Abstract
Acute myeloid leukemia (AML) is a malignant lymphohematopoietic tumor that ranks among the most frequent indications for allogeneic hematopoietic stem cell transplantation (allo-HSCT). This article aims to provide a comprehensive analysis of the application of allo-HSCT for AML and identify prognostic factors to enhance future treatment effect. This retrospective study collected data from 323 patients diagnosed with AML at Peking University First Hospital who underwent allo-HSCT between September 2003 and July 2022. The annual number of transplantations has steadily increased. Our center has observed a rise in the proportion of cytogenetic high-risk and measurable residual disease (MRD) positive patients since 2013, as well as an increase in the number of haploidentical transplantations. The overall leukocyte engraftment time has decreased over the past 20 years. Furthermore, both overall survival (OS) and disease-free survival (DFS) have significantly improved, while non-relapse mortality (NRM) has significantly decreased since 2013. Multivariate analysis identified transplantation before 2013, patients in complete remission (CR) 2 or non-CR, and recipients older than 50 years as risk factors for NRM, while patients in non-CR and patients with positive MRD are risk factors for recurrence. These findings offer insights into AML treatment outcomes in China, highlighting changes in transplantation practices and the need to reduce post-transplant relapse. Effective interventions, such as MRD monitoring and risk stratification schemes, are crucial for further enhancing transplant outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative option for non-M3 acute myeloid leukemia (AML), but its potential is limited by treatment-related complications, relapse after transplantation, and the availability of suitable donors. Over the past 20 years, the feasibility of allo-HSCT has remarkably expanded due to major improvements in transplantation procedures [1,2,3]. However, given the remarkably complex diversity of AML, appropriate risk stratification and effective treatments are necessary to enhance overall survival and reduce transplantation-related complications.
Our previous studies typically focused on a specific aspect of allo-HSCT, and there is a lack of comprehensive research on the implementation of AML allo-HSCT. As obtaining a complete picture is essential for enriching our understanding of allo-HSCT, we conducted a large retrospective study to comprehensively analyze the evolution and outcomes of allo-HSCT for AML over the past 20 years in our transplant center. We aim to identify prognostic factors and offer insights for future refinements through this study.
Methods
Study population
This study retrospectively collected data from 323 patients diagnosed with AML who received allo-HSCT between September 2003 and July 2022. The patients were then followed up until April 2023 and were classified according to the WHO classification of hematolymphoid tumors [4]. Standard-dose “3+7” induction chemotherapy or priming chemotherapy was administered before transplantation.
Definitions
Complete remission (CR) was defined as bone marrow blasts less than 5%, absence of circulating blasts, no extramedullary lesions, and recovery of blood counts. Relapse was defined as the presence of more than 5% blasts in patients who previously had a normal bone marrow (BM) or evidence of extramedullary leukemia. Cytogenetic risk was determined following the 2022 edition of the European Leukemia Net (ELN) recommendations for the diagnosis and management of AML [5]. Hematopoietic repopulation was determined based on the established criteria outlined by the European Society for Blood and Marrow Transplantation. These criteria mandated three consecutive days with leukocytes ≥1.0 × 10^9/L, neutrophils ≥0.5 × 10^9/L, and thrombocytes ≥20 × 10^9/L, without the need for any transfusions in the preceding 7 days. Disease-free survival (DFS) was defined as the time from diagnosis to relapse or death, while overall survival (OS) was defined as the time from diagnosis to death or the most recent follow-up. Non-relapse mortality (NRM) was defined as death without relapse. Acute graft-versus-host disease (aGVHD) grading was performed according to the International Bone Marrow Transplant Registry (IBMTR), and chronic graft-versus-host disease (cGVHD) was graded based on the National Institutes of Health (NIH) global severity of cGVHD criteria [6, 7]. Only patients who survived beyond 100 days post-transplant without relapse were included in the analysis of cGvHD.
Allo-HSCT in AML
The conditioning regimens used in this study were modified Bu/Cy and Bu/Flu, which are commonly recommended in China [8]. The specific conditioning protocols were as follows: cytarabine at a dose of 2 g/m2 per day for 3 days; busulfan administered intravenously at a dose of 3.2 mg/kg per day for 3 days, in combination with either cyclophosphamide at a dose of 1.8 g/m2 per day for 2 days or fludarabine at a dose of 50 mg for 3–6 days (total dose: 200 mg/m2) [9]. For elderly patients with multiple comorbidities and generally poor overall health, a reduced-intensity conditioning regimen is employed. Rabbit anti-thymocyte globulin (ATG) was administered for 3 days before transplantation, with a dosage of 7.5–10 mg/kg for patients with haploidentical or unrelated donors, and 0–5 mg/kg for patients with HLA identical sibling donors. Graft-versus-host disease (GvHD) prophylaxis included cyclosporin A (CsA), mycophenolate mofetil (MMF), and a short course of methotrexate (MTX) [10].
Minimal residual disease (MRD) monitoring
Monitoring of MRD includes techniques such as multiparameter flow cytometry (FCM), quantitative PCR, and detection of donor-recipient chimerism status. For cases without specific fusion gene markers, we typically perform sequential testing of the WT1 gene twice, with a 10- to 14-day interval between tests. The threshold for WT1 positivity is set at 0.6% (1.5% for children). Patients with WT1 expression exceeding 60% and >1.0% are more likely to experience hematological relapse. In patients with specific fusion genes, we monitor the corresponding fusion genes. A change from negative to positive or a continuous increase in copy number of the fusion gene is considered indicative of a high risk of relapse. 3-log MRD CBF fusion (RUNX1/RUNX1T1 and CBFβ-MYH11) transcripts reduction can be used to discriminate high-risk from low-risk patients [11]. Post-transplant bone marrow examinations are typically conducted at +1 month, +2 months, +3 months, +4 months, +6 months, +9 months, +12 months, +18 months, +24 months, +36 months, +48 months, and +60 months. For patients with detectable MRD, a retest is recommended within 2 weeks.
Statistical analysis
Between-group differences were assessed using the Pearson chi-squared test for categorical variables and the Student’s t-test for continuous variables. Univariate analysis was conducted using Gray’s method, and factors with a p-value less than 0.05 were included in the multivariate analysis. The multivariate analysis was performed using the Fine and Gray model. Cumulative incidences of OS, DFS, RR, NRM, aGvHD, and cGvHD were calculated using the Kaplan–Meier method and compared using the log-rank test. Statistical significance was defined as p < 0.05. All statistical analyses were conducted using R statistical software and the “survival” and “survminer” package (Comprehensive R Archive Network, TUNA, Tsinghua University, China).
Results
Patient characters
We retrospectively identified a cohort of 323 patients diagnosed with AML who received treatment at our institution. Figure 1 illustrates a consistent increase in the number of transplantations over the past two decades. Table 1 provides a summary of the baseline characteristics of the patients. Notably, there were no significant changes observed in terms of sex, white blood cell (WBC) count, platelet (PLT) count, hemoglobin (Hb) level, disease status, hematopoietic cell transplantation comorbidity index (HCT-CI), and conditioning regimen after the year 2013. However, there was a significant increase in the proportion of patients with positive MRD and high cytogenetic risk after the year 2013 (p-values of 0.003 and 0.018, respectively). The median number of chemotherapies administered prior to transplantation was 2 for AML secondary to myelodysplastic syndrome (MDS) and 3 for de novo AML. Furthermore, during the past 20 years, there was a notable increase in the percentage of haploidentical hematopoietic stem cell transplantations (haplo-HSCTs), accompanied by an elevation in the standard number of CD34+ cells used in the procedure.
Engraftment
In the subgroup of patients younger than 16 years, the engraftment rates for WBC and PLT were 100% and 97.7%, respectively. The median time to WBC engraftment was 12 days (range: 11 to 14 days), while the median time to PLT engraftment was 16 days (range: 12 to 22 days). Among different donor types, the median WBC engraftment time was 12 days for related haplo-HSCT, 13 days for matched sibling donor hematopoietic stem cell transplantation (MSD-HSCT), 11 days for matched unrelated donor hematopoietic stem cell transplantation (MUD-HSCT), and 17 days for umbilical cord blood (UCB) HSCT. Similarly, the median PLT engraftment time was 17 days for related haplo-HSCT, 15 days for MSD-HSCT, 18 days for MUD-HSCT, and 26 days for UCB-HSCT. Furthermore, there was a significant reduction in the median WBC engraftment time after the year 2013 (p-value < 0.001), indicating a shorter time for successful engraftment.
Transplantation complications
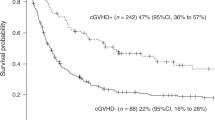
The incidence of grades II to IV aGVHD within 100 days post-transplantation was 25.5% (95% confidence interval [CI]: 20.5–30.2%). Specifically, it was 28.8% for related haplo-HSCT, 20.4% for MSD-HSCT, 19.4% for MUD-HSCT, and 14.3% for UCB-HSCT. The incidence of grades III to IV aGVHD within 100 days after transplantation was 13.9% (95% CI: 10.0–17.7%), with rates of 13.4% for related haplo-HSCT, 15.8% for MSD-HSCT, 12.9% for MUD-HSCT, and 14.3% for UCB-HSCT. Finally, the overall incidence of cGVHD at 1 year was 32.6% (95% CI: 26.6–38.1%), including rates of 30.4% for related haplo-HSCT, 40.8% for MSD-HSCT, 32.8% for MUD-HSCT, and 27.3% for UCB-HSCT. Figure 2 displays a comparison of the incidences of grades II to IV aGVHD, grades III to IV aGVHD, and cGVHD among different donor types. Notably, there were no significant changes in the incidence of grades II to IV aGVHD, grades III to IV aGVHD, or cGVHD over the past 20 years (Fig. 2).
Incidence of grades II to IV aGvHD, grades III to IV aGvHD and cGvHD according to donor type (a, b, c) and transplantation time (d, e, f). aGvHD, acute graft versus host disease; cGvHD, chronic graft versus host disease; MSD-HSCT, matched sibling donor hematopoietic stem cell transplantation; Haplo-HSCT, haploidentical donor hematopoietic stem cell transplantation; MUD-HSCT, matched unrelated donor hematopoietic stem cell transplantation; UCB, umbilical cord blood
Regarding infections, the overall incidence was 60.9%. This included 30 cases (9.3%) of bacterial combined fungal infection, 65 cases (20.1%) of simple fungal infection, 116 cases (35.9%) of simple bacterial infection, 12 cases of tuberculosis (3.7%), and 8 cases (2.5%) of Pneumocystis jirovecii pneumonia (PCP). Hemorrhagic cystitis was observed in 69 cases (21.4%). Within 100 days after transplantation, 186 cases (57.6%) experienced cytomegalovirus (CMV) reactivation. Additionally, there were 108 cases (33.4%) of Epstein-Barr virus (EBV) reactivation and 14 cases (4.3%) of post-transplant lymphoproliferative disease (PTLD).
Relapse
Out of the 323 patients in our study, 71 patients (22.0%) experienced relapse, with a median relapse time of 229 days (range: 42 to 1683 days) after transplantation. We observed a significant decrease in relapse rate after the year 2013 (p = 0.03), as illustrated in Fig. 3. Patients with positive MRD or without achieving CR before transplantation exhibited a significantly higher recurrence rate, as demonstrated in Figs. 4 and 5. Univariate analysis results are summarized in Table 2. Our multivariate analysis, which included disease stage, MRD status, and transplantation time, revealed that MRD positivity before transplantation had a significant influence on the relapse rate, with a HR of 3.0 (95% CI: 1.5 to 6; p = 0.002), as shown in Table 3.
Among the 71 patients who experienced relapse, 9 patients underwent prognostic donor lymphocyte infusion before hematologic relapse, and 6 patients received a second allo-HSCT. Remarkably, 16 relapse patients managed to survive after the relapse, with 14 of them experiencing relapse after the year 2013.
NRM
Out of the 323 patients, 49 patients (15.2%) experienced NRM. Specifically, 30 patients (12.6%) who were transplanted in CR1, 6 patients (24.0%) who were transplanted in CR2, and 13 patients (22.0%) who were transplanted in non-CR experienced NRM. The leading causes of NRM were infection (n = 28), GvHD (n = 14), bleeding (n = 3), and secondary tumors (n = 2). Notably, patients who underwent transplantation in CR1 and after the year 2013 had a reduced 5-year NRM, as shown in Figs. 3 and 5.
The univariate analysis results are summarized in Table 2. Multivariate analysis, which considered disease stage before transplantation, age, transplantation time, MNC, and donor/recipient gender, revealed that transplantation in CR2 and non-CR, transplantation before 2013 year, and recipients older than 50 years significantly increased NRM, as shown in Table 3.
Survival after transplantation
With a median follow-up period of 660 days (range: 1 to 4793 days), the estimated overall 5-year survival for the entire cohort was 68.4%. Notably, both the 5-year OS and DFS significantly increased after the year 2013, as illustrated in Fig. 3.
When considering disease stage before transplantation, transplantation time, age, HCT-CI, MRD and MNC, significant differences in 5-year survival were observed among the corresponding subgroups, as summarized in Table 2. Multivariate analysis identified disease status before transplantation, age, HCT-CI, and transplantation time as significant factors associated with OS, as shown in Table 3. The OS curves, stratified by disease status before transplantation, are presented in Fig. 5. Notably, for patients transplanted in CR1, the 1-year OS was 81.6% (95% CI, 76.8–86.8%), while for patients in CR2, the 1-year OS was 70.2% (95% CI, 53.8–91.6%). Conversely, patients transplanted in non-CR exhibited a lower 1-year OS of 53.7% (95% CI, 42.1–68.6%), as depicted in Fig. 5.
One-year DFS rates were as follows: 77.8% (95% CI, 72.6–83.4%) for patients in CR1, 65.2% (95% CI, 48.2–88.3%) for patients in CR2, and 53.1% (95% CI, 41.3–68.1%) for patients in non-CR (Fig. 5). Univariate analysis results are summarized in Table 2. Disease stage before transplantation, age, HCT-CI, transplantation time, and MRD before transplantation were included in the multivariate analysis. The multivariate analysis revealed a significant decrease in DFS for patients transplanted in non-CR and before 2013 year.
Discussion
Allo-HSCT has played a crucial role in the treatment of AML other than acute promyelocytic leukemia (APL) over the past 20 years. This study presents a comprehensive analysis of medical records from Peking University First Hospital spanning the last two decades, reflecting the development and evolution of the transplantation field in China. The study also identifies important prognostic factors for transplantation that hold potential for clinical application.
Our findings highlight significant changes in transplantation practices over the past two decades. Since 2013, there has been a notable increase in high-risk AML patients with MRD. This can be attributed to advancements in molecular biology and cytogenetics risk stratification, as well as the availability of more precise MRD detection methods. Donor types have also undergone substantial changes since 2013, with a decrease in MSD-HSCT from 36.3 to 15.5%, and a corresponding increase in haplo-HSCT from 37.4 to 75.4%. Compared to alternative transplantation methods, haplo-HSCT demonstrates similar survival rates, recurrence rates, and NRM. Additionally, there is no significant difference in the incidence of aGvHD and cGvHD, indicating the efficacy and safety of haplo-HSCT. Currently, main type of transplantation at our center is haplo-HSCT, which is related to the fact that most Chinese families are currently one-child families. Research has shown that the advantages of haplo-HSCT are as follows: (1) it is easier to find a donor, saving time; (2) cells are easily accessible, allowing high-risk patients to store reserves or undergo additional collections; (3) bone marrow or peripheral blood can be obtained as needed; (4) reduced risk of aGvHD in high-risk patients compared to MUD; (5) slightly higher incidence of aGvHD; (6) transplantation effectiveness is similar to MUD [12, 13]. Additionally, significant differences were observed in CD34+ cell count, graft source, and donor/recipient gender. These changes reflect the ongoing development of allo-HSCT from HLA-haploidentical related donors, with ongoing investigations focused on establishing optimal procedures [14]. One notable development in transplantation procedures is the refinement of criteria for allo-HSCT. Since 2013, our standard criteria have included a minimum total mononuclear cell (MNC) count of ≥10 × 10^8/kg and a CD34+ cell count of ≥5 × 10^8/kg. Multivariate analysis identified transplantation after 2013 as a protective factor for OS, DFS, and NRM, but not for relapse. This underscores the need to address the challenge of post-transplant recurrence to further improve transplant outcomes.
In this study, we investigated the impact of disease status and MRD before transplantation on relapse rates. The measurement of MRD in hematological neoplasms involving the bone marrow currently relies on highly sensitive methods capable of detecting specific genetic abnormalities using PCR-based techniques and next-generation sequencing, as well as tumor-associated immunophenotypic profiles through multiparametric flow cytometry (MFC) [11]. Previous studies have consistently demonstrated that achieving MRD negativity in patients with AML is associated with superior long-term survival. Consequently, it is suggested that MRD negativity should be considered as a clinical trial endpoint, enabling a more rapid evaluation of the efficacy of novel therapies [15, 16]. The valuable information obtained from MRD assessment has also been utilized in the design of personalized post-remission protocols and pre-emptive treatments for patients with sub-clinical relapse [17, 18]. These findings highlight the importance of incorporating MRD monitoring in the management of patients with hematological neoplasms undergoing allo-HSCT.
As disease status and MRD before transplantation have been identified as prognostic factors for relapse or DFS, it is important to consider post-transplant maintenance therapy for patients with positive MRD or non-CR before transplantation in order to reduce the risk of recurrence. In recent years, novel targeted drugs, such as hypomethylating agents, FLT3 inhibitors, and venetoclax, have been investigated as potential options for post-transplant maintenance therapy in AML patients. For some high-risk recurrent patients, our treatment center is currently attempting the application of the combination of Azacitidine and Venetoclax for post-transplant maintenance therapy. Preliminary results suggest that this regimen shows a trend towards improved survival. For patients with combined FLT3-ITD and IDH mutations, who are also in a refractory relapsed state or MRD-positive before transplantation, our center uses post-transplant maintenance therapy with targeted medications.
Retrospective and small-sample prospective studies have shown that maintenance therapy with hypomethylating agents like azacytidine and decitabine can be safe and effective in reducing relapse rates [19, 20]. However, conflicting findings have been reported regarding the benefit of hypomethylating agents as maintenance therapy in AML patients [21]. Additionally, sorafenib, a multi-kinase inhibitor, has demonstrated efficacy in treating FLT3-ITD AML and has been explored as a maintenance therapy option post-transplantation [22]. More recently, studies have indicated that venetoclax, a selective small molecular inhibitor of B-cell lymphoma-2 (Bcl-2), is well-tolerated as a post-transplant maintenance therapy for AML patients and may reduce relapse rates, particularly in high-risk patients. Prior studies have indicated that patients with AML carrying IDH mutations exhibit a suboptimal response to conventional chemotherapy, coupled with an elevated rate of relapse. Notably, in recent times, oral inhibitors targeting mutant IDH1 and IDH2, such as ivosidenib and enasidenib, have demonstrated promising clinical outcomes for individuals with relapsed/refractory or newly diagnosed IDH-mutated AML [23]. These emerging therapies hold promise for improving outcomes in AML patients undergoing allo-HSCT [24].
Currently, there is no consensus on the optimal timing of AML allo-HSCT. Numerous studies consistently demonstrate that patients with active disease have worse outcomes compared to those transplanted in CR [25]. However, patients transplanted in CR with incomplete count recovery (CRi) have inferior outcomes, primarily due to increased NRM rather than relapse risk [26]. The number of courses of consolidation chemotherapy administered prior to transplant has also shown no improvement in patient outcomes [27]. In our study, post-remission chemotherapy before allo-HSCT did not yield better results either. Our multivariate analysis identified disease status before transplantation, transplantation time, age, and HCT-CI before transplantation as factors associated with OS. Notably, transplantation in CR2 and non-CR, as well as recipients older than 50 years, significantly increased NRM. Therefore, we propose a selection strategy to identify patients who should undergo allo-HSCT in CR1 based on the risks of relapse and concomitant NRM [28]. According to our findings, young and well-fit patients with a high relapse risk are more likely to benefit from allo-HSCT at CR1, and the use of novel targeted drugs before transplantation should be considered to decrease MRD and improve prognosis.
Moreover, NRM accounted for 49% of deaths, with infection and GvHD being the top two causes. Therefore, efforts should be made to explore strategies for reducing NRM. In our study, we investigated the addition of decitabine to the conditioning regimen in 111 AML patients in order to alleviate GvHD while preserving the graft-versus-leukemia effect. Our previous study demonstrated that a decitabine-containing regimen may significantly reduce or alleviate GvHD without increasing the risk of relapse [29]. Building upon these findings, we are currently conducting prospective clinical research on the decitabine conditioning regimen. Additionally, infection was identified as another major cause of NRM. Since only a small number of AML patients (5 cases) in our hospital underwent reduced-intensity conditioning (RIC) regimen over the past two decades, RIC may be explored as a potential approach to reduce NRM and improve OS in the future. Currently, studies comparing the survival outcomes of RIC and myeloablative conditioning (MAC) allo-HSCT in AML patients have not reached definitive conclusions [30]. Some researchers have reported a non-significant increase in 5-year OS with RIC conditioning [31].
In this retrospective study, we analyzed data from 323 AML patients treated at our hospital over the past two decades. Our findings suggest that reducing relapse rates could be a crucial factor in significantly improving long-term survival. Patients with positive MRD and those not achieving CR before transplantation may benefit from prophylactic treatments, such as maintenance therapy. However, it is important to note that this study has certain limitations, including its retrospective nature and potential patient heterogeneity, as well as the lack of detailed data on certain variables.
Conclusion
In conclusion, our study provides a comprehensive overview of the significant changes observed in the practice of allo-HCT for AML patients over the past two decades in our hospital. Our data underscore the persistent challenge of post-transplant relapse, which must be addressed for the successful outcomes of allo-HSCT. Implementing effective therapeutic interventions, such as MRD monitoring and risk stratification schemes, holds promise for further improving transplant outcomes.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bernasconi P, Borsani O (2021) Eradication of measurable residual disease in AML: a challenging clinical goal. Cancers (Basel) 13(13). https://doi.org/10.3390/cancers13133170
Shi W, Jin W, Xia L, Hu Y (2020) Novel agents targeting leukemia cells and immune microenvironment for prevention and treatment of relapse of acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation. Acta Pharm Sin B 10(11):2125–2139. https://doi.org/10.1016/j.apsb.2020.06.012
Yang G, Wang X, Huang S, Huang R, Wei J, Wang X, Zhang X (2022) Generalist in allogeneic hematopoietic stem cell transplantation for MDS or AML: epigenetic therapy. Front Immunol 13:1034438. https://doi.org/10.3389/fimmu.2022.1034438
Cree IA (2022) The WHO classification of haematolymphoid tumours. Leukemia 36(7):1701–1702. https://doi.org/10.1038/s41375-022-01625-x
Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, Ebert BL, Fenaux P, Godley LA, Hasserjian RP, Larson RA, Levine RL, Miyazaki Y, Niederwieser D, Ossenkoppele G, Röllig C, Sierra J, Stein EM, Tallman MS et al (2022) Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 140(12):1345–1377. https://doi.org/10.1182/blood.2022016867
Baumrin E, Loren AW, Falk SJ, Mays JW, Cowen EW (2022) Chronic graft-versus-host disease. Part II: disease activity grading and therapeutic management J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2022.12.023
DiMaggio E (2020) Acute graft-versus-host disease: emerging insights and updates into detection, prevention, and treatment. Pharmacotherapy 40(8):788–807. https://doi.org/10.1002/phar.2436
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, Liu D, Liu Q, Liu T, Jiang M, Ren H, Song Y, Sun Z, Wang J, Wu D, Zhou D, Zou P, Liu K, Huang X (2018) The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol 11(1):33. https://doi.org/10.1186/s13045-018-0564-x
Mo X-D, Kong J, Zhao T, Xu L-P, Zhang X-H, Liu D-H, Wang Y, Chen H, Yan C-H, Chen Y-H, Han W, Wang F-R, Wang J-Z, Liu K-Y, Huang X-J (2014) Extramedullary relapse of acute leukemia after haploidentical hematopoietic stem cell transplantation: incidence, risk factors, treatment, and clinical outcomes. Biol Blood Marrow Transplant 20(12):2023–2028. https://doi.org/10.1016/j.bbmt.2014.08.023
Lai Y-R, Chen Y-H, Hu D-M, Jiang M, Liu Q-F, Liu L, Hou J, Schwarzenberger P, Li Q-C, Zhang Z-M, Liu K-Y, Huang X-J (2014) Multicenter phase II study of a combination of cyclosporine a, methotrexate and mycophenolate mofetil for GVHD prophylaxis: results of the Chinese Bone Marrow Transplant Cooperative Group (CBMTCG). J Hematol Oncol 7:59. https://doi.org/10.1186/s13045-014-0059-3
Voso MT, Ottone T, Lavorgna S, Venditti A, Maurillo L, Lo-Coco F, Buccisano F (2019) MRD in AML: the role of new techniques. Front Oncol 9:655. https://doi.org/10.3389/fonc.2019.00655
Lv M, Chang Y-J, Huang X-J (2019) Update of the “Beijing Protocol” haplo-identical hematopoietic stem cell transplantation. Bone Marrow Transplant 54(Suppl 2):703–707. https://doi.org/10.1038/s41409-019-0605-2
Wang X, Huang R, Zhang X, Zhang X (2022) Current status and prospects of hematopoietic stem cell transplantation in China. Chin Med J 135(12):1394–1403. https://doi.org/10.1097/CM9.0000000000002235
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, Blaise D, Arcese W, Sociè G, Bourhis JH, Van Lint MT, Bruno B, Huynh A, Santarone S, Deconinck E, Mohty M, Nagler A (2018) Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica 103(8):1317–1328. https://doi.org/10.3324/haematol.2018.189258
Short NJ, Zhou S, Fu C, Berry DA, Walter RB, Freeman SD, Hourigan CS, Huang X, Nogueras Gonzalez G, Hwang H, Qi X, Kantarjian H, Ravandi F (2020) Association of measurable residual disease with survival outcomes in patients with acute myeloid leukemia: a systematic review and meta-analysis. JAMA Oncol 6(12):1890–1899. https://doi.org/10.1001/jamaoncol.2020.4600
Murdock HM, Kim HT, Denlinger N, Vachhani P, Hambley B, Manning BS, Gier S, Cho C, Tsai HK, McCurdy S, Ho VT, Koreth J, Soiffer RJ, Ritz J, Carroll MP, Vasu S, Perales M-A, Wang ES, Gondek LP et al (2022) Impact of diagnostic genetics on remission MRD and transplantation outcomes in older patients with AML. Blood 139(24):3546–3557. https://doi.org/10.1182/blood.2021014520
Platzbecker U, Middeke JM, Sockel K, Herbst R, Wolf D, Baldus CD, Oelschlägel U, Mütherig A, Fransecky L, Noppeney R, Bug G, Götze KS, Krämer A, Bochtler T, Stelljes M, Groth C, Schubert A, Mende M, Stölzel F et al (2018) Measurable residual disease-guided treatment with azacitidine to prevent haematological relapse in patients with myelodysplastic syndrome and acute myeloid leukaemia (RELAZA2): an open-label, multicentre, phase 2 trial. Lancet Oncol 19(12):1668–1679. https://doi.org/10.1016/S1470-2045(18)30580-1
Buccisano F, Maurillo L, Schuurhuis GJ, Del Principe MI, Di Veroli A, Gurnari C, Venditti A (2019) The emerging role of measurable residual disease detection in AML in morphologic remission. Semin Hematol 56(2):125–130. https://doi.org/10.1053/j.seminhematol.2018.09.001
Xuan L, Liu Q (2021) Maintenance therapy in acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation. J Hematol Oncol 14(1):4. https://doi.org/10.1186/s13045-020-01017-7
Gao L, Zhang Y, Wang S, Kong P, Su Y, Hu J, Jiang M, Bai H, Lang T, Wang J, Liu L, Yang T, Huang X, Liu F, Lou S, Liu Y, Zhang C, Liu H, Gao L et al (2020) Effect of rhG-CSF combined with decitabine prophylaxis on relapse of patients with high-risk MRD-negative AML after HSCT: an open-label, multicenter, randomized controlled trial. J Clin Oncol 38(36):4249–4259. https://doi.org/10.1200/JCO.19.03277
Maples KT, Sabo RT, McCarty JM, Toor AA, Hawks KG (2018) Maintenance azacitidine after myeloablative allogeneic hematopoietic cell transplantation for myeloid malignancies. Leuk Lymphoma 59(12):2836–2841. https://doi.org/10.1080/10428194.2018.1443334
Xuan L, Wang Y, Huang F, Jiang E, Deng L, Wu B, Fan Z, Liang X, Xu N, Ye J, Lin R, Yin C, Zhang Y, Sun J, Han M, Huang X, Liu Q (2018) Effect of sorafenib on the outcomes of patients with FLT3-ITD acute myeloid leukemia undergoing allogeneic hematopoietic stem cell transplantation. Cancer 124(9):1954–1963. https://doi.org/10.1002/cncr.31295
Kreidieh F, Abou Dalle I, Moukalled N, El-Cheikh J, Brissot E, Mohty M, Bazarbachi A (2022) Relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia: an overview of prevention and treatment. Int J Hematol 116(3):330–340. https://doi.org/10.1007/s12185-022-03416-
Wei Y, Xiong X, Li X, Lu W, He X, Jin X, Sun R, Lyu H, Yuan T, Sun T, Zhao M (2021) Low-dose decitabine plus venetoclax is safe and effective as post-transplant maintenance therapy for high-risk acute myeloid leukemia and myelodysplastic syndrome. Cancer Sci 112(9):3636–3644. https://doi.org/10.1111/cas.15048
Loke J, Buka R, Craddock C (2021) Allogeneic stem cell transplantation for acute myeloid leukemia: who, when, and how? Front Immunol 12:659595. https://doi.org/10.3389/fimmu.2021.659595
Innes AJ, Woolley P, Szydlo RM, Lozano S, Fernando F, Bansal D, Palanicawandar R, Milojkovic D, May PC, Nadal-Melsio E, Yebra-Fernandez E, Olavarria E, Apperley JF, Pavlů J (2020) Complete remission with incomplete count recovery (CRi) prior to allogeneic HCT for acute myeloid leukaemia is associated with a high non-relapse mortality. Leukemia 34(2):667–670. https://doi.org/10.1038/s41375-019-0572-z
Tallman MS, Rowlings PA, Milone G, Zhang MJ, Perez WS, Weisdorf D, Keating A, Gale RP, Geller RB, Laughlin MJ, Lazarus HM, Luger SM, McCarthy PL, Rowe JM, Saez RA, Vowels MR, Horowitz MM (2000) Effect of postremission chemotherapy before human leukocyte antigen-identical sibling transplantation for acute myelogenous leukemia in first complete remission. Blood 96(4):1254–1258
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhäuser M, Juliusson G, Råcil Z, Rowe JM, Russell N, Mohty M, Löwenberg B, Socié G, Niederwieser D, Ossenkoppele GJ (2012) The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol 9(10):579–590. https://doi.org/10.1038/nrclinonc.2012.150
Wang QY, Li Y, Liang ZY, Yin Y, Liu W, Wang Q, Dong YJ, Sun YH, Xu WL, Ren HY (2019) Decitabine-containing conditioning regimen for allogeneic hematopoietic stem cell transplantation in patients with intermediate- and high-risk myelodysplastic syndrome/acute myeloid leukemia: potential decrease in the incidence of acute graft versus host disease. Cancer Manag Res 11:10195–10203. https://doi.org/10.2147/CMAR.S229768
Sharma SK, Choudhary D, Doval D, Khandelwal V, Patel A, Setia R, Dadu T, Handoo A (2021) Myeloablative versus reduced intensity conditioning regimens for allogeneic hematopoietic stem cell transplant for acute myeloid leukemia and myelodysplastic syndrome: a retrospective analysis. Indian J Hematol Blood Transfus 37(3):472–478. https://doi.org/10.1007/s12288-020-01386-6
Song Y, Yin Z, Ding J, Wu T (2021) Reduced intensity conditioning followed by allogeneic hematopoietic stem cell transplantation is a good choice for acute myeloid leukemia and myelodysplastic syndrome: a meta-analysis of randomized controlled trials. Front Oncol 11:708727. https://doi.org/10.3389/fonc.2021.708727
Funding
This work was financially supported by the National Natural Science Foundation of China (No. 81970410); Beijing Natural Science Foundation (No. 7202203); The Beijing Municipal Science and Technology Commission (No. Z221100007422008); and Peking University First Hospital Scientific Research Seed Fund (No. 2021SF13).
Author information
Authors and Affiliations
Contributions
Conceptualization: YL, HYR, and YJD. Methodology: QYaW and ZYL; formal analysis and investigation: QYaW, NH, and YLL; writing — original draft preparation: QYaW; writing — review and editing: YL; supervision: QYunW, WL, YY, and BJW. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review board at Peking University First Hospital (No. 2023-332). Due to the retrospective nature of the study, the requirement for written informed consent was waived. All data used in this manuscript were anonymized to ensure patient confidentiality.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Q., Liang, Z., Ren, H. et al. Real-world outcomes and prognostic factors among patients with acute myeloid leukemia treated with allogeneic hematopoietic stem cell transplantation. Ann Hematol 102, 3061–3074 (2023). https://doi.org/10.1007/s00277-023-05429-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05429-6