Abstract
Primary poor graft function (PGF) is a severe complication after allogeneic stem cell transplantation (SCT). The incidence, risk factors, and outcomes of PGF have not been well described, especially in the haploidentical SCT setting. We retrospectively reviewed patients who received haploidentical SCT at Peking University Institute of Hematology between January 1, 2011, and December 31, 2012. PGF was defined as persistent neutropenia (≤0.5 × 109 L−1), thrombocytopenia (platelets ≤20 × 109 L−1), and/or hemoglobin ≤70 g L−1 after engraftment with hypocellular bone marrow and full donor chimerism, without concurrent graft-versus-host disease or disease relapse. Incidence was calculated from all patients. Of the 464 total patients, 26 (5.6 %) developed primary PGF. The risk factors were analyzed and compared with control patients with good graft function who were selected using the case-pair method. Finally, 104 patients were selected as a control group according to the matching conditions: (1) the type (acute leukemia, myelodysplastic syndrome (MDS), chronic myelogenous leukemia (CML)) and status (standard risk, high risk) of underlying disease, (2) sex, (3) year in which the transplantation was received, and (4) a 1:4 ratio of case-control. No factors were found to be associated with primary PGF. Compared to cases with good graft function, patients with primary PGF experienced poor overall survival (34.6 vs. 82.7 %, p < 0.001). Of the 26 primary PGF patients, only nine achieved hematopoietic recovery and survived. In conclusion, primary PGF is a rare but life-threatening complication after haploidentical SCT, and effective therapies need to be explored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematopoietic reconstitution has been a cornerstone of successful allogeneic stem cell transplantation (allo-SCT). Recovery of hematopoiesis included the following: (1) rapid and persistent recovery of trilineage cell counts in peripheral blood and (2) the hematopoiesis originating from donor stem cells. Primary graft failure is a severe complication in which reconstitution of initial hematopoiesis after allo-SCT fails [1]. Its criteria are predominantly operational and based on peripheral blood cell counts. One of the known causes of primary graft failure is graft rejection. Graft rejection is the immune-mediated rejection of the donor allograft by residual host effector cells that occurs because of the genetic disparity between the recipient and the donor. However, another type of primary graft failure involves failure to achieve adequate blood counts following allo-SCT despite the presence of complete donor hematopoietic cell chimerism [2]; this group of patients is defined as poor graft function (PGF). Rejection is related to the recipient’s residual immune system, and a second transplantation is the only salvage treatment; however, the mechanism and characteristics of PGF remain unknown.
PGF can be divided into two groups, primary and secondary PGF. The former did not achieve initial reconstitution, while the latter specifies the loss of initial reconstitution. Patients with primary PGF have significantly poorer prognosis. In PGF patients treated with a boost of CD 34+ selected peripheral blood cells, the rate of trilineage recovery was 69 % in secondary PGF compared to 36 % in patients with primary PGF [3]. We had similar results in a previous study [4, 2], in which the recovery rates in primary and secondary PGF were 25 and 66.7 %, respectively; however, we used a different treatment, unselected peripheral blood cells. This suggests that primary PGF and secondary PGF may be different entities with different underlying pathogeneses; therefore, these two kinds of PGF should be investigated separately.
In the present study, we focused specifically on primary PGF since it indicates a clinically critical situation. A few prior studies have described the characteristics of PGF [5, 6, 3]; however, none of these studies distinguished primary PGF from secondary PGF. In addition, studies about PGF are mainly in the human leukocyte antigen (HLA)-identical SCT setting. Until recently, there have been no data about PGF in haploidentical SCT. In fact, there are more and more haploidentical transplantations for patients without an HLA-matched sibling (MSD) and unrelated donor (URD) in current era [7, 8]. Peking University Institute of Hematology (PUIH) is one of the most important centers in this field; we have adopted a protocol of unmanipulated haploidentical SCT, and patients have achieved comparable outcomes to those of MSD and URD [9, 10]. Here, we report the incidence, risk factors, and outcomes of primary PGF after haploidentical SCT in a large cohort.
Methods
Patients
Incidence cohort
All consecutive patients who received haploidentical SCT at PUIH from January 1, 2011, to December 31, 2012, were retrospectively reviewed. Patients who were diagnosed with acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), myelodysplastic syndrome (MDS), and chronic myelogenous leukemia (CML), and patients who received the first time of allo-SCT were included in the incidence cohort.
Risk factor cohort
In the incidence cohort, patients were divided into five groups according to the status on day 28 after allo-SCT: (1) good graft function (GGF), defined as achievement of both neutrophil and platelet engraftment on day 28 and independent of transfusion; (2) PGF, defined as persistent neutropenia (≤0.5 × 109 L−1), thrombocytopenia (platelets ≤20 × 109 L−1), and/or hemoglobin ≤70 g L−1 for at least three consecutive days by day 28 post-transplantation, transfusion-dependence, associated with hypoplastic-aplastic bone marrow (BM), and complete donor chimerism without concurrent graft-versus-host disease (GVHD) or disease relapse, primary PGF was defined as the failure to achieve initial engraftment by day 28 after transplantation and secondary PGF was defined as the fulfillment of the criteria after initial engraftment HSCT; (3) graft rejection, defined as never having achieved engraftment with mixed chimerism or complete recipient chimerism; (4) isolated cytopenia, defined as presence of one cytopenic count; or (5) early death before day 28. To analyze the risk factors, the control group was selected from the GGF patients using the case-pair method. Matching conditions included the following: (1) the type (acute leukemia, MDS, CML) and status (standard risk, high risk) of underlying disease, (2) sex, (3) year in which the transplantation was received, and (4) a 1:4 ratio of case-control. Finally, 104 patients were selected as a control group.
Transplantation regimen
Donor selection, HLA typing, and stem cell harvesting have been previously described [10, 9]. In brief, the conditioning therapy consisted of cytarabine (4 g m−2 day−1 on days −10 to −9), busulfan (3.2 mg kg−1 day−1 intravenously on days −8 to −6), cyclophosphamide (1.8 g m−2 day−1 on days −5 to −4), semustine (250 mg m−2 orally on day −3), and anti-thymocyte globulin (2.5 mg kg−1 day−1, rabbit [Sang Stat, Lyon, France] on days −5 to −2). Transplant recipients received cyclosporine A, mycophenolate mofetil, and short-term methotrexate for prevention of GVHD.
Definitions
Engraftment of neutrophils was defined as the first of three consecutive days when the absolute neutrophil count achieved 0.5 × 109 L−1 without granulocyte colony-stimulating factor stimulation (G-CSF). Engraftment of platelets was defined as the first of seven consecutive days when the platelet count was ≥20 × 109 L−1, independent from platelet substitution. Underlying disease was classified as high-risk or standard-risk. High-risk disease included acute leukemia either in non-remission or in the third or greater complete remission, and chronic myeloid leukemia in the blast phase; standard-risk disease included all other diagnoses. Hematological recovery was defined as neutrophils >0.5 × 109 L−1, platelets >20 × 109 L−1, and hemoglobin >70 g L−1 and without transfusion or G-CSF.
Statistical
All clinical data were analyzed retrospectively using SPSS package software (SPSS, Chicago, IL, USA). The incidence of PGF was calculated by the proportion of PGF in the total cohort. Univariate analysis in comparing crude incidence rates used χ 2 test or Fisher’s exact test. Risk factors with p < 0.2 in univariate analysis were chosen for further evaluation by multivariate logistic regression. Significant risk factors were added to the final model using a stepwise forward method with significance margins for entry of 0.10 and removal of 0.15.
Results
Incidence and characteristics of primary PGF
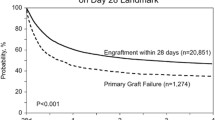
A total of 464 patients were enrolled in the incidence cohort, and of these, 26 (5.6 %) patients experienced primary PGF, 2 (0.4 %) with secondary PGF, 65 (14.0 %) with isolated thrombocytopenia, 2 (0.4 %) with early death, and 1 (0.2 %) with graft rejection. The basic characteristics of patients with primary PGF are listed in Table 1. In the 26 patients with primary PGF, 14 were male and 12 were female. The median age of patients and donors were 30 years (4–55) and 34.5 years (17–60), respectively. Twenty-one patients were diagnosed with acute leukemia, three with MDS, and two with CML. Of the 26 patients, 2 developed cytomegalovirus (CMV) viremia before day 28; none developed Epstein-Barr virus (EBV) or adenovirus.
The crude incidence of primary PGF was 5.6 %; the incidence was 4.1 % among those aged ≤35 and 10.0 % in those aged >35, respectively. In patients with AML, ALL, MDS, and CML, the incidence was 5.1, 5.8, 7.7, and 5.1 %, respectively. The incidences of primary PGF in patients with standard-risk and high-risk disease were 5.8 and 3.3 %, respectively.
Risk factors of PGF
The control group consisted of 104 patients with GGF and was used to identify the risk factors for PGF, which are shown in Table 2. Patients with donors of five matched loci had lower incidence of PGF (p = 0.026). Patients with older age, an older donor, and low CD4+ cells had p values <0.2 and were included in the multivariate model. However, none of these factors were found to be associated with the occurrence of primary PGF (Table 2).
Outcomes of primary PGF
In the 26 primary PGF, 9 recovered finally with a median time of 50 days (35–100) after transplantation. In the 26 patients, 14 received supportive therapy (G-CSF and transfusion) only and 7 recovered, 11 received second donor cell infusion and 2 recovered, 1 received second transplantation and did not recover. Finally, the nine patients with hematological recovery survived. All the patients without response died, only 1 death was attributed to relapse, the other 16 was attributed to infection-caused treatment-related mortality (TRM).
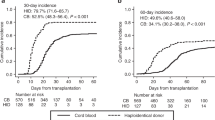
Regarding the long-term prognosis, patients with primary PGF have significantly poorer survival than patients with GGF (34.6 vs. 82.7 %, p < 0.001, Fig. 1). In the multivariate analysis, primary PGF was an independent factor associated with poor overall survival.
Discussion
PGF is an infrequent complication after allo-SCT that is not well understood, and little is known about the incidence and characteristics of PGF. Early reports found that the incidence of PGF ranged from 5 to 27 % [3, 11]; however, there were a number of flaws with these studies, including a lack of distinction between PGF and graft rejection, as well as a lack of separation between cases of primary and secondary PGF. It is important to distinguish between these two types of PGF because we now realize that primary and secondary PGF are distinct entities with significantly different prognoses [4] and the majority of cases are actually secondary PGF. Another limitation of previous studies was the heterogeneity of criteria used to define PGF [5, 3, 2]. We chose to define PGF in terms of its most insidious effects, infection, and hemorrhage attributed to severe neutropenia and thrombocytopenia [2]. The cutoff values that we selected for this study represent the minimal sufficient values that do not require blood or platelet transfusion and are associated with reduced risk of infectious complications.
A retrospective study by Xiao et al. [12] reported that the incidence of primary PGF was 12.1 %; this was significantly higher than that reported in our studies, possibly because the criteria of PGF in our study were stricter. In addition, most of the patients in the study by Xiao et al. were HLA-identical. Importantly, PGF may be more likely to occur in mismatched transplantation, and there are no data of PGF after haploidentical SCT. Our data provide the exact incidence of PGF after haploidentical transplantation for the first time since the wide adoption of this technique.
In previous reports, patient age, donor-recipient blood-type matching, and CMV infection were associated with PGF [12]. In our report, however, we did not find any of these associations. These differences may be due to the different patients group (both primary and secondary PGF), definition of PGF, types of transplantation, and so on. GVHD [13] and virus [14] are clearly associated with secondary PGF, and our previous study suggested that patients with secondary PGF have an impaired microenvironment [2]; however, this may not be applicable to primary PGF. In fact, these might be part of the different mechanisms through which primary and secondary PGF occur; primary PGF may be immune-related, while secondary PGF may be associated with impaired microenvironment due to GVHD and virus. We speculate that, to some extent, PGF after transplantation presents a similar situation to that of bone marrow failure. Immune-related impairment to the microenvironment and hematopoietic stem cells likely contribute to the pathogenesis of classical bone marrow failure syndrome (acquired aplastic anemia). The imbalance of T helper type 1 cells (Th1)/T helper type 2 cells (Th2), reduction of regulatory T cells, and activation of cytotoxic T lymphocytes (CTL) may involve in the pathogenesis [15, 16].
We notice that none of the patients with 1-locus mismatched donor developed PGF although the HLA disparity was not found to be associated with primary PGF in multivariate analysis. However, in previous studies, HLA-disparity has been shown to be related to increased incidence of PGF [3], though the underlying mechanism was not clear and this phenomenon remains to be confirmed in prospective studies. The increased incidence of PGF in mismatched transplantation suggests that there may be immune-related mechanism in primary PGF. DSA was associated with graft failure after allogeneic SCT [17, 18]. Our recent unpublished data demonstrated that there is strong association between DSA and primary PGF (41st EBMT annual meeting, 2015, Istanbul, oral presentation O043). DSA-positive patients experienced higher incidence of primary PGF (31 vs. 3.2 %, p = 0.000) than those of DSA-negative cases. However, these preliminary data needed to be confirmed, and the way how it associates with primary PGF needed to be explored in further study.
There are evidences demonstrating the correlation between natural killer cells with graft failure [19]. As one subgroup of primary PGF, NK cells may play role in its pathogenesis. However, we have to admit that we have no direct study of NK cells in patients of homogenous primary PGF. This is a question needed to answer in our further study.
Some recent reports [20, 21] suggest that patients with idiopathic myelofibrosis might have higher incidence of PGF than patients with other underlying disease. However, incidence and pathogenesis were not provided. In our study, no patient with idiopathic myelofibrosis received HSCT during this study period, so we do not have this data. This could be an interesting topic for further study. Our current study focuses on malignant hematological disease and suggests that primary PGF in malignant hematological disease is not very rare.
The prognosis of primary PGF is very poor, which can be easily understood. Most patients die of infection attributed to persistent leukocytopenia. Although some patients received a second infusion of donor cells or even second transplantation, the efficacy was very poor. Some recent studies have shown promising results from treating with a booster of CD34+ cells [20–22]; however, we should note that most patients who received the boosted cell infusion had secondary PGF, and we have already demonstrated that primary PGF has significantly worse prognosis than secondary PGF [4]. New therapeutic options are warranted to manage primary PGF on the basis of better understanding of primary PGF.
There were some limitations to our study. First, this was a retrospective study, and the event of primary PGF is still relatively rare. Second, no data regarding DSA or natural killer cell alloreactivity were available in the current study. Future prospective studies should be conducted to investigate the potential relationship between DSA or natural killer cells and primary PGF.
In conclusion, we demonstrated for the first time that primary PGF occurs in 5.6 % patients who received haploidentical transplantation, which was associated with poor survival. Our data suggest that further elucidation of the mechanisms underlying primary PGF is warranted so that effective therapies can be developed.
References
Locatelli F, Lucarelli B, Merli P (2014) Current and future approaches to treat graft failure after allogeneic hematopoietic stem cell transplantation. Expert Opin Pharmacother 15(1):23–36. doi:10.1517/14656566.2014.852537
Kong Y, Chang YJ, Wang YZ, Chen YH, Han W, Wang Y, Sun YQ, Yan CH, Wang FR, Liu YR, Xu LP, Liu DH, Huang XJ (2013) Association of an impaired bone marrow microenvironment with secondary poor graft function after allogeneic hematopoietic stem cell transplantation. Biology Blood Marrow Transplant J Am Soc Blood Marrow Transplant 19(10):1465–1473. doi:10.1016/j.bbmt.2013.07.014
Larocca A, Piaggio G, Podesta M, Pitto A, Bruno B, Di Grazia C, Gualandi F, Occhini D, Raiola AM, Dominietto A, Bregante S, Lamparelli T, Tedone E, Oneto R, Frassoni F, Van Lint MT, Pogliani E, Bacigalupo A (2006) Boost of CD34 + −selected peripheral blood cells without further conditioning in patients with poor graft function following allogeneic stem cell transplantation. Haematologica 91(7):935–940
Sun YQ, Liu DH, Xu LP, Zhang XH, Liu KY, Huang XJ (2013) The efficacy and safety of recombinant human granulocyte colony stimulating factor primed donor peripheral cell harvest in treatment of poor graft function after allogeneic stem cell transplantation. Zhonghua Nei Ke Za Zhi 52(9):730–733
Mohty M, Faucher C, Chabannon C, Vey N, Stoppa AM, Ladaique P, Novakovitch G, Olivero S, Bouabdallah R, Gastaut JA, Maraninchi D, Blaise D (2000) CD34(+) immunoselected cells for poor graft function following allogeneic BMT. Cytotherapy 2(5):367–370
Bittencourt H, Rocha V, Filion A, Ionescu I, Herr AL, Garnier F, Ades L, Esperou H, Devergie A, Ribaud P, Socie G, Gluckman E (2005) Granulocyte colony-stimulating factor for poor graft function after allogeneic stem cell transplantation: 3 days of G-CSF identifies long-term responders. Bone Marrow Transplant 36(5):431–435. doi:10.1038/sj.bmt.1705072
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P, Duarte RF, Dufour C, Falkenburg JH, Farge-Bancel D, Gennery A, Kroger N, Lanza F, Nagler A, Sureda A, Mohty M (2015) Hematopoietic SCT in Europe 2013: recent trends in the use of alternative donors showing more haploidentical donors but fewer cord blood transplants. Bone Marrow Transplant 50(4):476–482. doi:10.1038/bmt.2014.312
Piemontese S, Ciceri F, Labopin M, Bacigalupo A, Huang H, Santarone S, Gorin NC, Koc Y, Wu D, Beelen D, Tischer J, Ehninger G, Arcese W, Nagler A, Mohty M (2015) A survey on unmanipulated haploidentical hematopoietic stem cell transplantation in adults with acute leukemia. Leukemia 29(5):1069–1075. doi:10.1038/leu.2014.336
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, Chen H, Liu DH, Gao ZY, Chen YH, Xu LP, Zhang YC, Ren HY, Li D, Liu KY (2006) Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood 107(8):3065–3073. doi:10.1182/blood-2005-05-2146
Xiao-Jun H, Lan-Ping X, Kai-Yan L, Dai-Hong L, Yu W, Huan C, Yu-Hong C, Wei H, Jing-Zhi W, Yao C, Xiao-Hui Z, Hong-Xia S, Feng-Rong W, Fei-Fei T (2009) Partially matched related donor transplantation can achieve outcomes comparable with unrelated donor transplantation for patients with hematologic malignancies. Clin Cancer Res Off J Am Assoc Cancer Res 15(14):4777–4783. doi:10.1158/1078-0432.CCR-09-0691
Lee KH, Lee JH, Choi SJ, Lee JH, Kim S, Seol M, Lee YS, Kim WK, Lee JS (2004) Failure of trilineage blood cell reconstitution after initial neutrophil engraftment in patients undergoing allogeneic hematopoietic cell transplantation - frequency and outcomes. Bone Marrow Transplant 33(7):729–734. doi:10.1038/sj.bmt.1704428
Xiao Y, Song J, Jiang Z, Li Y, Gao Y, Xu W, Lu Z, Wang Y, Xiao H (2014) Risk-factor analysis of poor graft function after allogeneic hematopoietic stem cell transplantation. Int J Med Sci 11(6):652–657. doi:10.7150/ijms.6337
Peralvo J, Bacigalupo A, Pittaluga PA, Occhini D, Van Lint MT, Frassoni F, Nardelli E, Transino A, Pantarotto M, Marmout AM (1987) Poor graft function associated with graft-versus-host disease after allogeneic marrow transplantation. Bone Marrow Transplant 2(3):279–285
Lin Z, Kong Y, Wang Y, Zhang X, Liu D, Xu L, Huang X (2014) Analysis of risk factors for secondary cytopenia after allogeneic hematopoietic stem cell transplantation. Zhonghua Xue Ye Xue Za Zhi 35(1):4–8. doi:10.3760/cma.j.issn.0253-2727.2014.01.002
Solomou EE, Rezvani K, Mielke S, Malide D, Keyvanfar K, Visconte V, Kajigaya S, Barrett AJ, Young NS (2007) Deficient CD4+ CD25+ FOXP3+ T regulatory cells in acquired aplastic anemia. Blood 110(5):1603–1606. doi:10.1182/blood-2007-01-066258
Shi J, Ge M, Lu S, Li X, Shao Y, Huang J, Huang Z, Zhang J, Nie N, Zheng Y (2012) Intrinsic impairment of CD4(+)CD25(+) regulatory T cells in acquired aplastic anemia. Blood 120(8):1624–1632. doi:10.1182/blood-2011-11-390708
Yoshihara S, Maruya E, Taniguchi K, Kaida K, Kato R, Inoue T, Fujioka T, Tamaki H, Ikegame K, Okada M, Soma T, Hayashi K, Fujii N, Onuma T, Kusunoki Y, Saji H, Ogawa H (2012) Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical SCT. Bone Marrow Transplant 47(4):508–515. doi:10.1038/bmt.2011.131
Ciurea SO, Thall PF, Wang X, Wang SA, Hu Y, Cano P, Aung F, Rondon G, Molldrem JJ, Korbling M, Shpall EJ, de Lima M, Champlin RE, Fernandez-Vina M (2011) Donor-specific anti-HLA Abs and graft failure in matched unrelated donor hematopoietic stem cell transplantation. Blood 118(22):5957–5964. doi:10.1182/blood-2011-06-362111
Breuer S, Preuner S, Fritsch G, Daxberger H, Koenig M, Poetschger U, Lawitschka A, Peters C, Mann G, Lion T, Matthes-Martin S (2012) Early recipient chimerism testing in the T- and NK-cell lineages for risk assessment of graft rejection in pediatric patients undergoing allogeneic stem cell transplantation. Leukemia 26(3):509–519. doi:10.1038/leu.2011.244
Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, Pozzi S, Varaldo R, Lamparelli T, Bregante S, Van Lint MT, di Grazia C, Bacigalupo A (2014) CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 20(9):1440–1443. doi:10.1016/j.bbmt.2014.05.016
Askaa B, Fischer-Nielsen A, Vindelov L, Haastrup EK, Sengelov H (2014) Treatment of poor graft function after allogeneic hematopoietic cell transplantation with a booster of CD34-selected cells infused without conditioning. Bone Marrow Transplant 49(5):720–721. doi:10.1038/bmt.2014.5
Klyuchnikov E, El-Cheikh J, Sputtek A, Lioznov M, Calmels B, Furst S, Chabannon C, Crocchiolo R, Lemarie C, Faucher C, Bacher U, Alchalby H, Stubig T, Wolschke C, Ayuk F, Reckhaus ML, Blaise D, Kroger N (2014) CD34(+)-selected stem cell boost without further conditioning for poor graft function after allogeneic stem cell transplantation in patients with hematological malignancies. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 20(3):382–386. doi:10.1016/j.bbmt.2013.11.034
Acknowledgments
This work was supported (in part) by the National High Technology Research and Development Program of China (Program 863) (Grant No. 2013AA020401), The Key Program of National Natural Science Foundation of China (Grant No. 81230013), and the Scientific Research Foundation for Capital Medicine Development (Grant No. 2011-4022-08). We thank the editage (https://www.editage.com/) for the assistance in editing the manuscript.\
Conflict of interest
None.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yu-Qian Sun and Gan-Lin He contributed equally to this work.
Rights and permissions
About this article
Cite this article
Sun, YQ., He, GL., Chang, YJ. et al. The incidence, risk factors, and outcomes of primary poor graft function after unmanipulated haploidentical stem cell transplantation. Ann Hematol 94, 1699–1705 (2015). https://doi.org/10.1007/s00277-015-2440-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2440-x