Abstract
To investigate the effect of chronic graft-versus-host disease (cGVHD) on the outcomes of acute myeloid leukemia (AML) patients who relapsed after allogenic hematopoietic cell transplantation, we performed a retrospective analysis on 218 patients with a median follow-up of 21.4 (3.4–179.6) months. A total of 103 patients developed cGVHD, with a 2-year cumulative incidence of 48.9% (95% CI 42.1–55.7%). The estimated 3-year overall survival was 85.7% (95% CI 75.7–95.7%), 48.8% (95% CI 31.7–66.0%), and 54.1% (95% CI 44.3–63.8%) for patients with limited cGVHD, extensive cGVHD, and without cGVHD (P < 0.001). The 3-year event-free survival were 75.5% (95% CI 63.7–87.4%), 46.0% (95% CI 28.8–63.2%), and 45.0% (95% CI 35.6–54.4%) (P < 0.001), while the 3-year cumulative relapse rates were 22.8% (95% CI 11.0–34.6%), 11.6% (95% CI 5.3–22.6%), and 40.3% (95% CI 31.0–49.6%), respectively (P < 0.001). At the last evaluation, 62 patients relapsed with 17 patients having active cGVHD and 45 without. Compared to patients relapsing without cGVHD, patients who relapsed with cGVHD had a longer duration of remission and a better 2-year post-relapse survival [10.9 months (3.7–42.2) versus 4.4 months (2.2–28.3); P < 0.001]; [32.8% (95% CI 8.2–57.4%) versus 4.5% (95% CI 0–12.8%); P = 0.043]. For patients who relapsed with cGVHD, the remission rates were both 60% after salvage chemotherapy with or without donor lymphocyte infusion (P = 1.000). In conclusion, cGVHD may exert a stronger graft-versus-leukemia effect, which may decrease the post-transplantation relapse rate and may also benefit those patients who eventually relapsed after transplantation in terms of prolong post-relapse survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogenic hematopoietic stem cell transplantation (allo-HSCT) is a curative treatment for acute myeloid leukemia (AML) not only due to the eradication of leukemic cells by conditioning regimen, which is composed of high-dose chemotherapy or irradiation, but also due to the immune-mediated graft-versus-leukemia (GVL) effect. Most studies have shown lower incidence of disease relapse with the presence of chronic graft-versus-host disease (cGVHD) [1,2,3,4]. Although cGVHD is generally considered being associated with GVL effect, approximately 15–25% of patients relapse with active cGVHD [5, 6]. Thanarajasingam et al. reported that history of GVHD in AML patients relapsed after allo-HSCT is an adverse factor for post-relapse survival [7]. However, Schmid et al. found that acute GVHD (aGVHD) was an adverse factor, and cGVHD had no correlation with post-relapse survival [8]. The impact of cGVHD on post-relapse survival, especially the presence of active cGVHD at the time of relapse, is not clarified. Treatment for relapsed patients after allo-HSCT remains difficult. The treatment options include rapid tapering or stop of immunosuppression, donor lymphocyte infusions (DLI) with or without chemotherapy or second allo-HSCT [9]. It is more difficult for those patients relapsing with active cGVHD due to the risk of exacerbation of GVHD. To investigate the influence of cGVHD on relapse and survival after relapse, we performed a retrospective analysis of prognostic factors for the relapse rate and post-relapse overall survival (prOS) in 218 AML patients. We found that cGVHD is associated with improved prOS in AML patients. However, we failed to see the difference between salvage therapy with DLI or without for patients relapsing with cGVHD.
Patients and methods
Patients
In this retrospective analysis, a total of 228 AML patients received their first allo-HSCT from HLA-matched sibling, unrelated donor or haplo-identical related donor in Changhai Hospital or Ruijin Hospital between March 2001 and August 2015 were included. Among these 228 patients, 10 patients were excluded due to early death within 100 days after transplantation, and the remaining 218 patients were included in this retrospective analysis with a median follow-up time of 21.40 months (range 3.43 to 179.63 months). Detailed information about the patients and transplant characteristics are summarized in Table 1. All patients or their agents signed informed consent forms before transplantation.
Transplantation protocol
Of the 218 patients, a total of 111 patients received granulocyte colony-stimulating factor (G-CSF)-mobilized peripheral blood stem cells (PBSCs) from HLA-matched related donors, and the other 96 patients received PBSCs from HLA-matched unrelated donors (≥ 8/10 loci). The conditioning regimen included Cy-TBI (60 mg/kg/day IV cyclophosphamide on days − 5 to − 4; total body irradiation with 3 Gy twice daily on days − 3 to − 2); the BuCy regimen (0.8 mg/kg IV busulfan q6h on days − 8 to − 5 and 60 mg/kg/day IV cyclophosphamide on days − 4 to − 3); or the FBA regimen [10] (30 mg/m2/day IV fludarabine for 2 h on days − 10 to − 6; 1.5 g/m2/day IV cytarabine on days − 10 to − 6 started 4 h after fludarabine and continued for 3 h; and 0.8 mg/kg IV busulfan q6h on days − 5 to − 3). For 11 patients received haplo-identical donor transplantation with a modified BuCy conditioning regimen (4 g/m2/day IV cytarabine on days − 10 to − 9; 3.2 mg/kg/day IV busulfan on days − 8 to − 6; 1.8 g/m2/day IV cyclophosphamide on days − 5 to − 4; 250 mg/m2/day methyl chloride hexamethylene urea nitrate orally once on day − 3; and 5 mg/kg/day anti-thymocyte globulin-Fresenius or 2 mg/kg/day thymoglobulin IV on days − 5 to − 2) [11], G-CSF-mobilized PBSC and bone marrow stem cells were infused on day 0. For 13 refractory/relapse patients, sequential chemotherapy followed by reduced-intensity conditioning regimen (fludarabine 30 mg/m2 on days − 20 to − 16, cytarabine 2 g/m2 on days − 20 to − 16, and idarubicin 12 mg/m2 on days − 16 to − 14 followed by fludarabine 30 mg/m2 on days − 6 to − 2 and busulfan 3.2 mg/kg on days − 5 to − 3) [12] were given before related or unrelated donor transplantation. If an unrelated donor was used, the patient also received anti-thymocyte globulin (ATG) (Fresenius, Germany, 5 mg/kg/day, IV from days − 4 to − 1). All patients received cyclosporine, short-term methotrexate, and mycophenolate mofetil as GVHD prophylaxis [13]. DLI was recommended according to donor chimerism, minimal residual disease (MRD), and the presence of acute GVHD (aGVHD) or cGVHD. Prostaglandin E1 was used to prevent hepatic veno-occlusive disease. G-CSF was administered starting on day + 5 until neutrophil engraftment. All patients received blood products when necessary according to institutional guidelines. Fluconazole, ganciclovir, and sulfamethoxazole were used as infection prophylaxis from days − 10 to − 1 before transplantation. After neutrophil and platelet engraftment, the following drugs were administered individually in turn for 7 days, until the termination of immunosuppression, in the following sequence: fluconazole, ganciclovir, and sulfamethoxazole. When a suspected infection happened, appropriate antibiotics or antifungal agents were administered according to institutional guidelines.
Definitions and statistical analysis
Complete remission (CR) was defined as less than 5% blasts in the bone marrow and normalization of the peripheral blood count without circulating blasts. Relapse was defined according to cytological criteria as reappearance of leukemic blasts in the peripheral blood or the finding of equal to or more than 5% blasts in the bone marrow not attributable to other causes or extramedullary relapse (EMR). aGVHD and cGVHD were graded according to established criteria [14, 15]. Overall survival (OS) was defined as the time from transplantation to death. Event-free survival (EFS) was defined as the time from transplantation to relapse or death resulting from any cause. Post-relapse OS was defined as the time from relapse to death.
Wilcoxon’s rank sum test was used to compare continuous variables, and the chi-squared test was used to compare categorical variables. The cumulative incidences of relapse, transplant-related mortality (TRM), and GVHD were estimated using competing risk analysis with non-relapse mortality, with relapse and with death from any cause as competing risks. OS, prOS, and EFS were calculated by the Kaplan-Meier method and were compared using the log-rank test. Cox proportional hazard models were used to estimate hazard ratios with a 95% confidence interval (CI) for prognostic factors. When analyzing the influence of cGVHD on relapse and survival, the three patients who developed cGVHD after relapse and salvage DLI were both classified in the no-GVHD group. When analyzing the response for salvage therapies, these three patients were classified to the group of relapse without cGVHD, while comparing prOS between patients relapsing with or without cGVHD, these three patients were excluded. Patient characteristics that were significant in the univariate models at the 0.10 level were included in the multivariate analysis. A P value of 0.05 or less was considered statistically significant. SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA), and R 3.4.4 were used for data analysis.
Results
The overall HSCT outcomes
The 3-year OS, EFS, and cumulative incidence of relapse were 62.0% (95% CI 55.0–69.0%), 54.9% (95% CI 47.9–61.9%), and 30.2% (95% CI 23.7–36.7%) for the whole cohort. The 100-day cumulative incidence of grades II–IV aGVHD was 22.9% (95% CI 17.3-28.5%). A total of 103 patients developed cGVHD, including three cases that occurred after relapse; 65 cases were limited and 38 were extensive cGVHD. The organs involved are listed in Table 2. The 2-year cumulative incidence of cGVHD was 48.9% (95% CI 42.1-55.7%) and that of extensive cGVHD was 18.1% (95% CI 12.9-23.3%).
Impact of cGVHD on relapse
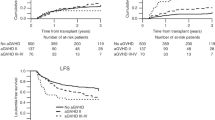
A total of 62 patients relapsed after allo-HSCT with a median time of 5.23 months (range 2.17 to 42.20 months). For patients with limited, extensive cGVHD, and without cGVHD, the cumulative 3-year OS were 85.7% (95% CI 75.7–95.7%), 48.8% (95% CI 31.7–66.0%), and 54.1% (95% CI 44.3–63.8%), respectively (P < 0.001) (Fig. 1a); the 3-year EFS were 75.5% (95% CI 63.7–87.4%), 46.0% (95% CI 28.8–63.2%), and 45.0% (95% CI 35.6–54.4%), respectively (P < 0.001) (Fig. 1b); and the 3-year cumulative relapse rates were 22.8% (95% CI 11.0–34.6%), 11.6% (95% CI 5.3–22.6%), and 40.3% (95% CI 31.0–49.6%) (Fig. 1c), respectively (P < 0.001). We analyzed the variables using the Cox proportional hazard model to identify risk factors for relapse. In the multivariate analysis, limited and extensive cGVHD were both related to decreased relapse rates [HR 0.40 (95% CI 0.21–0.77), P = 0.006; HR 0.33 (95% CI 0.13–0.82), P = 0.018] (Table 3).
Impact of cGVHD on prOS
A total of 42 patients relapsed without cGVHD all the time, 17 patients relapsed with active cGVHD (12 limited and 5 extensive cases), and 3 developed cGVHD after salvage DLI (detailed information in Table S1). In patients relapsed without cGVHD, only one (1/42) experienced isolated extramedullary involvement, while there were 8 (8/17) in patients relapsed with active cGVHD (P < 0.001). The 2-year prOS were 32.8% (95% CI 8.2–57.4%) for patients relapsing with active cGVHD (N = 17) and 4.5% (95% CI 0–12.8%) for patients without cGVHD (N = 42) (P = 0.043; Fig. 2). In the multivariate analysis, patients who relapsed with active cGVHD had superior prOS [HR 0.23 (95% CI 0.10–0.52), P < 0.001] (Table 4). Moreover, late relapse was also associated with superior prOS [HR 0.11 (95% CI 0.03–0.43), P = 0.001].
Post-relapse salvage therapy and the outcome
We also compared the remission rates after salvage therapy separately for patients who relapsed with active cGVHD and for patients without active cGVHD. Four patients relapsing without cGVHD (4/45) received supportive care only. Twenty-eight patients (28/45) in this group received DLI, and 15 achieved remission (53.6%), while only 2 of 13 patients (16.7%) who received chemotherapy or radiotherapy (13/45) achieved remission (P = 0.021). Three patients relapsing without cGVHD who received DLI developed cGVHD after salvage therapy, and all with sustained CR (3/15) and 2 of them (2/3) are still alive. Two patients in the group of those relapsing with cGVHD (2/17) received supportive care only. Three of five patients (60%) in this group achieved CR with DLI, while six of ten patients (60%) who received chemotherapy or radiotherapy achieved remission (P = 1.000).
Discussion
Advances in allogeneic stem cell transplantation have improved the safety of the procedure and significantly broadened its application during the past two decades. However, approximately 30~40% of AML patients receiving allo-HSCT will relapse, and their outcomes are generally dismal [16, 17]. Relapse remained as a leading cause of treatment failure in allo-HSCT setting [17,18,19]. Most studies have reported decreased relapse rate with the presence of cGVHD suggesting an association with GVL effect [1,2,3,4], while an analysis reported by our institution a few years ago failed to find the protective effect of cGVHD in relapse/refractory AML which most likely due to the limited number of patients involved [13]. As a result, for many years, the primary strategy for preventing and treatment of relapse after transplantation is to induce GVL effect in the expense of increased GVHD. Meanwhile, the impact of cGVHD occurring before relapse in those patients who eventually relapsed after allo-HSCT is still controversial. Our data showed that active cGVHD is a protective factor not only against relapse after allo-HSCT but also for prOS in AML patients. Schmid et al. reported no correlation between cGVHD and prOS based on the hypothesis of a close correlation between cGVHD and longer remission after transplantation [8]. However, we found that longer remission was also an independent protective factor for prOS, which was similar to the results of most of the previous studies [7, 20, 21]. This discrepancy may be due to the difference in conditioning regimens. Thanarajasingam et al. reported that a history of GVHD was an adverse factor for prOS [7]. However, their analysis did not separate the influences of aGVHD and cGVHD. In addition, the primary diseases they included were more heterogeneous. Another study from CIBMTR also reported GVHD as an adverse factor for AML patients relapsing after allo-HSCT [21]. The author speculated that the poor outcome for patients relapsing with active GVHD may be due to the preclusion of cell-based therapy and the increasing risk of infectious complications. In their study, the influences of aGVHD and cGVHD were also analyzed together. In the current study, we analyzed the influence of active cGVHD alone on relapse and prOS. We found more isolated extramedullary relapse and longer remission duration for patients relapsing with active cGVHD. In both univariate and multivariate analysis, active cGVHD and longer remission duration were protective factors for prOS, while relapse site had no significant influence. Patients relapsing with active cGVHD maybe had a stronger GVL effect which decreased marrow relapse and postponed time to recurrence. As a result, extramedullary relapse accounted for a larger proportion for these patients. Some studies have reported better prOS for patients with isolated extramedullary relapse compared with those had bone marrow involvement [22,23,24]. So, the better prognosis for patients relapsing with active cGVHD may be associated with stronger GVL effect at least in bone marrow. Furthermore, the relatively higher relapse rate after transplantation in the current study compared with other reports may be attributed to the higher proportion of late stage disease status before transplantation.
Treatment for patients who relapse with active cGVHD is more complicated since the attempts to enhance the GVL effect are usually associated with aggravation of cGVHD. We found that patients who relapsed without cGVHD may benefit from DLI after intensive chemotherapy in comparison with those with cGVHD. Although no definite conclusion could be drawn from this observation due to the limited number of patients, the influence of DLI on patients relapsing with cGVHD deserves further verification in larger cohorts in the future.
The limitation of this study was the retrospective nature with limited number of patients actually relapsed after allo-HSCT. There was variation of donor type, and conditioning regimens with lack of MRD data in patients made it difficult to reach solid conclusion. But, our data still provide evidence to support the association of cGVHD with GVL effect in AML patients undergoing allo-HSCT in terms of significant reduced relapse rate. The protective effect was also observed in patients relapsed with active cGVHD. Though DLI may have limited role in the treatment of these patients, the overall survival after relapse was better than patients relapsed without active cGVHD. These findings are worth to verify in a larger cohort of patients.
References
Signori A, Crocchiolo R, Oneto R, Sacchi N, Sormani MP, Fagioli F, Rambaldi A, Ciceri F, Bacigalupo A (2012) Chronic GVHD is associated with lower relapse risk irrespective of stem cell source among patients receiving transplantation from unrelated donors. Bone Marrow Transplant 47(11):1474–1478
Weiden PL, Sullivan KM, Flournoy N, Storb R, Thomas ED, The Seattle Marrow Transplant Team (1981) Antileukemic effect of chronic graft-versus-host disease: contribution to improved survival after allogeneic marrow transplantation. N Engl J Med 304:1529–1533
Gustafsson Jernberg A, Remberger M, Ringdén O, Winiarski J (2003) Graft-versus-leukaemia effect in children: chronic GVHD has a significant impact on relapse and survival. Bone Marrow Transplant 31(3):175–181
Kato M, Kurata M, Kanda J, Kato K, Tomizawa D, Kudo K, Yoshida N, Watanabe K, Shimada H, Inagaki J, Koh K, Goto H, Kato K, Cho Y, Yuza Y, Ogawa A, Okada K, Inoue M, Hashii Y, Teshima T, Murata M, Atsuta Y (2018) Impact of graft-versus-host disease on relapse and survival after allogeneic stem cell transplantation for pediatric leukemia. Bone Marrow Transplant 54:68–75. https://doi.org/10.1038/s41409-018-0221-6
Sullivan KM, Weiden PL, Storb R, Witherspoon RP, Fefer A, Fisher L, Buckner CD, Anasetti C, Appelbaum FR, Badger C (1989) Influence of acute and chronic graft-versus-host disease on relapse and survival after bone marrow transplantation from HLA-identical siblings as treatment of acute and chronic leukemia. Blood 73(6):1720–1728
Ozawa S, Nakaseko C, Nishimura M, Maruta A, Cho R, Ohwada C, Sakamaki H, Sao H, Mori SI, Okamoto S, Miyamura K, Kato S, Kawase T, Morishima Y, Kodera Y, for the Japan Marrow Donor Program (2007) Chronic graft-versus-host disease after allogeneic bone marrow transplantation from an unrelated donor: incidence, risk factors and association with relapse. A report from the Japan marrow DonorProgram. Br J Haematol 137(2):142–151
Thanarajasingam G, Kim HT, Cutler C, Ho VT, Koreth J, Alyea EP, Antin JH, Soiffer RJ, Armand P (2013) Outcome and prognostic factors for patients who relapse after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 19(12):1713–1718
Schmid C, Labopin M, Nagler A, Niederwieser D, Castagna L, Tabrizi R, Stadler M, Kuball J, Cornelissen J, Vorlicek J, Socie G, Falda M, Vindelov L, Ljungman P, Jackson G, Kroger N, Rank A, Polge E, Rocha V, Mohty M, on behalf of the Acute Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT) (2012) Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensityconditioning for allogeneic stem cell transplantation. Blood 119(6):1599–1606
Wang Y, Chen H, Chen J, Han M, Hu JD, Jiong Hu, Huang H, Lai Y, Liu D, Liu Q, Liu T, Jiang M, Ren H, Song Y, Sun Z, Wang C, Wang J, Wu D, Xu K, Zhang X, Xu L, Liu K, Huang X (2018) The consensus on the monitoring, treatment, and prevention of leukemia relapse after allogeneic hematopoietic stem cell transplantation in China. Cancer Lett 438:63–75. https://doi.org/10.1016/j.canlet.2018.08.030
Zhang WP, Wang ZW, Hu XX, Chen J, Yang D, Song XM, Gao L, Ni X, Chen L, Xia XX, Zhou H, Tang GS, Cheng H, Luo YR, Li HM, Yang JM, Wang JM (2018) Preconditioning with fludarabine, busulfan and cytarabine versus standard BuCy2 for patientswith acute myeloid leukemia: a prospective, randomized phase II study. Bone Marrow Transplant 19. https://doi.org/10.1038/s41409-018-0356-5
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, Fan ZP, Wu DP, Huang XJ (2015) Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood 125:3956–3962
Tang W, Fan X, Wang L, Hu J (2015) Busulfan and fludarabine conditioning regimen given at hematological nadir of cytoreduction fludarabine, cytarabine, and idarubicin chemotherapy in patients with refractory acute myeloid leukemia undergoing allogeneic stem cell transplantation: a single arm pilot consort study. Medicine (Baltimore) 94(15):e706
Zhang WP, Yang D, Song XM, Ni X, Chen J, Chen L, Yang JM, Zhou H, Cheng H, Liu BH, Li HM, Wang JM (2013) Allogeneic peripheral blood stem cell transplantation is a promising and safe choice for the treatment of refractory/relapsed acute myelogenous leukemia, even with a higher leukemia burden. Biol Blood Marrow Transplant 19(4):653–660
Glucksberg H, Storb R, Fefer A et al (1974) Clinical manifestations of graft-versus-host disease in human recipients of marrow from HLA-matched sibling donors. Transplant 18:295–304
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, Hackman R, Tsoi MS, Storb R, Donnall Thomas E (1980) Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 69(2):204–217
Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, Sorror ML, Horowitz MM, Bolwell B, Rizzo JD, Socié G (2011) Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol 29(16):2230–2239
Tsirigotis P, Byrne M, Schmid C, Baron F, Ciceri F, Esteve J, Gorin NC, Giebel S, Mohty M, Savani BN, Nagler A (2016) Relapse of AML after hematopoietic stem cell transplantation: methods of monitoring and preventive strategies. A review from the ALWP of the EBMT. Bone Marrow Transplant 51(11):1431–1438
Shah MV, Jorgensen JL, Saliba RM, Wang SA, Alousi AM, Andersson BS, Bashir Q, Ciurea SO, Kebriaei P, Marin D, Patel KP, Popat UR, Rezvani K, Rondon G, Shpall EJ, Champlin RE, Oran B (2018) Early post-transplant minimal residual disease assessment improves risk stratification in acute myeloid leukemia. Biol Blood Marrow Transplant 24:1514–1520
Ma YR, Xu LP, Zhang XH, Yan CH, Wang Y, Wang FR, Wang JZ, Chen Y, Han W, Chen YH, Chen H, Liu KY, Huang XJ (2017) Comparable post-relapse outcomes between haploidentical and matched related donor allogeneic stem cell transplantation. Bone Marrow Transplant 52(3):409–414
Bejanyan N, Oran B, Shanley R, Warlick E, Ustun C, Vercellotti G, Verneris M, Wagner JE, Weisdorf D, Brunstein C (2014) Clinical outcomes of AML patients relapsing after matched- related donor and umbilical cord blood transplantation. Bone Marrow Transplant 49(8):1029–1035
Bejanyan N, Weisdorf DJ, Logan BR, Wang HL, Devine SM, de Lima M, Bunjes DW, Zhang MJ (2015) Survival of AML patients relapsing after allogeneic hematopoietic cell transplantation: a CIBMTR study. Biol Blood Marrow Transplant 21(3):454–459
Shem-Tov N, Saraceni F, Danylesko I, Shouval R, Yerushalmi R, Nagler A, Shimoni A (2017) Isolated extramedullary relapse of acute leukemia after allogeneic stem cell transplantation: different kinetics and better prognosis than systemic relapse. Biol Blood Marrow Transplant 23(7):1087–1094
Ge L, Ye F, Mao X, Chen J, Sun A, Zhu X, Qiu H, Jin Z, Miao M, Fu C, Ma X, Chen F, Xue S, Ruan C, Wu D, Tang X (2014) Extramedullary relapse of acute leukemia after allogeneic hematopoietic stem cell transplantation: different characteristics between acute myelogenous leukemia and acute lymphoblastic leukemia. Biol Blood Marrow Transplant 20(7):1040–1047
Clark WB, Strickland SA, Barrett AJ, Savani BN (2010) Extramedullary relapses after allogeneic stem cell transplantation for acute myeloid leukemia and myelodysplastic syndrome. Haematologica 95(6):860–863
Funding
This study is supported by the National Natural Science Foundation of China (NSFC 81530047, 81270638, 81090413) and Science and Technology Commission of Shanghai Municipality (08JC1406500, 05DZ19327) to JMW.
Author information
Authors and Affiliations
Contributions
ZWW collected and verified patient information, analyzed the data, and wrote the manuscript. CRY collected and verified patient information. JMW and JH designed the study, wrote, and modified the manuscript. All other authors involved in treatment of the patients. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 74.5 kb)
Rights and permissions
About this article
Cite this article
Wang, Z., Yin, C., Zhang, W. et al. The benefit of chronic graft-versus-host disease in patients with acute myeloid leukemia relapsed after allogeneic stem cell transplantation. Ann Hematol 98, 1765–1773 (2019). https://doi.org/10.1007/s00277-019-03682-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03682-2