Abstract
This observational study aimed to evaluate the prognostic significance of interim and final 18F-fluorodeoxyglucose positron emission tomography-computed tomography (PET/CT) responses to upfront autologous stem cell transplantation (ASCT) in patients with peripheral T cell lymphomas (PTCLs). A total of 118 patients, from two independent institutions, with newly diagnosed PTCLs were enrolled, and 96 of them were evaluated. PET/CT was assessed at diagnosis, and during and after the primary treatment. Clinical outcomes of interim and final PET/CT were compared between transplanted and non-transplanted patients. The responses of PET/CT were assessed based on visual analysis using the Deauville five-point scale (5-PS). Clinicopathological features of transplanted patients (n = 37) were similar to those of non-transplanted patients (n = 59). After a median follow-up of 60.8 months, only final PET/CT response based on 5-PS was the independent prognostic factor of survival outcome (P < 0.001; HR 8.215; 95% C.I. 2.97–22.72) in multivariate analysis. Interim PET/CT response did not have a differential potential for predicting progression-free survival (PFS). In 59 patients, with score 1 or 2 in final PET/CT, the PFS rate was not significantly different between transplanted and non-transplanted patients (P = 0.970). Moreover, among the 37 patients with final PET/CT response score of 3–4, the PFS rate was equally poor in both transplanted and non-transplanted patients (P = 0.178). Final PET/CT assessment, based on 5-PS, was an important prognostic parameter for primary treatment of PTCLs, regardless of upfront ASCT. Interim PET/CT response could not be an indicator to determine the requirement for upfront ASCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral T cell lymphoma (PTCL) is a rare malignancy accounting for 5% of all lymphoid neoplasms in the Western countries [1]. Compared with B cell lymphomas, PTCLs have more aggressive and dismal prognosis. Most patients with PTCLs are relatively older in age and usually present with advanced stages [2, 3]. Although cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP), and CHOP-like regimen are commonly used as a first-line chemotherapy, the outcome in PTCLs following conventional chemotherapy remains poor, except in anaplastic lymphoma kinase (ALK)-positive anaplastic large cell lymphomas (ALCLs) [4]. High-dose chemotherapy with autologous stem cell transplantation (HDT/ASCT) has represented a rescue option from the poor prognosis of PTCLs, with several prospective trials reporting its promising results [5,6,7,8]. However, the effectiveness of upfront ASCT in distinct T cell subtypes, optimal transplant timing during the clinical courses, and the available prognostic factors for predicting better outcomes still remain unclear.
To predict the prognosis of PTCLs, pretreatment prognostic indices such as International Prognostic Index (IPI) and Prognostic Index for T cell lymphoma (PIT) can be used [9, 10]. However, these prognostic scores do not reflect the individual therapeutic response. For Hodgkin’s lymphoma (HL) and diffuse large B cell lymphoma (DLBCL), many studies have demonstrated the prognostic value of interim positron emission tomography-computed tomography (PET/CT) response [11,12,13]. In an attempt to standardize the reporting criteria of interim or final PET/CT, Lugano classification suggested visual response criteria using the Deauville five-point scale (5-PS) [14].
Although several trials have suggested the prognostic value of interim or final PET/CT response in PTCLs, the data have not been consistent [15,16,17,18,19]. Moreover, data from the investigation of clinical impact of PET/CT scan in patients with PTCLs undergoing upfront ASCT is still lacking.
The current study aimed to investigate whether interim and final PET/CT response using 5-PS could have prognostic value in patients with PTCLs, who are eligible for upfront ASCT. Furthermore, we aimed to find specific patient groups that could benefit either from ASCT or from chemotherapy alone.
Patients and methods
Patients
This comparative, retrospective, and observational study was performed between January 2005 and December 2016. A total of 118 patients with newly diagnosed PTCL were enrolled and 96 eligible patients were evaluated. The main inclusion criteria for upfront ASCT were as follows: (1) age under 65 years, (2) histopathologically proven PTCLs, except ALK-positive ALCLs, (3) IPI > low-intermediate or PIT > group 1, except NK/T cell lymphoma, (4) patients who achieved a complete response (CR) or partial response (PR) after primary chemotherapy, (5) Eastern Cooperative Oncology Group (ECOG) performance status ≤ 2, (6) no severe concomitant disease, and (7) adequate cardiac, pulmonary, hepatic, and renal function. All patients underwent an initial CT and PET/CT scan at diagnosis, with subsequent CT and PET/CT after three or four cycles of CHOP/CHOP-like regimen or non-anthracycline-based chemotherapy, as well as after completion of primary chemotherapy. While 37 patients underwent upfront ASCT, 59 did not. All study participants had provided informed consent.
Treatment strategy
Most patients were treated with a total of 6 cycles of anthracycline- or non-anthracycline-based chemotherapy. The anthracycline-based chemotherapy regimen consisted of 750 mg/m2 cyclophosphamide intravenously (IV), 50 mg/m2 doxorubicin IV, 1.4 mg/m2 vincristine (maximum 2 mg) IV on day 1, 100 mg/m2 etoposide IV on days 1 through 2, and 100 mg prednisolone orally per day on days 1 through 5, every 21 days. Patients were re-staged with CT scan and PET/CT after three or four cycles of chemotherapy, and if initially involved, bone marrow (BM) was biopsied again. If PR or CR was found in the CT scan, patients received additional two to three cycles of chemotherapy until the final sixth course. Patients achieving PR or CR in the CT scan at the end of primary chemotherapy either underwent stem cell mobilization chemotherapy using cyclophosphamide 3 g/m2, followed by subsequent HDT and ASCT, or were kept under observation. Cyclophosphamide stem cell mobilization chemotherapy was conducted after 4 to 6 weeks from day 1 of the preceding course of chemotherapy. The uniform conditioning regimen consisted of administration of 0.8 mg/kg/day busulfan IV every 6 h, from days 1 to 3, 400 mg/m2 etoposide IV on days 3 and 4, and 50 mg/kg cyclophosphamide IV on days 5 and 6. Stem cell sources in all cases were obtained from peripheral blood [20]. ASCT was conducted at a median of 7.2 weeks (interquartile range, 5.2–8.7 weeks) after final PET/CT.
Procedure and response assessment of PET/CT
All patients underwent PET/CT at diagnosis, mid-treatment, and at the completion of primary chemotherapy. Interim PET/CT was performed after three or four cycles of chemotherapy. After a total of 6 cycles of primary chemotherapy, a final PET/CT was performed. Interim and final PET/CT were scheduled a minimum of 2 weeks from the last treatment. If granulocyte colony stimulating factor (G-CSF) was administered, PET/CT was scanned after a minimum of 48 h from the last G-CSF injection. 18F-fluorodeoxyglucose (FDG) PET/CT was performed using a Discovery ST PET/CT system (GE Healthcare), consisting of a bismuth germanate full scanner and a 16-detector row CT scanner. The patients fasted for at least 6 h prior to the intravenous administration of 18F-FDG (7.4 MBq per body weight) to ensure a serum glucose level below 7.2 mmol/L. At 60 min after 18F-FDG administration, transmission data were acquired using low-dose CT (120 kV, automated from 10 to 130 mA, 512 × 512 matrix, 50-cm field of view (FOV), 3.75-mm slice thickness, and a rotation time of 0.8 s), extending from the base of the skull to the proximal thighs. Immediately after CT acquisition, PET emission scans were acquired in the same anatomic locations with a 15.7-cm axial FOV acquired in the two-dimensional mode using a 128 × 128 matrix. CT data were used for correction of attenuation. The responses of PET/CT were assessed by visual analysis using 5-PS [21].
Statistical analysis
Statistical analyses were performed using SPSS software (version 23.0). The primary endpoint was progression-free survival (PFS) and the secondary endpoint was overall survival (OS), since the clinical courses after progression or relapse were not evaluated here. PFS was defined from the date of diagnosis to disease progression, relapse, and death due to any cause, or the date of last follow-up for surviving patients. OS was defined as the period beginning at diagnosis up to the date of the last follow-up or death from any cause. PFS and OS were estimated using the Kaplan-Meier method. Log-rank test was used to compare the survival rates according to PET/CT response. Cox regression models and log-rank tests were used to analyze the univariate and multivariate impacts of various prognostic factors. A P value < 0.05 was considered statistically significant.
Results
Patient characteristics and treatment outcome
A total of 118 patients were screened for eligibility from two institutions. Of them, 22 patients were excluded (inadequate treatment response, n = 11; withdrawal of consent, n = 4; insufficient follow-up data, n = 7) and 96 were finally analyzed. Baseline characteristics of the 96 eligible patients are presented in Table 1. Patients with (n = 37) and without upfront ASCT (n = 59) had similar clinicopathological features. The median age was 47.6 years (range, 37.6–57.6 years) and 48.9 years (range, 36.9–60.9 years) with nodal PTCL incidence of 23 (60.0%) and 29 (47.4%) for the transplanted and non-transplanted patients, respectively. Advanced stage (III and IV) was presented by 22 patients with transplant (56.4%) and 27 without transplant (47.4%) at the time of diagnosis. In the transplanted group, 29 patients (74.4%) were classified as low/low-intermediate risk according to the IPI, and 28 (71.8%) were classified as group 1 or 2 by the PIT at diagnosis. Similarly, 34 patients (59.6%) were classified in the low/low-intermediate risk group, according to IPI, and 36 (63.2%) were classified as group 1 or 2 by PIT, among the non-transplanted group. After a median follow-up of 60.8 months, the disease had progressed in 42 (43.8%) of 96 patients while 30 (31.3%) patients had expired.
Deauville score and survival outcomes
To evaluate the impact of interim or final PET/CT response on survival outcome, we analyzed PFS (primary endpoint) of all patients, from both transplanted and non-transplanted groups, according to interim and final PET/CT response based on 5-PS. At the interim assessment, 25 patients (26%) were classified with score 1, 21 (21.9%) with score 2, 19 (19.8%) with score 3, and 31 (32.3%) with score 4. In the final PET/CT assessment, 35 patients (36.5%) were classified with score 1, 24 (25%) with score 2, 22 (22.9%) with score 3, and 15 (15.6%) with score 4. There was no patient with PET/CT response of score 5 in our cohorts, since the study included only patients who had achieved PR or CR after primary chemotherapy.
When we analyzed PFS of our cohorts by interim and final response using 5-PS, it was found to be well discriminated (Fig. 1a, b). After a median follow-up of 60.8 months, the 5-year PFS of patients with interim PET/CT response score 1 and 2 were 76% and 74.1%, respectively. These rates were significantly different from those in patients with interim PET/CT response scores 3 and 4 (28.4%; P < 0.05 and 35.8%; P < 0.05, respectively). Likewise, when we evaluated the 5-year PFS according to the final PET/CT response, that of patients with a final response score 2 (49.9%) was well discriminated from that of patients with final response score 3 (23.9%, P < 0.05). Therefore, we re-categorized the patients into two response groups: good response (score 1–2) and poor response (score 3–4) groups based on 5-PS. The significant differences of PFS and OS, between these two groups, in interim and final PET/CT, are showed in supplementary Figures 1 and 2.
Prognostic factors for survival outcomes
Univariate analysis showed PFS to be significantly associated with age (P = 0.022), stage (P = 0.030), lactate dehydrogenase (LDH) (P = 0.001), IPI (P = 0.002), PIT (P = 0.005), and interim (P = 0.001) and final PET/CT response using 5-PS (P < 0.001). On multivariate analysis, only final PET/CT response using 5-PS (P < 0.001; hazard ratio (HR) 8.215; 95% confidence interval (CI) 2.97–22.72) remained significantly associated with PFS (Table 2).
OS was associated with stage (P = 0.016), ECOG performance score (P = 0.028), LDH (P < 0.001), IPI (P = 0.001), PIT (P = 0.005), and interim (P = 0.014) and final PET/CT response using 5-PS (P = 0.014) in univariate analysis. In multivariate Cox regression analysis, significant prognostic factors for OS included IPI (P = 0.017; HR 4.501; 95% CI 1.312–15.447) and final PET/CT response using 5-PS (P < 0.001; HR 10.75; 95% CI 3.164–36.520) (Table 2).
PET/CT response and autologous stem cell transplantation
To identify the group of patients that could benefit from upfront ASCT, survival analysis according to transplantation was performed in each PET/CT subgroup. Based on interim PET/CT responses, using 5-PS, in 46 patients with interim response scores 1–2, PFS and OS of the ASCT group were found not significantly different from those of the non-ASCT group (P = 0.661, Fig. 2a; P = 0.708, Fig. 3a). In addition, the PFS and OS of 50 patients with interim response scores 3–4 did not show significant difference between the transplanted and non-transplanted patients (P = 0.324, Fig. 2b; P = 0.302, Fig. 3b).
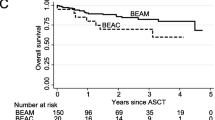
According to the response assessment based on final PET/CT using 5-PS, there was no survival benefit with respect to upfront ASCT. In the 59 patients with final response scores 1–2, PFS and OS did not present a statistically significant difference between the transplanted and non-transplanted patients (P = 0.97, Fig. 2c; P = 0.955, Fig. 3c). Among the 37 patients with final response scores 3–4, PFS of patients with upfront ASCT was not discriminated significantly compared with that of non-transplanted patients (P = 0.178, Fig. 2d), although it seemed to have better outcomes in upfront transplanted group. Additionally, the OS rates of patients with or without the upfront transplantation were similar among patients with final PET/CT response scores 3–4 (P = 0.766, Fig. 3d).
Discussion
PET/CT has become an important tool in the management of patients with FDG-avid lymphoma, including DLBCL and HL [22, 23]. However, the role of PET/CT in PTCL remains unclear. Recent studies have evaluated the role of interim and final PET/CT in PTCLs. A retrospective study by El-Galaly et al. had suggested that interim 5-PS > 3 is not prognostic for worse OS and PFS across CHOP/CHOP-like regimen-treated patients with nodal PTCL. In contrast, final 5-PS > 3 was associated with poor prognosis [15]. Tomita et al. had also demonstrated retrospectively that a positive final PET/CT result predicted worse outcome in PTCLs [17]. However, unlike the aforementioned finding by El-Galaly, Pellegrini et al. had reported positive interim PET/CT response to be predictive of poor PFS and OS in 34 patients with PTCLs [18].
In the current study, we collected clinical data of patients with newly diagnosed PTCLs from two institutions. Our cohorts either underwent upfront ASCT or were observed after achieving PR or CR. Clinical characteristics and histological distributions were similar between the transplanted and non-transplanted patients. In multivariate analysis, final PET/CT response by 5-PS was identified as an independent prognostic factor for PFS and OS. Final PET/CT response score ≥ 3 was significantly associated with disease progression and death. However, interim PET/CT response using 5-PS did not show prognostic significance for PFS and OS in multivariate analysis. In terms of OS, IPI was also predictive of better survival.
Upfront ASCT has been proposed as a promising consolidative option to improve the outcome of patients with PTCLs. A large prospective study with Nordic Lymphoma Group had reported superior 5-year OS (51%) and 5-year PFS (44%) in patients with PTCL and HDT/ASCT, compared with that in the conventional group [8]. Another prospective German study had analyzed 111 patients with PTCL and ASCT, and the 5-year OS, DFS, and PFS were 44%, 54%, and 39%, respectively [24]. However, these reports are limited to patients with PR or CR after initial therapy, and the cohorts of these studies had relatively favorable clinical characteristics for eligibility of transplantation. In addition, there has been no randomized prospective trial comparing conventional chemotherapy alone with upfront ASCT. Therefore, the actual role of upfront ASCT in PTCLs is yet to be clearly defined.
According to our data, the procedure of consolidative upfront ASCT was not associated with better PFS or OS in multivariate analysis. An Italian study analyzing 209 patients with PTCL had also suggested upfront ASCT to not be able to predict prognosis [25]. However, these results should be interpreted carefully, since some patients may still benefit from upfront ASCT. We analyzed the role of interim or final PET/CT in selecting patients that could benefit from upfront ASCT. When we evaluated survival outcome according to the transplantation in each subgroup, based on interim or final PET/CT response using 5-PS (within interim response of scores 1–2 or scores 3–4, and final response of scores 1–2 or scores 3–4, respectively), there was no specific beneficial subgroup.
There is a controversy regarding whether final response with score 3 could be considered as complete metabolic response (CMR). Although Lugano criteria had defined score 3 in 5-PS as CMR [23], several studies have suggested poor outcome of score 3 compared with that of score 1 or 2 in PTCLs other than HL, DLBCL, and follicular lymphoma. Yhim et al. had found patients with post-treatment score 3 or 4–5 to have worse PFS than those with score 1 or 2 in nodal PTCLs [26]. Furthermore, Kim et al. had demonstrated the final response scores 1–2 to be associated with better PFS and OS compared with score 3 or 4 in extranodal NK/T cell lymphoma in a retrospective study [27]. Similarly, in our data, PFS and OS of patients with scores 1–2 in interim and final PET/CT were significantly discriminated with those with scores 3–4. Moreover, in a retrospective study on nodal PTCLs by El-Galaly et al., 12 patients (71%) showed no FDG-uptake in BM among 17 with BM-positive biopsy [15]. This suggested that involvement of BM in PTCLs could be underestimated in PET/CT. These findings together suggest post-treatment PET/CT response with score 3 to possibly be considered as an incomplete response.
This study has certain limitations. Our study was retrospectively analyzed and PET/CT scans were obtained over a long period of time from two independent institutions. Different PET/CT machines and software products were used for response assessment. However, Biggi et al. had reported that concordance rates between reviewers were high when using 5-PS [28]. Like most PTCL studies, our cohort size was relatively small and provided limited information on the clinical course of patients with PTCLs who had achieved PR or CR after primary chemotherapy. Furthermore, we had interpreted PET/CT response using only 5-PS; other methods of PET/CT response assessment (e.g., quantitative analysis such as standardized uptake value or metabolic tumor volume) might show different data from our current study.
Despite these limitations, we first evaluated the prognostic utility of PET/CT response using 5-PS in PTCLs by comparing the treatment outcome between patients with upfront ASCT and with chemotherapy only. Our study showed the final PET/CT response based on 5-PS to be an independent prognostic factor of PTCLs, regardless of upfront ASCT. Patients with score ≥ 3, assessed by final PET/CT, had poor survival outcome despite upfront ASCT. Achieving score 1 or 2 in final PET/CT in patients with upfront ASCT is an important factor for PFS and OS. Unfortunately, we could not find a specific response group that could benefit from ASCT in the sub-analysis (within interim response of scores 1–2 and 3–4, within final response of scores 1–2 and 3–4). However, prospective comparative clinical trials with large cohorts would be necessary to define the role of PET/CT in PTCLs with upfront ASCT.
In conclusion, our study suggested the clinical outcome of PTCLs to be mainly reflected by final PET/CT response using 5-PS, regardless of upfront ASCT. According to our data, interim PET/CT response using 5-PS would not be an indicator to determine the requirement of upfront ASCT in patients.
References
Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS (2006) Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood 107:265–276. https://doi.org/10.1182/blood-2005-06-2508
Coiffier B, Brousse N, Peuchmaur M, Berger F, Gisselbrecht C, Bryon PA, Diebold J (1990) Peripheral T-cell lymphomas have a worse prognosis than B-cell lymphomas: a prospective study of 361 immunophenotyped patients treated with the LNH-84 regimen. The GELA (Groupe d'Etude des Lymphomes Agressives). Ann Oncol 1:45–50. https://doi.org/10.1093/oxfordjournals.annonc.a057673
Vose J, Armitage J, Weisenburger D, International TCLP (2008) International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol 26:4124–4130. https://doi.org/10.1200/JCO.2008.16.4558
Gascoyne RD, Aoun P, Wu D, Chhanabhai M, Skinnider BF, Greiner TC, Morris SW, Connors JM, Vose JM, Viswanatha DS, Coldman A, Weisenburger DD (1999) Prognostic significance of anaplastic lymphoma kinase (ALK) protein expression in adults with anaplastic large cell lymphoma. Blood 93:3913–3921
Corradini P, Tarella C, Zallio F, Dodero A, Zanni M, Valagussa P, Gianni AM, Rambaldi A, Barbui T, Cortelazzo S (2006) Long-term follow-up of patients with peripheral T-cell lymphomas treated up-front with high-dose chemotherapy followed by autologous stem cell transplantation. Leukemia 20:1533–1538. https://doi.org/10.1038/sj.leu.2404306
Mercadal S, Briones J, Xicoy B, Pedro C, Escoda L, Estany C, Camos M, Colomo L, Espinosa I, Martinez S, Ribera JM, Martino R, Gutierrez-Garcia G, Montserrat E, Lopez-Guillermo A, Grup per l'Estudi dels Limfomes de Catalunya IB (2008) Intensive chemotherapy (high-dose CHOP/ESHAP regimen) followed by autologous stem-cell transplantation in previously untreated patients with peripheral T-cell lymphoma. Ann Oncol 19:958–963. https://doi.org/10.1093/annonc/mdn022
Rodriguez J, Conde E, Gutierrez A, Arranz R, Leon A, Marin J, Bendandi M, Albo C, Caballero MD, Grupo Espanol de Linfomas/Trasplante Autologo de Medula O (2007) Frontline autologous stem cell transplantation in high-risk peripheral T-cell lymphoma: a prospective study from The Gel-Tamo Study Group. Eur J Haematol 79:32–38. https://doi.org/10.1111/j.1600-0609.2007.00856.x
d'Amore F, Relander T, Lauritzsen GF, Jantunen E, Hagberg H, Anderson H, Holte H, Osterborg A, Merup M, Brown P, Kuittinen O, Erlanson M, Ostenstad B, Fagerli UM, Gadeberg OV, Sundstrom C, Delabie J, Ralfkiaer E, Vornanen M, Toldbod HE (2012) Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01. J Clin Oncol 30:3093–3099. https://doi.org/10.1200/JCO.2011.40.2719
Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, Morabito F, Martelli M, Brusamolino E, Iannitto E, Zaja F, Cortelazzo S, Rigacci L, Devizzi L, Todeschini G, Santini G, Brugiatelli M, Federico M, Intergruppo Italiano L (2004) Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood 103:2474–2479. https://doi.org/10.1182/blood-2003-09-3080
Gutierrez-Garcia G, Garcia-Herrera A, Cardesa T, Martinez A, Villamor N, Ghita G, Martinez-Trillos A, Colomo L, Setoain X, Rodriguez S, Gine E, Campo E, Lopez-Guillermo A (2011) Comparison of four prognostic scores in peripheral T-cell lymphoma. Ann Oncol 22:397–404. https://doi.org/10.1093/annonc/mdq359
Gallamini A, Hutchings M, Rigacci L, Specht L, Merli F, Hansen M, Patti C, Loft A, Di Raimondo F, D'Amore F, Biggi A, Vitolo U, Stelitano C, Sancetta R, Trentin L, Luminari S, Iannitto E, Viviani S, Pierri I, Levis A (2007) Early interim 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography is prognostically superior to international prognostic score in advanced-stage Hodgkin's lymphoma: a report from a joint Italian-Danish study. J Clin Oncol 25:3746–3752. https://doi.org/10.1200/jco.2007.11.6525
Yang DH, Min JJ, Song HC, Jeong YY, Chung WK, Bae SY, Ahn JS, Kim YK, Bom HS, Chung IJ, Kim HJ, Lee JJ (2011) Prognostic significance of interim (1)(8)F-FDG PET/CT after three or four cycles of R-CHOP chemotherapy in the treatment of diffuse large B-cell lymphoma. Eur J Cancer 47:1312–1318. https://doi.org/10.1016/j.ejca.2010.12.027
Mikhaeel NG, Hutchings M, Fields PA, O’Doherty MJ, Timothy AR (2005) FDG-PET after two to three cycles of chemotherapy predicts progression-free and overall survival in high-grade non-Hodgkin lymphoma. Ann Oncol 16:1514–1523. https://doi.org/10.1093/annonc/mdi272
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, Lister TA, Alliance AL, Lymphoma G, Eastern Cooperative Oncology G, European Mantle Cell Lymphoma C, Italian Lymphoma F, European Organisation for R, Treatment of Cancer/Dutch Hemato-Oncology G, Grupo Espanol de Medula O, German High-Grade Lymphoma Study G, German Hodgkin’s Study G, Japanese Lymphorra Study G, Lymphoma Study A, Group NCT, Nordic Lymphoma Study G, Southwest Oncology G, United Kingdom National Cancer Research I (2014) Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol 32:3059–3068. https://doi.org/10.1200/JCO.2013.54.8800
El-Galaly TC, Pedersen MB, Hutchings M, Mylam KJ, Madsen J, Gang AO, Bogsted M, de Nully BP, Loft A, Nielsen AL, Hendel HW, Iyer V, Gormsen LC (2015) Utility of interim and end-of-treatment PET/CT in peripheral T-cell lymphomas: a review of 124 patients. Am J Hematol 90:975–980. https://doi.org/10.1002/ajh.24128
Ham JS, Kim SJ, Choi JY, Hyun SH, Choi SK, Kim HS, Lim SH, Lee JY, Jung SH, Ko YH, Kim WS (2016) The prognostic value of interim and end-of-treatment PET/CT in patients with newly diagnosed peripheral T-cell lymphoma. Blood Cancer J 6:e395. https://doi.org/10.1038/bcj.2016.2
Tomita N, Hattori Y, Fujisawa S, Hashimoto C, Taguchi J, Takasaki H, Sakai R, Tateishi U, Ishigatsubo Y (2015) Post-therapy (1)(8)F-fluorodeoxyglucose positron emission tomography for predicting outcome in patients with peripheral T cell lymphoma. Ann Hematol 94:431–436. https://doi.org/10.1007/s00277-014-2227-5
Pellegrini C, Argnani L, Broccoli A, Stefoni V, Derenzini E, Gandolfi L, Casadei B, Maglie R, Pileri S, Zinzani PL (2014) Prognostic value of interim positron emission tomography in patients with peripheral T-cell lymphoma. Oncologist 19:746–750. https://doi.org/10.1634/theoncologist.2013-0463
Jung SH, Ahn JS, Kim YK, Kweon SS, Min JJ, Bom HS, Kim HJ, Chae YS, Moon JH, Sohn SK, Lee SW, Byun BH, Do YR, Lee JJ, Yang DH (2015) Prognostic significance of interim PET/CT based on visual, SUV-based, and MTV-based assessment in the treatment of peripheral T-cell lymphoma. BMC Cancer 15:198. https://doi.org/10.1186/s12885-015-1193-1
Ahn JS, Yang DH, Jung SH, Chae YS, Sohn SK, Yhim HY, Kwak JY, Lee SR, Kim YK, Kim HJ, Lee JJ (2013) Autologous stem cell transplantation with busulfan, cyclophosphamide, and etoposide as an intensifying frontline treatment in patients with peripheral T cell lymphomas: a multicenter retrospective trial. Ann Hematol 92:789–797. https://doi.org/10.1007/s00277-013-1685-5
Meignan M, Gallamini A, Meignan M, Gallamini A, Haioun C (2009) Report on the first international workshop on interim-PET-scan in lymphoma. Leuk Lymphoma 50:1257–1260. https://doi.org/10.1080/10428190903040048
Hutchings M, Loft A, Hansen M, Pedersen LM, Berthelsen AK, Keiding S, D'Amore F, Boesen AM, Roemer L, Specht L (2006) Position emission tomography with or without computed tomography in the primary staging of Hodgkin’s lymphoma. Haematologica 91:482–489
Johnson SA, Kumar A, Matasar MJ, Schoder H, Rademaker J (2015) Imaging for staging and response assessment in lymphoma. Radiology 276:323–338. https://doi.org/10.1148/radiol.2015142088
Wilhelm M, Smetak M, Reimer P, Geissinger E, Ruediger T, Metzner B, Schmitz N, Engert A, Schaefer-Eckart K, Birkmann J (2016) First-line therapy of peripheral T-cell lymphoma: extension and long-term follow-up of a study investigating the role of autologous stem cell transplantation. Blood Cancer J 6:e452. https://doi.org/10.1038/bcj.2016.63
Gritti G, Boschini C, Rossi A, Delaini F, Grassi A, Algarotti A, Mico C, Trezzi R, Gianatti A, Barbui AM, Rambaldi A (2015) Primary treatment response rather than front line stem cell transplantation is crucial for long term outcome of peripheral T-cell lymphomas. PLoS One 10:e0121822. https://doi.org/10.1371/journal.pone.0121822
Yhim HY, Park Y, Han YH, Kim S, Kang SR, Moon JH, Jeong JH, Shin HJ, Kim K, Choi YS, Kim K, Kim MK, Kong E, Kim DS, Eo JS, Lee JH, Kang DY, Lee WS, Lee SM, Do YR, Ham JS, Kim SJ, Kim WS, Choi JY, Yang DH, Kwak JY (2018) A risk stratification model for nodal peripheral T-cell lymphomas based on the NCCN-IPI and posttreatment Deauville score. Eur J Nucl Med Mol Imaging 45:2274–2284. https://doi.org/10.1007/s00259-018-4093-1
Kim SJ, Choi JY, Hyun SH, Ki CS, Oh D, Ahn YC, Ko YH, Choi S, Jung SH, Khong PL, Tang T, Yan X, Lim ST, Kwong YL, Kim WS, Asia Lymphoma Study G (2015) Risk stratification on the basis of Deauville score on PET-CT and the presence of Epstein-Barr virus DNA after completion of primary treatment for extranodal natural killer/T-cell lymphoma, nasal type: a multicentre, retrospective analysis. Lancet Haematol 2:e66–e74. https://doi.org/10.1016/S2352-3026(15)00002-2
Biggi A, Gallamini A, Chauvie S, Hutchings M, Kostakoglu L, Gregianin M, Meignan M, Malkowski B, Hofman MS, Barrington SF (2013) International validation study for interim PET in ABVD-treated, advanced-stage hodgkin lymphoma: interpretation criteria and concordance rate among reviewers. J Nucl Med 54:683–690. https://doi.org/10.2967/jnumed.112.110890
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary fig. 1
Progress-free survival (PFS) according to (A) interim PET/CT and (B) final PET/CT response (PNG 291 kb)
Supplementary fig. 2
Overall survival (OS) according to (A) interim PET/CT and (B) final PET/CT response (PNG 309 kb)
Rights and permissions
About this article
Cite this article
Ahn, SY., Jung, SY., Jung, SH. et al. Prognostic significance of FDG-PET/CT in determining upfront autologous stem cell transplantation for the treatment of peripheral T cell lymphomas. Ann Hematol 99, 83–91 (2020). https://doi.org/10.1007/s00277-019-03867-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03867-9