Abstract
Goals of work
To evaluate differences in success rate between two dosages of intraluminal urokinase (IL-UK) for treatment of withdraw occlusion in central venous catheters (CVC) and to confirm the efficacy of a salvage protocol with low-dose systemic urokinase (S-UK) in case of failure of IL-UK or of complete catheter obstruction.
Patients and methods
All malfunctioning or occluded partially implanted indwelling catheters inserted in a 29-month period in children with cancer at two tertiary care centers (Genoa and Turin) in Italy were eligible for this study. In cases of withdraw occlusion, IL-UK was used as first-line treatment with different schedules of administration in the two centers: a 5,000 IU/ml dose was used in Genoa and a 25,000 IU/ml dose in Turin (Protocol A). In case of failure of the front-line protocol or in case of complete CVC occlusion, S-UK at 1,000 IU/kg per hour for 3 h was used as a salvage protocol in both centers (Protocol B).
Main results
There were 81 episodes of malfunction and three of occlusion recorded in 68 CVCs. Protocol A was successful in 75 (92.5%) of the malfunction episodes. In particular, the dose of 5,000 IU of IL-UK was successful in 42 (89%) CVCs while the 25,000 IU dose resolved 33 (97%) of the episodes (not significant). The six patients with CVC refractory to IL-UK and the three subjects with complete CVC occlusion were treated with S-UK. Patency was obtained in seven cases (78%); the remaining two catheters had to be removed.
Conclusions
We found that 5,000 IU of IL-UK were as effective as 25,000 IU to resolve withdrawal occlusion in partially implanted CVCs and that systemic treatment with urokinase may rescue a significant proportion of CVCs refractory to IL-UK or that are apparently completely occluded.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Indwelling central venous catheters (CVCs) have been used over the last two decades in pediatric oncology and are now considered essential devices for appropriate management of children with cancer [1]. Although few reports are available regarding CVC-related complications in children, the inability to withdraw blood or the complete obstruction of the catheter are the most frequent complications, occurring according to different reports in 20–40% of implanted CVCs [2, 3]. In these cases, postural changes with or without heparin flushes are usually used to resolve the complication, but when these procedures fail, urokinase (UK) is often used with different schedules reported in the literature [4, 5]. Administration of intraluminal UK (IL-UK) usually restores CVC patency, but it is not clear if low doses are as effective as high doses. Generally, IL-UK has been reported to fail in about 5–6% of all implanted CVCs, resulting in catheter removal [2, 6]. Thus, new strategies are needed in order to reduce the number of children who have to undergo another surgical procedure to implant a new CVC.
We here report on a study to determine differences, if any, in success rates between two dosages of IL-UK (5,000 IU versus 25,000 IU) for treatment of malfunctioning or occluded catheters and to evaluate the feasibility and efficacy of a salvage protocol with low-dose systemic UK (S-UK: 1,000 IU/kg per hour for 3 h) for the rescue of completely occluded or IL-UK-refractory CVCs.
Design and methods
As part of a comprehensive prospective follow-up study on CVC-related complications in children with hematological or oncological diseases, all CVCs inserted between January 2000 and May 2002 at the G. Gaslini, Genoa and Regina Margherita, Turin, children’s hospitals for the management of hematological or oncological diseases were prospectively evaluated to determine the incidence of any complication. In this paper, we report on the experience pertaining to incidence and treatment of malfunction complications.
During the study period, most of the cancer patients had partially implanted, tunneled, silicone rubber, right-atrial CVCs inserted. Catheters where either of the Hickman-Broviac (HB) type or of the pressure-activated valve (PASV) type. Catheter size was usually 6 or 9 fr. according to the patient’s age. Totally implantable catheters (ports) were used only in selected cases and are thus excluded from this study. In both centers, CVC insertion was always performed surgically under general anesthesia via external or internal jugular vein cut down. During placement, the correct position of the distal tip of the catheter (at the superior vena cava–right atrium junction) was checked by fluoroscopy, and a standard chest radiograph with the patient in the upright position was obtained immediately afterward. As for maintenance procedures in both centers, HB catheters, when not in use, were flushed three times a week with a heparinized solution while PASVs were flushed with normal saline solution once a week.
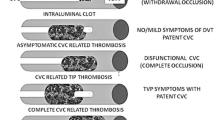
For purposes of this study, a malfunction event was defined as the difficulty to withdraw blood through the catheter not solved by postural changes or flushes with saline or heparinized solution (50 IU/ml). Occlusion was defined as the inability to withdraw blood and infuse fluids. In case of a malfunctioning CVC, IL-UK was used as first-line treatment (Protocol A, Table 1). The schedule of administration of UK was different in the two centers, with a 5,000 IU/ml dose used in Genoa and a 25,000 IU/ml dose in Turin. In both centers, the vial (either the 5,000 IU or the 25,000 IU) was reconstructed with 1 ml of normal saline, and the CVC was then filled with 0.3–0.5 ml of this solution based upon the internal volume of the device. The solution was then left in place for 30 s, and afterward, the patency of the device was checked.
In case of Protocol A failure or in case of CVC occlusion, children were clinically evaluated and a chest X-ray performed to locate the CVC’s tip. If CVC was correctly positioned, a Doppler ultrasound (US) and/or 2D echocardiography were performed to look for deep vein thrombosis (DVT) or thrombi at or near the device tip [7]. Subjects with documented DVT or right atrial thrombus were excluded from this study and treated with other institutional protocols. Subjects refractory to intraluminal UK with undetectable thrombotic complication and with platelets count >50×109/L were then treated according to a salvage protocol (Protocol B, Table 1) with S-UK at a dosage of 1,000 IU/kg per hour for 3 h (via peripheral vein in case of CVC occlusion). The drug was usually diluted in 100 ml of saline. Parental informed consent was requested and obtained before application of either protocol. Finally, to evaluate whether 25,000 IU of IL-UK may be more effective than 5,000 IU in preventing further catheter occlusion, malfunction episodes occurring within 20 days from IL-UK administration in the same CVC were identified.
The χ2 test or the Fisher exact test was used to compare differences in the percentages of success between the different treatment modalities. Statistical tests were two-tailed, and tests were considered significant when p<0.05.
Results
During the study period, 418 catheters were consecutively inserted in 368 children (212 M, 156 F) with hematological or oncological diseases and a median age of 6.2 (range 0.1–17.9). years The median follow-up after CVC insertion was 258 days (range 3–868) for a total of 107,012 catheter days. During follow-up, a total of 81 episodes of malfunction (47 in Genoa, 34 in Turin) and three of occlusion were recorded in 68 CVCs (16% of all CVCs) for a total of 84 episodes and an overall incidence of 0.78 malfunction or occlusion events per 1,000 catheter days.
Protocol A was successful in 75 (92.5%) of the 81 malfunction episodes. In particular, the dose of 5,000 IU of IL-UK (Genoa) was successful in 42 (89%) CVCs while the 25,000 IU dose (Turin) resolved 33 (97%) of the malfunction episodes. The difference in success rate between the two schedules was not significant (p=0.393).
The six patients with CVC refractory to IL-UK (five to the 5,000 IU and one to the 25,000 IU dose) and the three subjects with complete CVC occlusion and negative imaging were treated with systemic low-dose UK according to Protocol B (Table 1). Patency was obtained in seven cases (78%) and, in particular, in four malfunctioning CVCs (67%) and in three (100%) occluded CVCs (not significant). The remaining two catheters had to be removed (one in the 5,000 IU group and the second in the 25,000 IU group) due to persistent withdrawal occlusion. No episode of bleeding was reported.
Finally, a second malfunction episode within 20 days from the first one occurred in five of the 42 events successfully treated with 5,000 IU (12%) and in three of the 33 (9%) successfully treated with 25,000 IU (not significant; p=0.22).
Discussion
We have demonstrated that 5,000 IU of IL-UK are as effective as 25,000 IU to resolve withdrawal occlusion in partially implanted CVCs and that systemic treatment with urokinase may rescue a significant proportion of CVC refractory to IL-UK or that are apparently completely occluded. These results confirm that a subclinical thrombotic complication is the most frequent etiological factor in CVC occlusion occurring in children with cancer or other hematological diseases. This is probably secondary to the frequent administration of blood products in these subjects. In patients with other types of diseases, the etiology might be different.
In general, the schedule of administration of thrombolytic agents for restoration of flow in malfunctioning catheters in children with cancer is empiric, and thrombolytic regimens differ with regard to the type of drug used, its dosage, and its duration [8]. When UK is used, both 5,000 and 25,000 IU of IL-UK are usually employed for restoring patency of malfunctioning or occluded CVCs [2, 5], and the reported success rate varies between 77 and 98%. In Italy, the cost of the 5,000 IU vial is of about €7.0 while that of the 25,000 IU vial is €26.0. Our success rate of 89% with 5,000 IU schedule, which is not significantly different from the 93% observed with the 25,000 IU schedule, further enhances the recommendation of the use of the lowest dose because of its economic advantage and comparable efficacy.
However, it might be argued that a higher dose of IL-UK might be more effective in the complete resolution of the fibrin deposit on the CVC surface thus preventing possible further malfunctioning. Our data did not demonstrate any difference between the two IL-UK schedules we considered in preventing malfunctioning complications within 20 days after IL-UK administration. We do not know if even lower doses can be effective; as far as this problem is concerned, the unavailability of vials with less than 5,000 IU of UK perhaps is the reason why treatment of withdrawal occlusion with lower doses has never been reported.
Our experience shows that the 1,000 IU/kg per hour of S-UK for 3 h is an effective rescue protocol for completely occluded CVCs since only two out of the nine CVCs (22%) for which this protocol was indicated had to be removed because of irresolvable complications. This observation confirms our previous results of five cases of CVCs that restored patency thanks to this low-dose UK schedule after failure with 25,000 IU of IL-UK [7].
Two other reports previously described a similar schedule to restore the functioning of blocked catheters in children. In the first [2], the authors used 5,000 IU of UK intraluminally and 200 IU/kg per hour as a systemic schedule. They did not report the results regarding the efficacy of the treatment in detail, but they did describe an overall 75% success rate of UK in treating malfunctioning or occluded CVCs. In the second [9], the treatment was effective in 11/12 CVCs. However, the authors of both papers used a lower dose of UK (200 IU/kg per hour) infused over a longer period (24 h). Those protocols consequently obliged the patients to be hospitalized for at least 24 h whereas our strategy, which did not generate any bleeding, allowed patients to be discharge on the same day (when admission was only due to CVC blockage), offering evident advantages in terms of cost and patient comfort.
References
Massicotte MP, Dix D, Monagle P, Adams M, Andrew M (1998) Central venous catheter-related thrombosis in children: analysis of the Canadian Registry of Venous Thromboembolic Complications. J Pediatr 133(6):770–776
Biagi E, Arrigo C, Dell’Orto MG, Balduzzi A, Pezzini C, Rovelli A et al (1997) Mechanical and infective central venous catheter–related complications: a prospective non-randomised study using Hickman and Groshong catheters in children with hematological malignancies. Support Care Cancer 5(3):228–233
Fratino G, Molinari AC, Mazzola C, Giacchino M, Saracco P, Bertocchi E et al (2002) A prospective study on indwelling central venous catheter related complications in children with broviac or clampless valved catheter. J Pediatr Hematol Oncol 24(8):657–661
Winthop AL, Wesson DE (1984) Urokinase in the treatment of occluded central venous catheters in children. J Pediatr Surg 19(5):536–538
Kellerman S, Chan J, Jarvis W (1998) Use of urokinase in paediatric haematology/oncology patients. Am J Infect Control 26(5):502–506
Ertem M, Yavuz G, Aysev D, Unal E, Gozdasoglu S, Tacyildiz N et al (1999) Right atrial catheter-related complications in pediatric oncology patients: the situation in a developing country. Pediatr Hematol Oncol 16(4):299–309
Molinari AC, Castagnola E, Mazzola C, Piacentino M, Fratino G (2001) Thromboembolic complications related to indwelling central venous catheters in children with oncological/hematological diseases: a retrospective study of 362 catheters. Support Care Cancer 9(7):539–544
Haire WD (2001) Techniques in dosing for thrombolysis of occluded central venous catheters. Tech Vasc Interv Radiol4(2):127–130
Bagnall HA, Gomperts E, Atkinson JB (1989) Continuous infusion of low-dose urokinase in the treatment of central venous catheter thrombosis in infants and children. Pediatrics 83(6):963–966
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Molinari, A.C., Haupt, R., Saracco, P. et al. Urokinase for restoring patency of malfunctioning or blocked central venous catheters in children with hemato-oncological diseases. Support Care Cancer 12, 840–843 (2004). https://doi.org/10.1007/s00520-004-0616-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0616-3