of West China Hospital, Sichuan University, and the written informed consent was obtained from all patients. This study was registered at clinicaltrials.gov (NCT05250362).
Treatment
The conditioning regimens of ASCT for AML included FAB (fludarabine-cytarabine-busulfan), Chi-FAB (chidamide + FAB) and Chi-CAB (chidamide- cladribine-cytarabine-busulfan), and the regimens for NHL were Chi-CGB (chidamide-cladribine-gemcitabine-busulfan), BeEMA (bendamustine-etoposide-melphalan-cytarabine), and Chi-BeEMA (chidamide + BeEMA). When the clinical setting showed hematopoietic engraftment and blood cell counts recovery (usually at day +30 after ASCT), the patients started to receive ex vivo-expanded CB-NK cell product infusion at a dose of 4.5×109 nucleated cells (mean 5.98 ×107/kg NK cells) every three months for four times in the first year post transplant (Fig. 1). No immunosuppression agent was given prior to CB-NK cells infusion, and only promethazine was mandated to prevent anaphylaxis. During every course of infusion, the total dose of 4.5×109 nucleated cells were administered into two split doses1.5×109 and 3.0×109, intravenously infusing in 30-60min for two consecutive days.
Treatment schema for the clinical study of adding infusions of expanded umbilical cord blood NK cells to the maintenance therapy after autologous hematopoietic stem cell transplantation (ASCT). Chi, chidamide; FA, fludarabine;Ara-c, cytarabine; BUS, busulfan; CDA, cladribine; GEM, gemcitabine; Benda, bendamustine; VP-16, etoposide; MEL, melphalan
In addition to CB-NK cell infusions, some agents were also available for the maintenance therapy after ASCT, including interleukin-2 for AML patients, rituximab, anti-PD-1 antibody, lenalidomide, chidamide, and BTK inhibitors for NHL patients.
CB-NK cell production
Cord blood units were obtained from the Sichuan Cord Blood Bank after obtaining informed consent as donation for cord blood stem cell banking with the compliance of the ethical committee review board of Sichuan Cord Blood Stem Cell Bank (LL-20100310-QX-1; LL-20151029-QD-1). CB-NK expansion ex vivo was under a good manufacturing practice (GMP)-compliant culture method. We used a feeder cell-free NK cell expansion system to obtain a high quantity of highly pure NK cells from cord blood mononuclear cells (CBMCs). The detailed description of the method was presented in the patent (CN107384859A). Briefly, CBMCs were isolated by Ficoll density gradient centrifugation from fresh CB units and cultured at 37 °C with 5% CO2 for 14 days in gas permeable bioreactors in X-VIVO 15 medium supplemented with 5-10% human serum in the presence of 500 U/mL IL-2 and 30 ug/mL IL-15 at the initial concentration of (0.8-1.0) ×106/mL. At the end of culture (day 14), quality controls were performed involving microbial detection, cell number, viability and cellular composition of cultures. Final NK product release criteria included sterile, endotoxin assay < 2 IE/mL and cell viability of ≥ 80%.
Phenotype and function of expanded NK cells
After expansion cultures, phenotypic and functional characteristics of expanded NK cells were assayed by flow cytometry. Expanded NK cells were stained with the following antibodies: anti-CD3, anti-CD56, anti-CD16, anti-CD69, anti-NKp30, anti-NKp44, anti-NKp46, anti-NKG2D, anti-CD69, anti-CD96, anti-NKG2A, anti-CD158; KIR2DL1/S1/S3/S5 and anti-TIGIT. To estimate NK cells cyto-toxicity, expanded NK cells were co-incubated with carboxyfluorescein succinimidyl ester (CFSE)-labeled K562 for 4 hours at an effector-to-target (E:T) ratio of 5:1 assaying 7-aminoactinomycin D (7AAD) uptake as described [19]. Sample acquisition was performed on the CytoFLEX (Beckman Coulter) and data were analyzed with CXP software (Beckman Coulter).
Clinical assessment
The primary objective was to evaluate the safety and tolerability of CB-NK cells infusion. An evaluation of adverse effects was conducted using National Cancer Institute Common Toxicity Criteria (Version 4.0.3) [20]. Secondary objectives were to estimate relapse rate (RR), PFS, and OS. Response of acute leukemia was evaluated by bone marrow aspiration at 1, 2, 3, 4, 6, 9 and 12 months after transplantation and every 6 months thereafter according to ELN 2017 criteria. The lymphoma stage was assessed by positron emission tomography-computed tomography (PET/CT) when 1 month prior to study, as well as 3, 6, 9 and 12 months after transplantation, then every 6 months for 2 years, and then yearly. Response assessment was in accordance with the Lugano 2014 criteria [21].
Statistical methods
This was a single-arm pilot study that sequentially included 31 patients with AML or NHL after they obtained disease CR. The patients with the same disease status during the same period who had received ASCT without NK cells infusion were used as contemporaneous control for survival analysis. PFS duration was defined as the time from transplantation to treatment failure (relapse, progression or death) or last follow-up. OS was calculated as the time from transplantation to death or last contact. The survival curves were estimated using the Kaplan-Meier method and compared by the log-rank tests. Comparison of patient characteristics among two groups was accomplished by the Fisher’s exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables. P value < 0.05 was considered as significant. Data were analyzed using SPSS (version 22, SPSS, Chicago, IL, USA) and GraphPad Prism 8.0 (GraphPad Software, San Diego, CA, USA) software.
Results
Patients and characteristics
In total, 121 patients who were compliance with inclusion criteria received ASCT from 2017 to 2021 in West China Hospital. Among them, 31 patients with median age of 40 years (range, 15-60 years) followed by CB-NK cells multiple infusions as maintenance therapy after ASCT on a voluntary basis. In control group, 90 patients with median age of 46 years (range, 16-68 years) underwent ASCT without CB-NK cells infusions. Patient demographic and clinical characteristics are summarized in Table 1. In CB-NK infusion group, diagnoses include AML (n = 10), B-cell non-Hodgkin lymphoma (n = 18), and mature T cell or NK/T cell lymphoma (n = 3). Favorable and intermediate risk AML patients each accounted for 50%. 29 patients achieved CR1 (93.5%), and 1 patient was in CR2 (3.2%), another was in PR (3.2%). In control group, 90 patients including AML (n = 12), B-NHL (n= 57) and mature T cell or NK/T cell lymphoma (n=21). Cytogenetic analysis showed favorable-risk AML in 8 cases and intermediate-risk AML in 4 cases. 77 patients achieved CR1(85.6%), and 11 patients were in CR2 or CR3(12.2%), other 2 were in PR(2.2%). The baseline analysis of clinical characteristics was performed, and the results showed either AML or NHL patients in CB-NK group or control group were comparable (Table 1, Supplementary Table S1 and S2). In all ASCT patients, the median CD34+ cells infused was 2.87 × 106/kg (range, 1.37-10.69 × 106/kg), and successful engraftment was achieved by all patients. The median time to neutrophil engraftment (absolute neutrophil count ˃ 0.5 × 109/L) and platelet engraftment (absolute platelet count ˃ 20 × 109/L) was 10 days (range, 8-13 days) and 13 days (range, 9-21 days). Baseline and engraftment characteristics were not statistically different between CB-NK group and control group. In control group, a patient showed a delayed platelet recovery and the time to platelet engraftment was 97 days.
Expanded CB-NK cell product
A total of 116 CB-NK culture products were completed with the mean total nucleated cells viability of 98.45% (range, 89.11-99.72%). The median CD3-CD56+ and CD3+ content of the expanded CB-NK cell products was 84.35% (range, 50.2-98.3%) and 11.88% (range, 0.94-48.76%), respectively, and the wide range of NK cell and T cell proportions was likely due to the substantial variability of cord blood NK cells in CB units and the manufacture skill improvement. NK cells killed K562 cells with 85.99% (range, 53.88-93.90%) lysis at an E:T ratio of 5:1 (Table 2). Phenotype analysis of expanded CB-NK cells was performed in expanded products. All CB-NK cells expressed activating as well as inhibitory receptors in varying degrees. The phenotype of CD56+CD3- cells expressed high levels of the activating receptors CD16 (median 74.45%; range 24.08-95.93%), NKG2D (median 91.07%; range 67.94-99.24%), NKp30 (median 84.46%; range 30.51-94.68%), NKp44 (median 75.86%; range 55.04-93.14%) and NKp46 (median 74.79%; range 28.91-87.07%). (Fig. 2)
CB-NK cells infusion
Thirty-one patients received a median dose of 5.98 ×107/kg (range, 1.87-17.69 × 107/kg) NK cells and 23 patients completed four infusions, 8 patients received three infusions. Only mild toxicities were associated with CB-NK cells infusion therapy, which was well tolerated. The incidence of nonhematologic adverse events in 116 infusions was extremely low, including chills, fatigue, fever, vomiting headache, rash, myalgia and edema limbs (Table 3). No significant hematologic toxicities and graft-versus-host disease(GVHD) were observed in all patients.
Patient outcomes
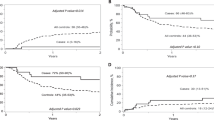
The median follow-up time of CB-NK group and control was 30.13 (9.93- 57.23) months and 29.43 (3.23-57.8) months, respectively. During the total follow-up time, there was a tendency of difference of relapse rate between CB-NK group and control group (9.7% vs 24.4%; P = 0.080). The patients who receiving NK cell infusions had a better PFS and OS than controls (4 year PFS, 84.4 ± 8.3% vs 73.5 ± 5.4%; P = 0.060; and 4 year OS, 100% vs 78.1 ± 5.4%; P = 0.016). In respect of the two major disease categories, in AML, 4 year PFS, 88.9% vs 81.5%, P = 0.499; 4 year OS, 100% vs 88.9%, P = 0.317; and in NHL, 4 year PFS, 80.2% vs 72.1%, P = 0.154; 4 year OS, 100% vs 76.1%, P = 0.046) (Fig. 3).
Comparison of clinical outcomes between patients treated with (solid line) or without (dashed line) cord blood derived-NK cells. Probability of progression-free and overall survival. Kaplan-Meier survival curves were compared using the log-rank method. A All patients. B Patients with acute myeloid leukemia. C Patients with non-Hodgkin lymphoma
Discussion
This is a pilot study on the high doses of ex vivo-expanded allogeneic CB-NK cells multiple infusions were administered as long-term maintenance therapy after ASCT. Compared to a contemporaneous patient cohort without NK cell infusions, there was a tendency of difference of decreased the relapse rate (9.7% vs 24.4%) and improved 4-year PFS (84.4% vs 73.5%) and OS (100% vs 78.1%) in CB-NK cell infusions patients. The higher number of CB-NK cells were successfully generated and safely infused, resulting in a promising method of using MHC mismatched and KIRs mismatched allogeneic CB-NK cells for cellular therapy to contribute to a graft versus leukemia/tumor effect, and prevent relapse of AML and high-risk lymphoma after ASCT. The efficacy and safety of a single dose or multiple doses of adoptive NK cells transferring were previously studied in hematologic malignancies. In a non-HSCT setting, adequate lymphodepletion and exogenous IL-12 or IL-15 could lead to expansion and persistence of adoptively transferred haploidentical NK cells or CB-NK cells in vivo [22, 23]. Infusion of allogeneic NK cells could induce remission and be against leukemia relapse in poor-prognosis and relapsed AML patients [24, 25]. In transplant setting, either for allo-HSCT or ASCT, the adoptive immunotherapy with allogeneic NK cells derived from donor or cord blood in the period of peritransplant improved NK-cell immune reconstitution, decreased the tumor relapse rate and the incidence of viral reactivation, and achieved better survival [12,13,14,15,16, 26]. In our study, the multiple infusions of allogeneic CB-NK cells as maintenance therapy after ASCT also showed promising results.
NK-cell adoptive transfer immunotherapy needs enough amounts of activated NK cells, and some previous studies used feeder cell systems for NK cells expansion in vitro [16, 26]. Although the culture conditions have been standardized according to good manufacturing practices, the use of cancer cell lines for NK cell production and clinical applications is still controversial. Therefore, we established a feeder cell-free system to produce active cord blood NK cells by cytokines stimulation. Previous studies have indicated that the proportion of CD56brightCD16- NK cell in cord blood is higher than that in peripheral blood. CB-NK cells are younger and have a stronger proliferation potential than the peripheral blood counterparts [27, 28]. In our study, the cytokine-expanded CB-NK cells displayed high expression of certain activating and inhibitory receptors, including CD16, NKp30, NKp44, NKp46, NKG2D, CD96, NKG2A, and the cytotoxic function of expanded NK cells was enhanced. Only mild infusion reactions and no GVHD were found in our study, confirming the safety and feasibility of this cellular therapy.
Previous data obtained with adoptive haploidentical KIR–HLA-mismatched NK cells offer safety, transient engraftment and efficacy in adult patients with AML, KIR-HLA class I mismatch is associated with anti-tumor effect of NK cells [11, 25], and by the general availability of haploidentical family members as NK cell donor to support the treatment. Alternative donor types include KIR-ligand mismatched or fully random cord blood donors. Although random donor NK cells carry the disadvantage of immune mediated rejection, obvious advantages are availability and the possibility to natural select a donor with appropriate KIR repertoire. At present, NK cell donor choice remains a matter of investigation, and no specific setting is known to be clearly superior to others. Multiple infusions of NK cells might be a crucial issue to benefit of adoptive NK cell therapy. A clinical trial using haploidentical NK cells treated nontransplant AML patients found chimerism levels of donor NK cells decreased after two weeks from the time of NK cell infusion in most patients [22]. In unmatched immune environment, the duration of NK cells is limited on account of rejection by recipient T cells. But some studies demonstrated that adoptive NK cells could persist for more than 3 months in an immune-compatible environment [12]. However, the optimal persistence of transfused cells in the circulation is not clear. Our study used random cord blood as NK cell donors, and the multiple infusions of high doses of ex vivo-expanded CB-NK cells were administered as long-term maintenance therapy after ASCT. These perhaps have some rationality of each CB-NK cell product with appropriate KIR repertoire to obtain the advantages of anti-leukemia/lymphoma. Currently, some approaches improving survival of infused NK cells include the administration of IL-2 or IL-15 [29, 30] , and pre-infusion immunosuppression agents, such as combination of fludarabine and cyclophosphamide for lymphodepletion [12, 23] .
Since this is a pilot study, there are some limitation. Firstly, the clinical results reported here are from a single-arm, relatively small sample size, and the control cohort is not a randomized design, the results require further validation in a randomized controlled clinical trial with more cases. In addition, the dynamic change and persistence of adoptive NK cells in vivo are not monitored.
In summary, in this pilot study, we confirmed the clinical safety and feasibility of high doses of CB-NK cell products derived from multiple random (MHC mismatched and KIR mismatched) donors. Repeated the CB-NK cell infusions as maintenance therapy after ASCT showed a tendency of difference in decreasing the relapse and improving long term survival in AML and high-risk lymphoma. Future clinical investigation of this therapy and correlative dynamic studies of NK cells in vivo are warranted.
Data availability
The datasets used and/or analyzed during the study are available from the corresponding author on reasonable request.
References
Vellenga E, van Putten W, Ossenkoppele GJ, Verdonck LF, Theobald M, Cornelissen JJ et al (2011) Autologous peripheral blood stem cell transplantation for acute myeloid leukemia. Blood 118(23):6037–6042
Venditti A, Piciocchi A, Candoni A, Melillo L, Calafiore V, Cairoli R et al (2019) GIMEMA AML1310 trial of risk-adapted, MRD-directed therapy for young adults with newly diagnosed acute myeloid leukemia. Blood 134(12):935–945
Passweg JR, Labopin M, Christopeit M, Cornelissen J, Pabst T, Socié G et al (2020) Postremission Consolidation by Autologous Hematopoietic Cell Transplantation (HCT) for Acute Myeloid Leukemia in First Complete Remission (CR) and Negative Implications for Subsequent Allogeneic HCT in Second CR: A Study by the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT). Biol Blood Marrow Transplant 26(4):659–664
Stiff PJ, Unger JM, Cook JR, Constine LS, Couban S, Stewart DA et al (2013) Autologous transplantation as consolidation for aggressive non-Hodgkin's lymphoma. N Engl J Med 369(18):1681–1690
Dahi PB, Lazarus HM, Sauter CS, Giralt SA (2019) Strategies to improve outcomes of autologous hematopoietic cell transplant in lymphoma. Bone Marrow Transplant 54(7):943–960
Mizutani M, Hara M, Fujita H, Aoki J, Kanamori H, Ohashi K et al (2016) Comparable outcomes between autologous and allogeneic transplant for adult acute myeloid leukemia in first CR. Bone Marrow Transplant 51(5):645–653
Schmitz N, Truemper L, Bouabdallah K, Ziepert M, Leclerc M, Cartron G et al (2021) A randomized phase 3 trial of autologous vs allogeneic transplantation as part of first-line therapy in poor-risk peripheral T-NHL. Blood 137(19):2646–2656
Wang J, Duan X, Yang L, Liu X, Hao C, Dong H et al (2020) Comparison of Survival Between Autologous and Allogeneic Stem Cell Transplantation in Patients with Relapsed or Refractory B-Cell Non-Hodgkin Lymphoma: A Meta-Analysis. Cell Transplant. 963689720975397
Dunbar EM, Buzzeo MP, Levine JB, Schold JD, Meier-Kriesche HU, Reddy V (2008) The relationship between circulating natural killer cells after reduced intensity conditioning hematopoietic stem cell transplantation and relapse-free survival and graft-versus-host disease. Haematol 93(12):1852–1858
Porrata LF, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, Nevala W et al (2016) Sustained natural killer cell recovery post-autologous peripheral blood hematopoietic stem cell transplantation predicts survival in non-Hodgkin’s lymphoma. Blood 128:4641
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A et al (2002) Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 295:2097–2100
Bednarski JJ, Zimmerman C, Berrien-Elliott MM, Foltz JA, Becker-Hapak M, Neal CC et al (2022) Donor memory-like NK cells persist and induce remissions in pediatric patients with relapsed AML after transplant. Blood 139(11):1670–1683
Choi I, Yoon SR, Park SY, Kim H, Jung SJ, Jang YJ et al (2014) Donor-derived natural killer cells infused after human leukocyte antigen-haploidentical hematopoietic cell transplantation: a dose-escalation study. Biol Blood Marrow Transplant 20(5):696–704
Devillier R, Calmels B, Guia S, Taha M, Fauriat C, Mfarrej B et al (2021) Phase I Trial of Prophylactic Donor-Derived IL-2-Activated NK Cell Infusion after Allogeneic Hematopoietic Stem Cell Transplantation from a Matched Sibling Donor. Cancers (Basel) 13(11)
Tschan-Plessl A, Kalberer CP, Wieboldt R, Stern M, Siegler U, Wodnar-Filipowicz A et al (2021) Cellular immunotherapy with multiple infusions of in vitro-expanded haploidentical natural killer cells after autologous transplantation for patients with plasma cell myeloma. Cytotherapy 23(4):329–338
Shah N, Li L, McCarty J, Kaur I, Yvon E, Shaim H et al (2017) Phase I study of cord blood-derived natural killer cells combined with autologous stem cell transplantation in multiple myeloma. Br J Haematol 177(3):457–466
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
International Non-Hodgkin's Lymphoma Prognostic Factors Project (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329(14):987–994
Fehniger TA, Cai SF, Cao X, Bredemeyer AJ, Presti RM, French AR et al (2007) Acquisition of murine NK cell cytotoxicity requires the translation of a pre-existing pool of granzyme B and perforin mRNAs. Immunity 26(6):798–811
NCI National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), , 2021 Available from: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E et al (2014) Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol 32(27):3059–3068
Nguyen R, Wu H, Pounds S, Inaba H, Ribeiro RC, Cullins D et al (2019) A phase II clinical trial of adoptive transfer of haploidentical natural killer cells for consolidation therapy of pediatric acute myeloid leukemia. J Immunother Cancer 7(1):81
Dolstra H, Roeven MWH, Spanholtz J, Hangalapura BN, Tordoir M, Maas F et al (2017) Successful Transfer of Umbilical Cord Blood CD34(+) Hematopoietic Stem and Progenitor-derived NK Cells in Older Acute Myeloid Leukemia Patients. Clin Cancer Res 23(15):4107–4118
Vela M, Corral D, Carrasco P, Fernandez L, Valentin J, Gonzalez B et al (2018) Haploidentical IL-15/41BBL activated and expanded natural killer cell infusion therapy after salvage chemotherapy in children with relapsed and refractory leukemia. Cancer Lett 422:107–117
Björklund AT, Carlsten M, Sohlberg E, Liu LL, Clancy T, Karimi M et al (2018) Complete Remission with Reduction of High-Risk Clones following Haploidentical NK-Cell Therapy against MDS and AML. Clin Cancer Res 24(8):1834–1844
Ciurea SO, Schafer JR, Bassett R, Denman CJ, Cao K, Willis D et al (2017) Phase 1 clinical trial using mbIL21 ex vivo-expanded donor-derived NK cells after haploidentical transplantation. Blood 130(16):1857–1868
Luevano M, Daryouzeh M, Alnabhan R, Querol S, Khakoo S, Madrigal A et al (2012) The unique profile of cord blood natural killer cells balances incomplete maturation and effective killing function upon activation. Hum Immunol. 73:248–257
Dalle JH, Menezes J, Wagner E, Blagdon M, Champagne J, Champagne MA et al (2005) Characterization of cord blood natural killer cells: implications for transplantation and neonatal infections. Pediatr Res. 57:649–655
Berrien-Elliott MM, Foltz JA, Russler-Germain DA, Neal CC, Tran J, Gang M et al (2022) Hematopoietic cell transplantation donor-derived memory-like NK cells functionally persist after transfer into patients with leukemia. Sci Transl Med 14(633):eabm1375
Cooley S, He F, Bachanova V, Vercellotti GM, DeFor TE, Curtsinger JM et al (2019) First-in-human trial of rhIL-15 and haploidentical natural killer cell therapy for advanced acute myeloid leukemia. Blood Adv 3(13):1970–1980
Acknowledgements
We would like to thank all of the participants in this study, include patients, nurses, and laboratory technicians for their contributions.
Author information
Authors and Affiliations
Contributions
T.L. designed and guild the clinical research. Q.C. guild the expansion of CB-NK cells products., YL.W., J.J.,Q.C., and T.L. interpreted the data. Y.W., X.L., expand CB-NK cells. P.K., X.C., J.J., Z.L., J.L, and T.D. treated patients. YL.W. and T.L. analyzed the data and wrote the paper. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was reviewed and approved by the Ethics Committees of West China Hospital, Sichuan University, and was registered on the Clinical Trial Registry (clinicaltrials.gov, NCT05250362). Written informed consent was obtained from all patients.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Y., Wang, Y., Ji, J. et al. A pilot study of cord blood-derived natural killer cells as maintenance therapy after autologous hematopoietic stem cell transplantation. Ann Hematol 102, 3229–3237 (2023). https://doi.org/10.1007/s00277-023-05471-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05471-4