Abstract
Purpose
The purpose of the study is to describe a case of ophthalmic artery (OA) arising from the presumed meningohypophyseal trunk (MHT) of the cavernous internal carotid artery (ICA).
Case report
A 63-year-old woman suspected of having cerebral infarctions underwent cranial magnetic resonance (MR) imaging and MR angiography. MR angiography showed a right OA that was found to arise from the superolateral aspect of the proximal cavernous ICA. This OA entered the orbit via the superior orbital fissure (SOF).
Discussion
Rarely, an OA arises from the inferior aspect of the middle cavernous ICA at the level of the inferolateral trunk (ILT) and enters the orbit via the SOF. This OA variation was traditionally regarded as a persistent primitive dorsal OA but is now believed to be due to the persistence of the lateral branch of the primitive maxillary artery. The present case had an OA arising from the superolateral aspect of the more proximal cavernous ICA than the origin of the ILT, which was suggested to be the origin of the MHT. Persistence of the proximal segment of the trigeminal artery may play an important role in the formation of this extremely rare variation.
Conclusion
To identify this extremely rare OA variation, careful observation of source images and the creation of volume-rendering MR angiography images are important.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ophthalmic artery (OA) is usually the first branch of the intradural internal carotid artery (ICA). The OA rarely arises from the cavernous ICA, with a reported magnetic resonance (MR) angiographic prevalence of 0.42% per OA [10]. The origin of this anomalous OA is usually located at the inferior aspect of the middle segment, suggestive of the inferolateral trunk (ILT).
We herein report a case of OA arising from the superolateral aspect of the proximal cavernous segment of the ICA, suggestive of the meningohypophyseal trunk (MHT). A similar case reported many years ago was diagnosed by catheter angiography [11].
Case report
A 63-year-old woman suspected of having cerebral infarctions underwent cranial MR imaging and MR angiography using a 3.0 Tesla scanner (Skyra; Siemens Healthineers, Erlangen, Germany). MR angiography findings were obtained using a standard three-dimensional time-of-flight technique. The imaging parameters were as follows: repetition time, 21.0 s; echo time, 3.7 s; flip angle, 18°; and slice thickness, 0.6 mm.
Cranial MR imaging revealed no abnormality except for non-specific small white-matter lesions (not shown). MR angiography showed a right OA arising from the superolateral aspect of the proximal cavernous segment of the ICA (Fig. 1). This finding was obvious on the volume-rendering (VR) images (Fig. 2). The source images of MR angiography revealed that the anomalous right OA passed through the superior orbital fissure (SOF), not the optic canal (OC) (Fig. 3).
Infero-superior projection of maximum-intensity-projection image of cranial magnetic resonance (MR) angiography shows an artery arising from the proximal cavernous segment of the internal carotid artery (ICA) (long arrow) and running toward the orbit (short arrow), suggestive of an ophthalmic artery (OA). There is no other artery supplying the right orbit
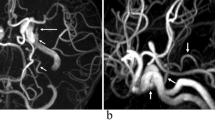
Infero-superior (a) and right lateral (b) projections of volume-rendering images of cranial MR angiography show an artery arising from the superolateral aspect of the proximal cavernous segment of the ICA (long arrows) and running toward the orbit (short arrows), suggestive of an OA. The normally originating left OA can be identified (dotted arrow), but the right OA is absent at the normal position
No further examinations (e.g. computed tomography [CT] angiography or catheter angiography) were performed. The patient was treated conservatively and showed a good clinical course.
Discussion
The OA usually arises from the anteromedial or superomedial aspect of the intradural ICA just distal to the dural ring. Rarely, it can arise from the superolateral aspect of the intradural ICA [3]. Based on microsurgical anatomic dissection findings, the prevalence of the cavernous origin of the OA was reported to range from 3.3% to 8% [1]. Because most of these cavernous origin OAs arise just proximal to the dural ring and enter the orbit via the optic canal [2], they may not be easily diagnosed by medical imaging as having a cavernous ICA origin [7]. In addition, due to the low spatial resolution of MR angiography, the reported prevalence of OA with cavernous ICA origin is only 0.42% per OA [10]. The cavernous ICA origin of an OA that enters the orbit via the SOF instead of the OC usually arises from the inferior aspect of the middle segment, suggestive of ILT. However, our patient had an OA arising from the superolateral aspect of the proximal segment, which was suggestive of MHT (Fig. 4). A similar case was reported previously based on catheter angiography findings [11].
A schematic illustration of the right carotid system in the right lateral projection. 1: normal OA arising from the supraclinoid ICA. 2: usually arising OA from the cavernous ICA. 3: OA of our patient arising from the proximal cavernous ICA. ICA internal carotid artery, OC optic canal, SOF superior orbital fissure
There are two different concepts concerning embryological development of the OA arising from the cavernous ICA: Padget’s and Lasjaunias’ concepts [2]. Arteries arising from the ILT and entering the orbit via the SOF were traditionally regarded as indicative of the persistence of the primitive dorsal OA. However, this variation is now believed to involve the persistence of the lateral branch of the primitive maxillary artery (PMA) [1]. The anomalous OA in our patient arose from the presumed MHT. At the origin of the persistent trigeminal artery (PTA), both the MHT and the artery of the inferior cavernous sinus arise [4]. Therefore, the MHT can be regarded as a remnant of the origin of the trigeminal artery, and the origin and extreme proximal segment of the anomalous OA in our patient might have been formed by the PTA, while the remaining distal segment might have been formed by the lateral branch of the PMA.
There are many types of OA origin variations in extra regions of the ICA. The most frequent type is middle meningeal artery (MMA) origin, which has a reported MR angiographic prevalence of 1.45% per OA [10]. Extremely rarely, OAs arise from the basilar artery [6], anterior cerebral artery [8] and middle cerebral artery (MCA) [2]. There are two types of double OAs: (1) both OAs arise from the ICA [9] and (2) one OA arises from the ICA and another from the MMA [10]. While the reason is unclear, there is a tendency toward right-side predominance in OA origin variations [10]. Indeed, our patient also had right-side OA variation.
Parlato et al. [5] reported a case of OA arising from the choroidal segment of the ICA; however, we believe that this patient had a duplicated MCA, and superimposition of this MCA and a normally originating OA was misdiagnosed as anomalous origin of the OA in the lateral projection of two-dimensional catheter angiography. To ensure the correct diagnosis of rare arterial variations, three-dimensional (3D) data acquisition, such as MR angiography, CT angiography, and 3D-rotational subtraction catheter angiography, are important and necessary. Using MR angiography, to identify a small artery running beside a large artery, VR images are superior to the maximum-intensity-projection images due to superimposition of two arteries (Fig. 1). Source images of MR angiography are crucial for identifying the entrance of the OA into the orbit (Fig. 2).
Conclusion
We reported a case of right OA arising from the superolateral aspect of the proximal cavernous ICA, presumed to lie at the level of the MHT, as diagnosed by MR angiography. VR images were useful for visualizing the proximal segment of this variation, and careful observation of the source images was important for the detection of the OA in the SOF.
Availability of data and materials
Not applicable.
References
Bertelli E, Regoli M, Bracco S (2017) An update on the variations of the orbital blood supply and hemodynamic. Surg Radiol Anat 39:485–496. https://doi.org/10.1007/s00276-016-1776-9
Bonasia S, Bojanowski M, Robert T (2020) Embryology and anatomical variations of the ophthalmic artery. Neuroradiology 62:139–152. https://doi.org/10.1007/s00234-019-02336-4
N’da HA, Peltier J, Zunon-Kipré Y, Alsaiari S, Foulon P, Legars D, Havet E, (2014) An unusual superolateral origin of ophthalmic artery: an anatomic case report. Surg Radiol Anat 36:95–97. https://doi.org/10.1007/s00276-013-1132-2
Ohshiro S, Inoue T, Hamada Y, Matsuno H (1993) Branches of the persistent primitive trigeminal artery–an autopsy case. Neurosurgery 32:144–148. https://doi.org/10.1227/00006123-199301000-00025
Parlato C, di Nuzzo G, Luongo M, Tortora F, Briganti F (2011) Anatomical variant of origin of ophthalmic artery: case report. Surg Radiol Anat 33:275–278. https://doi.org/10.1007/s00276-010-0745-y
Rivera R, Choi IS, Sordo JG, Giacaman P, Badilla L, Bravo E, Echeverria D (2015) Unusual origin of the left ophthalmic artery from the basilar trunk. Surg Radiol Anat 37:399–401. https://doi.org/10.1007/s00276-014-1327-1
Uchino A (2021) Intracavernous internal carotid artery-originating ophthalmic artery entering the orbit via the optic canal. Surg Radiol Anat 43:1967–1968. https://doi.org/10.1007/s00276-021-02835-1
Uchino A, Saito N, Ikeda S, Ishihara S (2015) Ophthalmic artery arising from the anterior cerebral artery diagnosed by MR angiography. Surg Radiol Anat 37:1009–1012. https://doi.org/10.1007/s00276-015-1441-8
Uchino A, Saito N, Kurita H, Ishihara S (2013) Double ophthalmic arteries arising from the internal carotid artery. Surg Radiol Anat 35:173–175. https://doi.org/10.1007/s00276-012-1005-0
Uchino A, Saito N, Takahashi M, Kozawa E, Mizukoshi W, Nakajima R, Okano N (2013) Persistent dorsal ophthalmic artery and ophthalmic artery arising from the middle meningeal artery diagnosed by MR angiography at 3 T. Surg Radiol Anat 35:775–782. https://doi.org/10.1007/s00276-013-1085-5
Willinsky R, Lasjaunias P, Berenstein A (1987) Intracavernous branches of the internal carotid artery (ICA). comprehensive review of their variations. Surg Radiol Anat 9:201–215. https://doi.org/10.1007/BF02109631
Acknowledgements
Not applicable.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
AU carried out the study design and drafted the manuscript. AU and SI reviewed the manuscript critically, and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
The patient signed informed consent regarding publishing his data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uchino, A., Ishihara, S. Ophthalmic artery arising from the presumed meningohypophyseal trunk of the cavernous internal carotid artery diagnosed by magnetic resonance angiography. Surg Radiol Anat 44, 1025–1028 (2022). https://doi.org/10.1007/s00276-022-02975-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-02975-y