Abstract
Purpose
Knowledge of the wide variability in celiac trunk branches is of paramount importance when planning an abdominal surgery.
Methods
We, hereby, report a previously undescribed origin of the gastroduodenal artery discovered on an abdominal angio-CT.
Results
CT-angiogram performed on a 33-year-old female randomly revealed a new variant of gastroduodenal artery arising directly from the splenic artery along with other vascular aberrations. The latter were previously described in medical literature.
Conclusion
High-quality preoperative imaging is crucial for identification of visceral artery variations, as those can technically modify the surgical or interventional procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unique and rare anatomic variations are interesting to report because they might modify therapeutic and surgical approaches. Variations in hepatic vascularization formed the topic of multiple studies, whereas very few studies were held on the gastroduodenal artery.
Clinical case
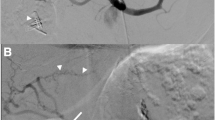
A 33-year-old female, with no prior significant medical history, underwent an abdominal CT-angiogram for demonstration of a right renal artery stenosis suspected on a Doppler ultrasound. Evaluation of the visceral arterial vascularization revealed some curious aberrances with unorthodox origins of the branches of the celiac trunk (see Fig. 1). In fact, the celiac trunk was totally absent, with the left gastric artery and the splenic artery arising independently and directly from the aorta above the origin of the superior mesenteric artery. The common hepatic artery was replaced by an aberrant proper hepatic artery arising from the superior mesenteric artery and splitting into a right hepatic artery and a left hepatic artery. The previously unreported finding was a replaced gastroduodenal artery taking origin from the splenic artery instead of the common hepatic artery.
Discussion
Tandler explained the morphogenesis of the visceral vascularization and the causes of possible aberrancies based on a study held on mole embryos [7]. Initially, the aorta gives three arterial arches for each metamere: a posterolateral arch for vertebral and parietal vascularization, a middle arch for gonadic and urinary vascularization and a median arch giving the primitive intestinal metameric arteries for visceral and splanchnic vascularization. Those primitive intestinal arteries are highly connected via ventral longitudinal anastomoses. During embryologic development, intestinal arteries and their ventral anastomoses regress progressively and by the 9th week of gestation, only intestinal arteries of the 10th, 13th, 21st and 22nd metameres persist and converge to form the celiac trunk, the superior mesenteric artery and the inferior mesenteric artery. By the end of the 12th week of gestation, the abdominal vascularization is definitive. The unusual regression of one of those four median arches or the persistence of other metameric median arches or aberrant ventral anastomoses will result in multiple variations in splanchnic arterial vascularization.
Classically, the celiac trunk arises anteriorly from the aorta at the level of T12–L1 and splits in 55–89% of cases into the left gastric artery, the splenic artery and the common hepatic artery [4]. Absence of celiac trunk is found in only 0.6% of cases [2].
The splenic artery arises most commonly from the celiac trunk, with 70% of cases having a common origin with the common hepatic artery, known as the hepato-splenic trunk [4]. Aberrant origins of the splenic artery were described in medical literature, with a splenic artery arising from the left gastric artery, the pancreatic artery, the superior mesenteric artery or as in our case directly from the aorta [6].
Common hepatic artery is defined as the portion coursing from the celiac trunk to the origin of the gastroduodenal artery, whereas the proper hepatic artery is the portion coursing from the origin of the gastroduodenal artery to the liver, splitting at the hepatic hilum into right lobe hepatic artery and left lobe hepatic artery. Numerous variations of hepatic vascularization were described, of which the most common variant is the absence of the common hepatic artery (1.4–12%) [8] which is the case of our patient. When common hepatic artery is absent, the hepatic vascularization is maintained by the left hepatic artery and/or the right hepatic artery. In our case, the common hepatic artery is absent and the proper hepatic artery originates from the superior mesenteric artery splitting into right hepatic and left hepatic arteries.
Identification of hepatic artery variants is of paramount importance preoperatively when planning for oncologic procedures requiring manipulation of major vessels in hepatobiliary, gastroesophageal and pancreatic area. This may involve longer operative time and consequently higher postoperative morbidity and mortality [5]. They also add complexity to the surgical procedure. For example, an aberrant right hepatic artery originating from the superior mesenteric artery, such as in our case, has high chances of being injured during pancreaticoduodenectomy for cephalo-pancreatic tumors. Its injury might affect the liver and the gut which may become necrotic as well as the bile ducts with the risk of leak in the bilioenteric anastomosis [3]. Invasive radiologists should also be aware of these variations, since a false identification of a major vessel could lead to an unsuccessful treatment or even a fatal complication during infusion therapy or transarterial chemoembolization of liver neoplasms.
As for the gastroduodenal artery, it is a small vessel that delivers blood to the pylorus, the proximal part of the duodenum and the head of the pancreas. It is recognized on axial images by its anterior path along the head of the pancreas as well as its typical branches. In fact, it gives rise to: (1) the right gastroepiploic artery which irrigates the greater curvature of the stomach and anastomoses with the left gastroepiploic artery (branch of the splenic artery); (2) the posterior superior pancreaticoduodenal artery which irrigates part of the duodenum and the head of the pancreas and anastomoses with the posterior inferior pancreaticoduodenal artery (branch of the superior mesenteric artery); (3) the anterior superior pancreaticoduodenal artery which passes on the anterior face of the pancreas and anastomoses with the anterior inferior pancreaticoduodenal artery (branch of the superior mesenteric artery) and (4) other possible ramifications such as the supraduodenal artery, the infrapyloric artery, some pancreatic and anterior duodenal ramifications. The gastroduodenal artery most commonly originates from the common hepatic artery (75% of cases [5]).
However, when the common hepatic artery is absent, the gastroduodenal artery might have many possible origins (see Fig. 2). Till today, there is no reported case of a gastroduodenal artery arising from the splenic artery. Inversely to the current report of a gastroduodenal artery arising directly from the splenic artery, Slaba et al. previously reported the case of a splenic artery arising directly from the gastroduodenal artery [6].
Variations in origin of gastroduodenal artery [1]
Conclusion
By this case report, we would like to emphasize the necessity of high-quality preoperative imaging using nowadays multidetector CT angiography that is far less invasive than regular arteriographies for identification of aberrant visceral arterial anatomy. This practically assumes significance in guiding abdominal surgeons performing hepatobiliary, pancreatic or gastric tumor resection, as variants of visceral arteries may be technically demanding, or when evaluating patients prior to a liver transplantation, and even for interventional radiologists performing arteriography to avoid potential iatrogenic injury and lethal complications.
References
Bergman R, Afifi A, Miyauchi R (1995) Variations in origin of gastroduodenal artery. In: Illustrated encyclopedia of human anatomic variation: opus II: cardiovascular system. http://www.anatomyatlases.org/AnatomicVariants/Cardiovascular/Images0001/0017.shtml. Accessed 16 July 2018
Iezzi R, Cotroneo AR, Giancristofaro D, Santoro M, Storto ML (2008) Multidetector-row CT angiographic imaging of the celiac trunk: anatomy and normal variants. Surg Radiol Anat 30(4):303–310. https://doi.org/10.1590/0100-3984.2014.0041
Jah A, Jamieson N, Huguet E, Praseedom R (2009) The implications of the presence of an aberrant right hepatic artery in patients undergoing a pancreaticoduodenectomy. Surg Today 39:669–674. https://doi.org/10.1007/s00595-009-3947-3
Michels NA (1995) Blood supply and anatomy of the upper abdominal organs with a descriptive atlas. Lippincott, Philadelphia
Natsis K, Piagkou M, Stamatopoulos T, Spyridakis I, Apostolidis S (2017) Anastomotic loop between common hepatic artery and gastroduodenal artery in coexistence with an aberrant right hepatic artery. Folia Morphol 76(4):752–756. https://doi.org/10.5603/FM.a2017.0023
Slaba S, Karam R, Ingea H, Haddad S, Noun R, Aoun N, Atallah N (1998) Aberrant origin of the splenic artery. J Radiol 79:434–435
Tandler J (1904) Uber die varietaten der Arteria coeliaca und deren Entwicklung. Anat Hft 25:473–500
Wind GG, Valentine RJ (1991) Anatomic exposures in vascular surgery. Lippincott Williams & Wilkins, Philadelphia
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Samy Slaba: project development and manuscript editing. Sarah Assaf: data analysis and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Slaba, S., Assaf, S. Aberrant gastroduodenal artery with splenic origin. Surg Radiol Anat 40, 1437–1440 (2018). https://doi.org/10.1007/s00276-018-2112-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-018-2112-3