Abstract
Purpose
The radius is described with a single tuberosity: the radial tuberosity. However, we hypothesize that there is a second tuberosity on the interosseous border of the radius: which we propose to call the interosseous tuberosity – Tuberositas interossea radii – (IT).
Methods
First, we analyzed all anteroposterior radiographs of the forearm (48 females, 54 males; 62 lefts and 40 rights) as well as CT scans (6 females, 7 males; 5 lefts and 8 rights) carried out during one year in our hospital. We evaluated the presence of IT, its length, thickness of the interosseous cortex at IT level, above and below compared with anterior, posterior and lateral bone cortices. In the second part of the study, we dissected cadaveric forearms to determine which ligaments and muscles were attaches on the IT.
Results
A total of 102 standard forearm radiographs and 13 CT-scans were analyzed. In all cases, an IT was present. The mean tuberosity length was 93.9 mm (+ / − 15.8), which corresponds to 37% (+ / − 5) of total radial length. IT corresponds to a significant thickening (7.6 mm than 4.2 mm and 4.3 mm below; p < 0.0001) of radial interosseous cortex. A total of 10 forearms were dissected. In all cases, we observed that IT served as an attachment for central band of interosseous membrane and for all extrinsic muscles of the thumb with the exception of the extensor pollicis longus.
Conclusion
Tuberositas interossea radii exists, corresponds to a cortex thickening and may play a role in the stability of the forearm and the function of the thumb.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The radius is classically described with a single tuberosity: the radial tuberosity for the biceps brachii tendon insertion. However, most of anatomical illustrations represent a smooth relief on interosseous border of the radius, approximately in the middle third. We commonly observe this relief in our daily clinical activity, especially on forearm X-rays.
In anatomical books and publications, interosseous border of the radius description is classically found, defined as the sharp margin located along the medial side of the radius shaft. It extends distally from the mediodistal edge of the radial tuberosity to the ulnar notch, thereby separating anterior and posterior radial surfaces. However, there is no mention of a tuberosity at this site.
We hypothesize that this relief corresponds to an authentic tuberosity, defined as a bone elevation or protuberance, in which a ligament or muscle is attached [9].
Our first purpose was to identify whether this relief really corresponds to a tuberosity. The secondary objective is to study its morphological characteristics and determine which structures are attached on it.
Materials and methods
This study was divided in two parts. The first one is a radiological part. It is to determine whether this relief fulfils tuberosity’s definition, but also to specify its morphological characteristics. The second part is cadaveric and aims to determine which structures were attached on this relief.
Radiological part
Our hospital’s database has been reviewed to collect all consecutive forearm X-rays taken between October 1, 2016 and September 31, 2017. These radiographs were found and analyzed using the image archiving and communication system (PACS, Carestream Vue Pacs, version 12.1, Carestream Healths, Rochester, New York, USA). Inclusion criteria were: age over 18 years and anteroposterior X-rays of the forearm in full supination. The exclusion criteria were the presence of at least one fracture or radio-ulnar dissociation, tumor, congenital malformation, former fracture, X-rays of the forearm not strictly in both the antero-posterior and full supination. All data collected were anonymized by a blinded study collaborator.
Three blind observers were involved to analyze radiographs. In order to achieve the main study objective, observers had to apply standardized methodology. First, they had to delimit ulnar boundary of endomedullary canal (ULEC). It corresponds to a bright radiographic line extending along the entire radial axis. Second, they had to delimit the radial interosseous border of the radius boundary (IB). Third, they had to determine if there was a radial diaphyseal segment on which an increasing distance between the ULEC and the IB exists, thus defining presence of an interosseous relief. If it was confirmed, observers had to mark two points labelled “SLIT” and “ILIT” corresponding respectively to the proximal and distal limits of this interosseous relief. Based on these two points, they had to collect following measurements using the PACS measurement tool: the length of the interosseous relief corresponding to the distance between SLIT and ILIT, the distance between proximal margin of the head of the radius (“RH”) and the tip of the styloid process of the radius (“TRSP”) corresponding to radius length (Fig. 1).
On the left: summary schema of anatomical methodological references for X-rays analysis. On the right: antero-posterior forearm X-rays in supination. Separation between ulnar boundary of endomedullary canal (ULEC) and radial interosseous boundary (IB) is clearly visible on the interosseous side of the radial shaft
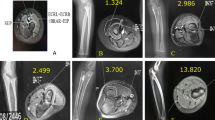
In order to improve morphometric characteristics determination of interosseous relief, additional data were obtained by CT scan. Forearm CT images were selected retrospectively from the PACS of our hospital from January 1, 2017 to June 30, 2017. Inclusion and exclusion criteria were similar as those mentioned for X-rays analysis. All scans were performed on a 64-slice CT scanner (SOMATOM Sensation 64 or Definition AS, Siemens, Erlangen, Germany). Interosseous relief presence was determined using the same methodology as described above. If it was present its upper and lower limits were also localized. Then, the radial morphology was analyzed on three groups of axial sections. Each group had three slices spaced 5 mm from each other: first group of slices between the radial tuberosity and SLIT, a second group at the level of the middle of the supposed tuberosity and a third group under ILIT point. On each slice, following parameters were measured: thickness (mm) of the anterior, posterior, medial and lateral bone cortex as well as the surface of the cancellous bone and the total surface of the radius. For each slice, the surface ratio (SR) between total radius surface and cancellous bone surface was calculated (Figs. 2, 3, 4).
Anatomical part
This part of the study was conducted in cadaveric anatomical laboratory. During their lifetime, all donors had given their informed consent to body donation for teaching and research purposes. The mean age of donors was 84 + / − 6.32 years old (76–95 years). Six donors (four left and two right forearms) were females and four donors (two left and two right forearms) were males.
Frozen bodies were thawed overnight and carefully evaluated according to following exclusion criteria: scars, deformity, dislocation of radio-ulnar joints, presence of an implanted device (osteosynthesis, arthroplasty). Fluoroscopy was also used to identify the interosseous relief. Then, soft tissues were dissected from the superficial layers to the deeper. A Henry’s approach was used to identify muscle attachments on the anterior surface along the interosseous border of the radius while a posterior approach was used to identify dorsal attachments. A map of muscle attachment was finally obtained for each subject. Finally, muscles were removed to keep the interosseous membrane (IOM) intact. Relationships between interosseous relief and the different parts of the IOM were recorded.
Statistical analysis
All the results are reported as mean and standard deviations. Comparisons were performed using a non-parametric analysis of variance (ANOVA) model. Post-hoc analysis (to detect individual differences) was only performed when the overall test was significant. A p value < 0.05 was considered statistically significant.
Results
In the radiographic part, we found 196 antero–posterior forearms radiographs. After applying exclusion criteria, 102 forearm radiographs were analyzed. Average age was 45.5 years (+ / − 20.7), with a sex ratio of 1.43 (62 left and 40 right sides). Interosseous tuberosity was observed in all patients (100%). The average radial length was 252.6 mm (+ / − 21.8). Mean IT length (SLIT-ILIT distance) was 93.9 mm (+ / − 15.8), which corresponds to 37% (+ / − 5) of total radial length.
A total of 13 CT forearms of the 19 CT scans selected, met the inclusion criteria (6 females, 7 males; 5 lefts and 8 rights). Average thickness of the interosseous cortex was significantly higher at the IT level (7.6 mm + / − 1.8) than above (4.2 mm + / − 0.9; p < 0.0001) and below (4.3 mm + / − 0.8; p < 0.0001). There was no significant difference of thickness between ventral, dorsal and lateral cortices above, at or below the IT (Fig. 5). At IT level, interosseous cortex thickness was higher compared with ventral (p < 0.0001), dorsal (p < 0.0001) and lateral (p < 0.0001) cortices. SR was higher at IT level (5.95 + / − 2.2) than above (3.48 + / − 1.1; p < 0.0001) and below (3.7 + / − 0.9; p < 0.0001) (Fig. 6).
Concerning the anatomical cadaveric part, we identified IT in all subjects analyzed (Fig. 7). On IT anterior face, we found flexor pollicis longus origin. It begins with a thin expansion under the radial tuberosity and then continues mainly on the IT anterior side and on anterior side of adjacent radial shaft. We found abductor pollicis longus attachment extending from the ulnar border and the posterior surface of the central band to the two-third proximal of the posterior IT face. Finally, extensor pollicis brevis is attached at the junction between IOM and the distal third of IT posterior surface (Fig. 8).
Muscle attachment on radial interosseous tuberosity identified during the dissection of anatomical subjects: (a) Flexor pollicis longus (forearm anterior surface)/ (b). Abductor pollicis longus (forearm posterior surface)/ (c). Abductor pollicis longus reclined, uncovering Extensor pollicis brevis (forearm posterior surface)
Central band of IOM was located entirely on the proximal two-third of IT. In seven anatomical subjects (70%), we found one or more accessory bands attached on proximal and/or distal ends of IT. Those attachment areas were always shorter than two centimeters. Finally, in five cases (50%), a dorsal oblique accessory cord was found under abductor pollicis longus origin [10, 13]. If it was present, the dorsal oblique accessory cord was attached behind the central band, at the proximal third – middle third junction of IT (Fig. 9).
a: Interosseous membrane attachment on radial interosseous tuberosity (tuberositas interossea radii). A posterior view with ulna (top) and hand (right)/ (b): zoom on radial interosseous tuberosity and interosseous membrane attachment / (c). Radial interosseous tuberosity (IT) is represented by blue hatched area with attachment of central band (white circles), proximal and two distal accessory bands (white arrows) and dorsal oblique accessory cord (white triangles)
Discussion
We confirmed the presence of an interosseous tuberosity (tuberositas interossea radii) in a very distinct portion of the interosseous margin of the radius. This relief results from a thickening of the interosseous cortex which is significantly thicker than the other cortical portions located at the same level on the radius, but also above and below. This interosseous relief serves as an attachment for two groups of structures: all extrinsic muscles of the thumb, except extensor pollicis longus; and IOM central band sometimes associated with accessory bands.
In anatomical literature, the interosseous border of the radius is classically described as extending from the area below radial tuberosity to the distal radioulnar joint [9, 12, 17]. This interosseous margin is described as a homogeneous surface, but our work clearly demonstrates that within this interosseous margin there is an individualized bone relief. The whole question is whether we can talk about tuberosity. We believe so, because a tuberosity is defined as a bony protuberance in which ligaments and/or muscles are attached [9]. These two characteristics were indeed found in this relief. Therefore, we believe that this work describes a new anatomical structure and we propose name it: the radial interosseous tuberosity.
The anatomic relief presence on a bone surface is never a coincidence. Every detail of our anatomy is the result of species long evolution which involves tough competitive selection processes. Increasing volume of a bone part responds to a biomechanical need to absorb excessive physical stress. These stresses may correspond to tensile or compressive forces. For example concerning the wrist, radial distal epiphysis is significantly larger than the ulnar and in parallel, biomechanical studies clearly show that most of longitudinal constraints transiting from wrist to forearm pass through the distal end of the radius [6]. In opposition concerning the elbow, proximal end of the ulna is significantly larger than radius head and most of longitudinal stresses between arm and forearm pass through olecranon.
With regard to IT, it is; therefore, questionable whether its existence is a result of tensile or compressive forces. There is never any contact between the radius and the ulna during the rotation of the radius. The hypothesis that this tuberosity developed in response to compressive stresses; therefore, seems inconsistent. By elimination, we make the hypothesis that the development of this tuberosity was progressively in response to tensile forces.
The central band is the thickest part of IOM whose function is to ensure radio-ulnar stability [1, 2, 4, 5]. Indeed, muscles attached from humerus to radius (pronator teres, brachioradialis, supinator) constantly tends to tract the radius-hand complex proximally. The same applies to muscles extending from humerus to the hand (flexor digitorum superficialis, palmaris longus, flexor carpi ulnaris, extensor carpi radialis brevis and longus, extensor digitorum, extensor digiti minimi) due to the radio-ulnar variance. At the wrist level, radius is longer than ulna that is why hand proximal migration produces early contact between wrist and radius and therefore pushes it proximally [7].
Another important source of longitudinal stress is direct external stress on the hand. It tends to cause radial migration outward. It is the case for example when body weight is supported directly on the palmar side by pushing, hitting or falling when landing on the hand. In total, there are therefore enormous constraints intrinsic to the upper limb or extrinsic, which tend to cause proximal radius migration. This explains central band size opposes this migration and thus contributes to forearm stability [8, 11]. However, central band function is linked to its bone attachment. Therefore, we assume that the purpose of this tuberosity is to oppose the force that tends attracting radius in a proximal direction.
It is surprising that this tuberosity has never been described since it is represented in most anatomy manuals [9, 12, 17]. This can be explained by the fact that IOM role has only been fully understood over the past twenty years. Previously, forearm stability was attributed only to proximal and distal radio-ulnar joints. The interosseous membrane simply appeared as a fibrous tissue filling the interosseous space and serving as a muscle origin. Forearm longitudinal and transverse stabilization function has been better understood in light of work on forearm instability (e.g., Essex–Lopresti syndrome) [3, 8]. Development of surgical forearm stabilization technics by central band reproduction has made it possible to focus on the radioulnar syndesmosis, which can be considered functionally as the middle radio-ulnary joint [16].
It is possible to restore most of IOM function without necessarily trying to reproduce entire membrane, but simply by central band reconstruction. All these techniques have in common the fixation of a tendon graft or synthetic ligament between radius and ulna [1, 14, 15]. The radial area fixation corresponds to central band attachment. One of the clinical applications of this work is; therefore, to highlight the close link between central band and IT, easily recognizable in fluoroscopy. Therefore, it corresponds to an intraoperative reference point useful for performing forearm stabilization techniques.
Main limitation of this study was the difficulty in determining precise limits of IT. Indeed, transitional zone between the IT and above or underlying areas is not sharp. To circumvent this limit, we used a protocol consisting of multiplying measurements by blind reviewers of their respective measures. This is a classical method used in biomedical research to reduce the bias associated with measurement uncertainty.
Conclusion
The radial interosseous tuberosity (tuberositas interossea radii) exists. It corresponds to about one-third of the interosseous border of the radius, by a cortex thickening. It may play a role in thumb function and in forearm stability with the origins of most extrinsic thumb muscles and the central band of interosseous membrane.
Code availability
Not applicable.
References
Adams JE (2017) Forearm instability: anatomy, biomechanics, and treatment options. J Hand Surg 42:47–52
Farr LD, Werner FW, McGrattan ML, Zwerling SR, Harley BJ (2015) Anatomy and biomechanics of the forearm interosseous membrane. J Hand Surg 40:1145–1151
Green JB, Zelouf DS (2009) Forearm instability. J. Hand Surg 34:953–961
Hotchkiss RN, An KN, Sowa DT, Basta S, Weiland AJ (1989) An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg 14:256–261
Loeffler BJ, Green JB, Zelouf DS (2014) Forearm instability. J. Hand Surg 39:156–167
Markolf KL, Lamey D, Yang S, Meals R, Hotchkiss R (1998) Radioulnar load-sharing in the forearm. A study in cadavera. J Bone Joint Surg Am 80:879–888
Márquez-Florez K, Vergara-Amador E, de Las Casas EB, Garzón-Alvarado DA (2015) Theoretical distribution of load in the radius and ulna carpal joint. ComputBiol Med 60:100–106
McGinley JC, Roach N, Gaughan JP, Kozin SH (2004) Forearm interosseous membrane imaging and anatomy. Skeletal Radiol 33:561–568
Keane M (2003) Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. Saunders Elsevier, Philadelphia
Moritomo H, Noda K, Goto A, Murase T, Yoshikawa H, Sugamoto K (2009) Interosseous membrane of the forearm: length change of ligaments during forearm rotation. J Hand Surg Am 34:685–691
Nakamura Y (1999) Functional anatomy of the interosseous membrane of the forearm–dynamic changes during rotation. Hand Surg 4:67–73
Netter FH (2006) Atlas of human anatomy. Saunders/Elsevier, Philadelphia
Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H (2009) Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg Am 34:415–422
Pfaeffle HJ, Stabile KJ, Li ZM, Tomaino MM (2005) Reconstruction of the interosseous ligament restores normal forearm compressive load transfer in cadavers. J Hand Surg 30:319–325
Soubeyrand M, Oberlin C, Dumontier C, Belkheyar Z, Lafont C, Degeorges R (2006) Ligamentoplasty of the forearm interosseous membrane using the semitendinosus tendon: anatomical study and surgical procedure. SurgRadiolAnat 28:300–307
Soubeyrand M, Wassermann V, Hirsch C, Oberlin C, Gagey O, Dumontier C (2011) The middle radioulnar joint and triarticular forearm complex. J Hand SurgEur 36:447–454
Standring S, Gray H (2008) Gray’s anatomy: The anatomical basis of clinical practice. Churchill Livingstone/Elsevier, Edinburgh
Acknowledgment
This manuscript has been proofread and edited by a native English-speaking proofreader.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
G. Rougereau: Data collection, Data analysis, Manuscript writing. B.Valteau: Data collection, Data analysis. M.Creze: Project development, Data management. M. Soubeyrand: Project development, Data analysis, Manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Availability of data and material
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rougereau, G., Valteau, B., Creze, M. et al. The interosseous tuberosity of radius: a descriptive radiological and cadaveric anatomical study. Surg Radiol Anat 43, 727–734 (2021). https://doi.org/10.1007/s00276-020-02594-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-020-02594-5