Abstract
We report our decennial experience with 1161 newly-placed long-term central venous catheters inserted in 919 hematology-oncology patients for a total of 413,901 CVC-days of observation. Most of the CVCs were partially-implanted, open-ended, Broviac-Hickman type of CVC (95 %). One thousand and twenty-four complications were recorded equal to 2.47 per 1000 CVC-days. The frequency of complications per CVC, the rate of episodes per 1000 CVC-days, and removal rate were malfunction/occlusion 42 %, 1.18/1000, and 2.3 %; mechanical (dislodgement/rupture/kinking) 18.3 %, 0.51/1000, and 77.4 %; bacteremia 14.8 %, 0.42/1000, and 18.6 %; exit-site/tunnel infection 11.5 %, 0.32/1000, and 9.7 %; thrombosis 0.86 %, 0.02/1000, and 30 %; pneumothorax 0.52 %, 0.01/1000, and 0. In multivariate analysis, the risk factors were for mechanical complications, a younger age <6.1 years at CVC insertion (HR 1.8, p = 0.0006); for bacteremia, a double lumen CVC (HR 3.1, p < 0.0001) and the surgical modality of CVC insertion (HR 1.5, p = 0.03); for exit-site/tunnel infection, a double lumen CVC (HR 2.1, p = 0.0003) and a diagnosis of leukemia or lymphoma (HR 1.8, p = 0.01); for malfunction/occlusion, an age <6.1 years (HR 1.6, p = 0.0003), the diagnosis of leukemia or lymphoma (HR 1.9, p < 0.0001) and double lumen CVC (HR 1.33, p = 0.023). The cumulative incidence of premature CVC removal was 29.2 % and the risk factors associated with this event were the surgical modality of CVC insertion (HR 1.4, p = 0.0153) and an age at CVC positioning less than 6.1 years (HR 1.6, p = 0.0025). We conclude that a best-practice set of rules resulted in reduced CVC complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of long-tem central venous catheters (CVCs) several decades ago represented one of the major advances in the quality of care of oncology patients, in particular for pediatric patients [1, 2]. The use of partially or totally implanted devices permits the safe administration of chemotherapy schedules requiring continuous infusion or high doses of drugs, hyperhydration, hyperosmolar solutions for parenteral nutrition, and intensive supportive care or blood testing [3]. Partially implanted CVCs are often preferred by the pediatric hematologist-oncologist because this CVC is more suitable for complex oncological and supportive treatment than a totally implanted CVC, especially in the youngest patients, and their use does not require skin puncture at every new access [4–6].
Despite the fact that the adoption of a CVC to deliver intravenous therapies is nowadays considered the standard of care in an oncology setting, its use exposes the patient to complications that can cause hospitalization or be life-threatening requiring its early removal [7, 8]. Mechanical and infection complications such as occlusion, dislodgment, rupture, bacteremia, and tunnel exit-site infection are the main causes of hospitalization for patient treatment and/or for premature removal of the CVC [4, 9]. In order to prevent CVC complications, every team involved in CVC management must define the standard procedures to adopt during CVC life and periodically re-assess them to evaluate their efficacy and the need for modification [10].
Our center adopted written procedures and set up educational programs to improve CVC standard care more than 10 years ago and, thereafter, decided to monitor their efficacy by a prospective recording of complication episodes year by year. We present here the results of this 10-year data collection that is the largest pediatric series so far reported on the incidence and type of complication of a partially implanted CVC and on the frequency of premature loss of the CVC due to complications.
Patients and methods
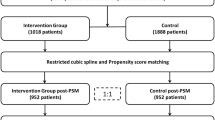
The study included prospectively all the pediatric and adolescent patients, aged 0 to 18 years, affected by malignant or non-malignant hematology or oncology diseases who needed the positioning of long-term, partially or totally implantable, tunneled, open-ended, CVCs for chemotherapy or hematopoietic stem cell transplantation (HSCT) purposes. The study period was from January 1st 2000 to December 31st 2009 whereas the follow-up data are as at December 31st 2011.
Signed informed consent was obtained by the parents both for CVC insertion and the anonymous use of patient demographic and clinical data for research purposes in accordance with Italian privacy policy. The study was approved by the local ethics committee. This comprehensive analysis also included data on 129 and 203 CVCs previously reported in two different reports [6, 9]. The study was part of an internal program of implementation of the policies for daily CVC maintenance care, and for prevention and treatment of CVC complications. The study was preceded by the preparation of common written center policies for CVC management by a multidisciplinary committee composed of nurses, pediatric hematologist, pediatric surgeon, anesthetist, and infectivologist. The methodology used to define CVC policies was based on three steps: (1) review of literature available as of 2000, (2) revision by discussion of internal procedures already existing, and (3) writing the revised policies and presentation to all components of the team. The prospective collection of data regarding type and number of CVCs and their complications was adopted as an internal method of monitoring the efficacy of interventions. The tools used for this purpose were (a) a form recording the characteristics of any CVC inserted (type, vessel incannulated, body site, CVC French, number of lumens, early complications) with the essential patient demographic and clinical information (age, sex, diagnosis, indication for CVC, phase of therapy); this form was completed by a trained nurse in the first week after CVC positioning and transferred to a database by a data manager; (b) common written policies regarding medication of the CVC exit-site, CVC maintenance flushing, and modality to check the CVC functioning at every use; these instructions were adopted by all of the nursing team working in the stem cell transplant unit, hematology and oncology inpatient and outpatient clinics, and also illustrated and distributed to doctors and nurses of referral network hospitals that cooperate in treating the patients; (c) a form recording complications by type (infection, thrombosis, malfunctioning) filled in by nurses or physicians who first made the diagnosis.
CVC insertion and maintenance care
The CVC was inserted in the operating theater by an experienced pediatric anesthetist or surgeon who used a percutaneous or open cutdown approach according to standard procedures [9, 11]. The open cut was preferred to the percutaneous approach in patients at major risk of bleeding complications or pneumothorax such as (a) those requiring daily platelet transfusion to maintain a count >50 × 109/L, (b) a second or third insertion, or, (c) in case of failure of vein cannulation by percutaneous technique. From January 2005, both techniques were modified by introducing the Sri Paran method to improve the fixation of the CVC to the chest wall [12] while the blind percutaneous venipuncture (landmark venipuncture) was substituted by ultrasound-guided venipuncture from 2007 [13]. No perioperative antimicrobial prophylaxis was adopted for CVC implantation.
CVC maintenance care was handled by trained pediatric nurses and consisted of flushing the CVC with 3 mL of normal solution and heparin 200 IU/mL twice a week by using a standard CVC cap. This procedure differed only in 101 patients who constituted the experimental arm of a randomized study on two different modalities of flushing CVCs performed at our center from January 2003 to January 2005. That study compared flushing with normal saline at least weekly (experimental arm), by using a positive-pressure CVC valve cap device (CLC 2000, ICU Medical Inc), versus flushing with normal saline and heparin (control arm) at least two times a week [9]. The skin care at CVC exit remained constant for the whole study period and consisted of weekly cleansing of the CVC exit-site with a 10 % povidone-iodine solution followed by covering with a sterile gauze dressing. Moreover, strict aseptic techniques and scrupulous hand hygiene were observed always in positioning and handling the CVC. Table 1 shows the main rules put into practice by our procedures.
After CVC insertion, the parents and/or patients received a diary in which every flushing, exit-site medication, and complication of the CVC was dated, described, and signed by the health personnel, i.e., nurse or physician who performed the assessment, made the diagnosis of the complication, performed the intervention, or prescribed the treatment. This diary and, for completeness of data, the clinical charts were reviewed by a trained nurse on each admission to, or discharge from, the ward or outpatient clinic to check that any CVC complications were captured. Data on CVC complications, i.e., date, type of CVC, type of complication, treatment, and outcome were recorded on a specific form and were signed by the trained nurse. All CVC complication forms were reviewed by the data managers for completeness and consistency before storage into the database and analysis of the results.
Definition and management of CVC-related complications
A standard approach to the diagnosis and treatment of a CVC-related infection was adopted.
CVC exit-site infection
We set up a visual score to define the severity of CVC exit-site infection and to guide the intervention. The score comprised four steps of severity, from 0 to 3, as indicated in Fig. 1. CVC exit-site infection was managed according to the algorithm showed in Fig. 2. Any CVC exit-site infection was treated more frequently, i.e., every 1 to 2 days, by cleansing the CVC exit-site with povidone-iodine solution and changing the sterile dressing. Topical antibiotic treatment was performed, if needed, according to the results of the skin swab culture. The exit-site infection was monitored visually and microbiologically, if the swab was positive initially, until resolution or for at least 7 days, before a decision to remove the CVC was made.
Tunnel infection
This included any inflammation that extended more than 2 cm beyond the CVC exit-site or along the CVC subcutaneous tunnel. Diagnostic procedures included taking a skin swab and CVC-blood cultures. This complication required prompt empiric antibiotic treatment that was continued for at least 3 days before deciding whether or not to remove the CVC or until resolution.
CVC-associated bacteremia or fungemia
This was defined as one or more blood cultures positive for bacteria or fungus obtained through a CVC in patients with fever (>38 °C) or other signs of infection, i.e., chills or hypotension. According to our standard practice, all febrile patients were investigated with one set of blood cultures obtained from each CVC lumen and peripheral vein; in case of inability to access a peripheral vein (severe hypotension or shock, infant baby, obesity), two sets of blood cultures were drawn from the CVC after a time interval of 15–30 min. Subsequently, they were treated promptly with empiric antibiotics, i.e., the combination of teicoplanin and a third-generation cephalosporin (mainly ceftazidime or cefipime); amikacin was added in the case of severe neutropenia (polymorphonuclear [PMN] cells <0.5 × 109/L) [8]. Adjustments were made, if necessary, according to the sensitivity testing on the organisms isolated from the blood culture. The treatment was continued until resolution of the infection or for at least 3 days before deciding whether or not to remove the CVC, or immediately in case of CVC-related septic shock.
Mechanical complications
These included dislocation of the CVC tip or external migration of the cuff, fracture, or accidental CVC self-removal by the patient. The diagnostic evaluation was based on the visual and manual assessment of the position of the Dacron cuff and a chest X-ray or line contrast study with enhancement medium to rule out CVC dislodgement, breakage, or leakage. A fracture of the external part of the CVC was repaired whenever possible; otherwise, the CVC was removed if it was a fracture of the internal portion of the CVC.
Malfunction
This diagnosis was based on difficulty, i.e., partial occlusion or complete occlusion resulting in inability to withdraw blood and/or infuse liquids through the CVC despite postural changes and in the absence of thrombosis or other mechanical complications. Treatment was based on one or two administration(s) of 10,000 IU of urokinase left in the CVC lumen for 2 h [9, 14, 15]. Sudden onset of CVC malfunction during or immediately after the infusion of drugs, blood components, or parenteral nutrition was considered a result of the precipitation of crystals or the formation of microaggregates among the infused components. In these cases, alcohol or hydrochloric acid was used, as reported elsewhere [16]. If urokinase and/or alcohol or hydrochloric acid failed to restore CVC patency, the CVC was removed.
CVC-related thrombosis
When suggested by clinical symptoms, i.e., swelling, pain, or pulmonary embolism, color-Doppler ultrasound, computed tomography, or magnetic resonance imaging was used for the noninvasive diagnosis of CVC-related thrombosis. Treatment was based on published guidelines for antithrombotic therapy in cancer patients [17].
Statistical analysis
Descriptive statistics were reported for the main demographic and clinical characteristics of patients as well as type of CVC and CVC complications. Median and range were used in case of continuous data, frequency, and percentage in case of discrete variables.
Cumulative incidence of mechanical complications, malfunction, exit-site and tunnel infection, CVC-associated bacteremia, CVC-related thrombosis, and pneumothorax was calculated only for the first CVC and estimated from the date of CVC insertion to the date of complication or to the date of latest follow-up. CVC survival was also calculated considering the time elapsed from CVC insertion to CVC premature removal due to complication or the date of the last follow-up.
The Kaplan-Meier method was used and differences between groups were compared by log-rank test. Impact of the main host- or CVC-related characteristics (gender, age at insertion, type of diagnosis, type of vessel accessed, body side of CVC access, modality of insertion, and number of lumen) on the different types of complications and on premature removal of the CVC was analyzed. After verifying the assumption of proportional hazards, univariate and multivariate Cox regression models were estimated taking into account the first event. If several recurrent complication episodes occur, an extension of the Cox proportional hazards model for recurrent events (the PWP Gap-time model) was applied [18]. Hazard rate (HR), 95 % CI, and two-sided p values were calculated. The level of significance was set at α < 0.05.
Results
Over a 10-year period, 919 patients (57.3 % males and 42.7 % females) were included in the study: 538 patients (58.5 %) were affected by leukemia or lymphoma, while 381 patients (41.5 %) were affected by solid tumor or non-malignant disease. A total of 1161 newly placed long-term CVCs were inserted for a total of 413,901 CVC-days of observation. The vast majority of CVCs were partially implanted, open-ended, Broviac-Hickman type CVC (95 %). Table 2 lists main patient and CVC characteristics.
Overall, 1024 complications were recorded, which was equivalent to 2.47 per 1000 CVC-days. Table 3 lists the types of complication, their incidence, and the removal rate. The incidence of complications ranged from 0.5 % for pneumothorax to 42 % for malfunction/occlusion, respectively. The malfunction/occlusion episodes were 488 and occurred at a median time of 75 days from insertion of CVC, range 0–1303. They were classified as malfunction for the difficulty to withdraw blood or infuse solutions through the CVC in 292 episodes (60 %) and as complete CVC occlusion in 192 episodes (39 %). In four cases, the type of malfunction was not reported. Despite their high frequency, malfunction/occlusion complications were managed successfully in most cases and, therefore, were associated with a very low rate of CVC removal (2.3 %). Conversely, mechanical complications, affecting 18.3 % of CVCs, were associated with the highest premature removal rate (77.4 %) and represented 74 % of all CVCs removed due to complications (164 of 223). Mechanical complications, classified as dislocation (80 %), fracture (16 %), kinking (4 %), occurred at a median time of 61 days, range 0–818 from insertion. In six cases (3 %), these episodes happened early, by 48 h from insertion.
Bacteremia affected 14.8 % of CVCs and caused a CVC removal rate of 18.6 %. Among the 172 episodes, 107 (62 %) were caused by Gram positive, 49 (28 %) were caused by Gram negative, two (1 %) were polimicrobial Gram positive/Gram negative and twelve (7 %) were fungemias, unknown in two cases. These episodes occurred at a median time of 98 days, range 0–1297, from insertion of CVC. Among the Gram positive bacteria, the most frequent strain was Staphylococcus epidermidis and among the Gram negative bacteria, the most frequent strain was Escherichia coli. The list of all bacteria cultured from the blood is shown in Table 4.
Exit-site/tunnel infection affected 11.5 % of CVCs and resulted in a removal rate of 9.7 %. There were 134 episodes of exit-site infection which were diagnosed at a median time from CVC insertion of 62 days, range 2–640. According to our score, they were classified as grade 1 in 38 episodes, grade 2 in 69 episodes, grade 3 in 18 episodes, whereas the score was not known in 9 episodes. The CVC removal rate was higher in grade 3 exit-site/tunnel infection (28 %) vs. episodes with grade 1 or 2 (3 %), p = 0.001.
CVC thrombosis and post-insertion pnemothorax were the least frequent complications, 0.86 % and 0.52 % respectively, but thrombosis, although rare, was associated with the highest CVC removal rate of 30 %.
Incidence and risk factor analysis
The cumulative incidence of mechanical complications was 24.5 % (95 % CI 20.7, 28.8). A younger age <6.1 years at CVC insertion was the only risk factor for the occurrence of mechanical complications: HR 1.8 (CI 1.3–2.4), p = 0.0006. Second or further events occurred in only 16 of the total episodes (8 %); thus, no recurrent event analysis has been performed.
The cumulative incidence of CVC-associated bacteremia was 17.1 % (CI 13.9, 20.8). In multivariate analysis, a double lumen CVC and the surgical modality of CVC insertion were the factors significantly associated with this complication, as follows: double lumen CVC: HR 3.1, CI 2.1–4.6, p < 0.0001; surgical modality of CVC insertion: HR 1.5, CI 1.0–2.2, p = 0.03). Due to the low number of recurrent events, only the first episode was considered for this analysis.
The cumulative incidence of exit-site/tunnel infection was 13.3 % (CI 10.6, 16.5). In multivariate analysis, the risk factors for this type of complication were a double lumen CVC (HR 2.1, CI 1.4–3.2, p = 0.0003) and a diagnosis of leukemia or lymphoma (HR 1.8, CI 1.1–2.8, p = 0.01).
The cumulative incidence of malfunction/occlusion was 36.0 % (CI. 31.9, 40.4). In multivariate analysis, the factor significantly associated with this complication was an age at positioning less than 6.1 years (HR 1.6, CI 1.2–2.0, p = 0.0003), the diagnosis of leukemia or lymphoma (HR 1.9, CI 1.4–2.4, p < 0.0001) and double lumen CVC (HR 1.33, CI 1.04–1.7, p = 0.023). A high number of recurrent malfunctions have been observed, but no significant associations were found among the variables analyzed.
Overall, premature removal was performed in 189 cases of 919 first CVCs, with a cumulative incidence of 29.2 % (CI 25.1, 33.8). The factors associated with this event were the surgical modality of CVC insertion (HR 1.4, CI 1.1–1.9, p = 0.0153) and an age at CVC positioning less than 6.1 years (HR 1.6, CI 1.2–2.1, p = 0.0025). Table 5 summarizes the results of the analysis of risk factors.
Discussion
The CVC is an essential tool to safely administer intravenous therapy in hematology and oncology patients who undergo chemotherapy or hematopoietic stem cell transplantation. However, CVC life can be affected by complications that may require its premature removal, or necessitate hospitalization, increasing health costs for patient treatment and/or presenting a life-threatening risk. Several authors have demonstrated that CVC-related morbidity can be reduced, especially that due to infectious complications, by adopting best-practice procedures and checking their implementation over time among the team members involved in the CVC maintenance [7, 10, 19]. Since 2000 our center established a protocol for insertion, maintenance care, diagnosis and treatment of CVC complications by a multidisciplinary working group. Most of the current set of rules recommended to prevent infection were part of the adopted protocol of CVC handling and care [10, 20]. The main difference was the absence from our procedures of chlorhexidine solution for skin antisepsis and the use of 10 % povidone-iodine solution. This is explained by the fact that at the beginning of the study, the superiority of chlorhexidine solution over 10 % povidone-iodine solution was not yet clear and, importantly in the following years, the delayed adoption of chlorhexidine solution in our hospital. In fact, povidone-iodine solution has been associated with difficulty or delay in visually determining the signs of local inflammation and with inactivation by a protein-rich exudate. A meta-analysis on eight randomized studies involving 4143 central lines showed that chlorhexidine gluconate reduced the risk for CVC-associated bacteremia over povidone-iodine by 49 % [21], but most of the evidence derived from studies with short- or medium-term or peripheral CVCs while this superiority with tunneled long-term CVCs is not yet clear. In a recent prospective study, Yamamoto et al. found that that in adult patients with long-term CVCs, the use of 1 % chlorhexidine-gluconate ethanol versus 10 % povidone-iodine for skin antisepsis of the CVC exit-site was associated with CVC-associated blood stream infections of 0.75 vs. 3.62 per 1000 CVC-days, respectively [22]. Interestingly, the use of povidone-iodine solution in our study was associated with a bacteremia rate of 0.4/1000 CVC-days that is even lower than that reported with chlorhexidine gluconate solution in the Yamamoto study. A recent randomized study performed in French intensive care units showed that skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol significantly reduced the rate of intravascular catheter-related infection but this effect was not evident for CVCs [23].
Although infections are usually believed to be the principal cause of CVC morbidity, mechanical complications and malfunctioning were in fact the most frequent complications accounting for 1.7 complications/1000 CVC-days. Overall, CVC malfunctioning did not have severe consequences for the patient because the protocol adopted to restore the patency of the CVC, based on urokinase administration, was successful in most cases and CVC removal was needed in only 2.3 % of episodes. Despite the limited prospective data available, the use of urokinase to restore the patency of a CVC is considered the most effective treatment together with alteplase with the advantage of a lower cost [24]. The risk factors for malfunction/occlusion complications, i.e., age range <6 years, diagnosis of leukemia/lymphoma, double lumen CVC, are consistent with the fact that all three situations require a high number of CVC accesses per day and/or expose the patient to procoagualant drugs, such as prednison, dexamethasone or L-aspaginase, which can favor the formation of fibrin inside the CVC or fibrin cap on the tip of the CVC [4, 5, 9]. Considering the very low rate of CVC-related thrombosis, i.e., 0.86 % of CVCs and 0.024 episodes/1000 CVC-days, and the fact that malfunction and occlusion can be managed with urokinase treatment, our findings agree with the current recommendation that anticoagulation with low molecular weight heparin or vitamin K antagonists is not needed for prophylaxis of CVC-related thrombosis and occlusions [25]. However, mechanical complications were rarely repairable, comprising 77.4 % of episodes of premature loss of the CVC. An age younger than 6 years was the only risk factor for this complication because in the infant, or in young babies, it is difficult to prevent sudden traction of the CVC or to monitor movements or positions that could pull out the CVC. According to these findings, the age range group of 0–6 years could benefit from the adoption of a sutured secure device provided that it is tolerated by the patient [13]. However, we highlight that the evidence of efficacy of this type of device (prolongation of dwell time, reduction of dislodgments, and reduction of infections) is limited to non-tunneled peripheral CVCs [26].
Systemic and exit-site/tunnel infections represented the third- and the fourth-ranked causes of CVC complications and the second- and third-ranked causes of CVC premature removal, respectively. Indeed, in this study, one out of five CVCs and one out of ten CVCs with bacteremia or exit-site/tunnel infection were removed, respectively. In particular, CVC-associated bacteremia may be life-threatening for the patient, and it is always associated with a cost increase for the health system and with a prolongation of the length of patient hospital stay [27]. Although still debated among experts, our internal policy to draw blood cultures both from CVC and peripheral vein at the onset of fever is supported by the demonstration that up to 12 % of true bloodstream infections may have the germ isolated only from peripheral vein [28]. Moreover, the use of a double set of blood cultures makes it possible to define a CVC-associated bacteremia without removing the CVC by recording, if available, the different times of positivization of cultures. Several strategies have been experimented with over the years to keep the incidence of CVC BSI as low as possible, ranging from the use of antibiotic/antibacteric-coated CVCs to flushing or locking the CVC with urokinase or antibiotic solutions [29, 30]. Despite these interventions resulting in a reduction of the incidence of CVC-related infections compared to controls, we and other pediatric groups reported an incidence rate of CVC-related infections comparable to that reported in the experimental arms simply by establishing a precise best-practice set of rules to prevent CVC infection from the daily handling for blood sampling or therapy administration [4, 5, 9]. The incidence of 0.4/1000 CVC-days for CVC-associated bacteremia found in this study is even better than that reported recently in a pediatric prospective study in which CVC-related blood stream infections decreased from 2.29 to 0.56/1000 CVC-days within 2 years through the implementation of a set of measures including the use of chlorexidine gluconate [10]. Our better results may depend on the fact that we report the complications as events per 1000 utilization days whereas other authors report the events per 1000 inpatient days [10, 31]. In multivariate analysis, surgical insertion by cutdown technique and dual lumen CVC were the risk factors for CVC-associated bacteremia. In our experience, both characteristics were typical of patients at higher risk of infectious complications because a dual lumen CVC was used in patients eligible for high dose chemotherapy or stem cell transplant whereas surgical positioning of CVC was reserved for patients at major risk of bleeding because of the status of the underlying disease.
In this study, we paid special attention to the management of the minor infectious complications, such as the exit-site/tunnel infections, by establishing “a priori” a protocol of intervention based on a visual score of severity. This type of complication is usually under-investigated, compared with CVC-associated bacteremia, despite the fact that it can result, though more rarely, in the loss of the CVC. We found an overall incidence of 0.3 episodes of exit-site/tunnel infection/1000 CVC-days that compared favorably with the figure of 2.59 episodes/1000 CVC-days reported by other authors in the past [31]. Notably, this complication was recently reported as high as 3.74 episodes/1000 CVC-days in pediatric patients with a tunneled CVC for chronic hemodialysis, when routine skin medication was performed with iodine-povidone [32]. The factors predicting a high risk of occurrence of this type of infectious complication were an underlying diagnosis of leukemia/lymphoma and the need for a dual lumen CVC. Both factors are usually present in patients who develop a prolonged, severe leukopenia and a high grade of immunosuppression due to chemotherapy.
The risk factors for premature removal of CVC, i.e., younger age and the surgical technique of insertion, reflect the most important complications for the survival of CVCs, which are the mechanical complication and CVC-related bacteremia. This suggests that a better fixation of the CVC could increase the probability of a longer CVC-life at least in younger patients, while the poorer outcome of CVCs inserted by the cutdown technique reflects the worst underlying clinical conditions and the higher bleeding risk of this group of patients.
In conclusion, we found that using a best-practice set of rules for a decade resulted in us keeping low the number of complications that may affect the CVC or the patient’s life without introducing into the practice flushing with antibiotics or using an antibiotic-coated CVC. Future prospective studies are needed to assess whether the benefit found in non-tunneled CVCs in using skin antisepsis with chlorexidine solutions or sutured secure device is applicable also to long-term tunneled CVCs.
References
Iannacci L, Piomelli S (1984) Supportive care for children with cancer. Guidelines of the children’s cancer study group. Use of venous access lines. Am J Pediatr Hematol Oncol 6:277–281
Albanese CT, Wiener ES (1993) Venous access in pediatric oncology patients. Semin Surg Oncol 9:467–477
Taber SW, Bergamini TM (1997) Long-term venous access: indications and choice of site and catheter. Semin Vasc Surg 10:130–134
Pinon M, Bezzio S, Tovo PA et al (2009) A prospective 7-year survey on central venous catheter-related complications at a single pediatric hospital. Eur J Pediatr 168:1505–1512
Fratino G, Molinari AC, Parodi S et al (2005) Central venous catheter-related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol 16:648–654
Cesaro S, Corrò R, Pelosin A et al (2004) A prospective survey on incidence and outcome of broviac/Hickman catheter-related complications in pediatric patients affected by hematological and oncological diseases. Ann Hematol 83:183–188
Schiffer CA, Mangu PB, Wade JC et al (2013) Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 31:1357–1370
Carraro F, Cicalese MP, Cesaro S et al (2013) Guidelines for the use of long-term central venous catheter in children with hemato-oncological disorders. On behalf of supportive therapy working group of Italian association of pediatric hematology and oncology (AIEOP). Ann Hematol 92:1405–1412
Cesaro S, Tridello G, Cavaliere M et al (2009) Prospective, randomized trial of two different modalities of flushing central venous catheters in pediatric patients with cancer. J Clin Oncol 27:2059–2065
Rinke ML, Chen AR, Bundy DG et al (2012) Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatrics 130:996–1004
Cesca E, Dall’igna P, Boscolo-Berto R et al (2014) Impact of severe neutropenia and other risk factors on early removal of implanted central venous catheter (ICVC) in children with hematologic malignancies. J Pediatr Hematol Oncol 36:541–544
Sri Paran T, Corbally M, Fitzgerald RI (2003) New technique for fixation of broviac catheters. J Pediatr Surg 38:51–52
Crocoli A, Tornesello A, Pittiruti M et al (2015) Central venous access devices in pediatric malignancies: a position paper of Italian association of pediatric hematology and oncology. J Vasc Access 16:130–136
Molinari AC, Haupt R, Saracco P, Di Marco M, Castagnola E, Fratino G (2004) Urokinase for restoring patency of malfunctioning or blocked central venous catheters in children with hemato-oncological diseases. Support Care Cancer 12:840–843
Kellerman S, Chan J, Jarvis W (1998) Use of urokinase in pediatric hematology/oncology patients. Am J Infect Control 26:502–506
Kerner JA Jr, Garcia-Careaga MG, Fisher AA, Poole RL (2006) Treatment of catheter occlusion in pediatric patients. JPEN J Parenter Enteral Nutr 30(Suppl 1):73–81
Baskin JL, Pui CH, Reiss U et al (2009) Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. Lancet 374:159–169
Kelly PJ, Lim LL (2000) Survival analysis for recurrent event data: an application to childhood infectious diseases. Stat Med 19:13–33
Wheeler DS, Giaccone MJ, Hutchinson N et al (2011) A hospital-wide quality-improvement collaborative to reduce catheter-associated bloodstream infections. Pediatrics 128:995–1004
O’Grady NP, Alexander M, Burns LA et al (2011) Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 52:162–193
Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S (2002) Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med 136:792–801
Yamamoto N, Kimura H, Misao H et al (2014) Efficacy of 1.0% chlorhexidine-gluconate ethanol compared with 10% povidone-iodine for long-term central venous catheter care in hematology departments: a prospective study. Am J Infect Control 42:574–576
Mimoz O, Lucet JC, Kerforne T et al (2015) Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 386:2069–2077
van Miert C, Hill R, Jones L (2012) Interventions for restoring patency of occluded central venous catheter lumens. Cochrane Database Syst Rev 4:CD007119
Debourdeau P, Farge D, Beckers M et al (2013) International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost 11:71–80
Frey AM, Schears GJ (2006) Why are we stuck on tape and suture? A review of catheter securement devices. J Infus Nurs 29:34–38
Leistner R, Hirsemann E, Bloch A, Gastmeier P, Geffers C (2014) Costs and prolonged length of stay of central venous catheter-associated bloodstream infections (CVC BSI): a matched prospective cohort study. Infection 42:31–36
Scheinemann K, Ethier MC, Dupuis LL, Richardson SE, Doyle J, Allen U, Sung L (2010) Utility of peripheral blood cultures in bacteremic pediatric cancer patients with a central line. Support Care Cancer 18:913–919
Huang EY, Chen C, Abdullah F et al (2011) Strategies for the prevention of central venous catheter infections: an american pediatric surgical association outcomes and clinical trials committee systematic review. J Pediatr Surg 46:2000–2011
van de Wetering MD, van Woensel JB, Lawrie TA (2013) Prophylactic antibiotics for preventing gram positive infections associated with long-term central venous catheters in oncology patients. Cochrane Database Syst Rev 11, CD003295
Elishoov H, Or R, Strauss N, Engelhard D (1998) Nosocomial colonization, septicemia, and Hickman/broviac catheter-related infections in bone marrow transplant recipients. A 5-year prospective study. Medicine (Baltimore) 77:83–101
Paglialonga F, Consolo S, Biasuzzi A et al (2014) Reduction in catheter-related infections after switching from ovidone-iodine to chlorhexidine for the exit-site care of tunneled central venous catheters in children on hemodialysis. Hemodial Int 18(Suppl 1):13–18
Acknowledgments
We thank Mr. Rodney Seddom for the revision of the English style of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cesaro, S., Cavaliere, M., Pegoraro, A. et al. A comprehensive approach to the prevention of central venous catheter complications: results of 10-year prospective surveillance in pediatric hematology-oncology patients. Ann Hematol 95, 817–825 (2016). https://doi.org/10.1007/s00277-016-2634-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-016-2634-x