Abstract
Purpose
To assess the efficacy and safety of a newly developed fully covered irradiation stent (FCIS) compared with a partially covered irradiation stent (PCIS) in patients with unresectable malignant dysphagia.
Materials and Methods
Data of 195 patients [158 (81.0%) males, median age of 75 years (range 49–89 years)] who underwent FCIS or PCIS placement for unresectable malignant dysphagia from January 2012 to November 2017 were retrospectively analyzed. The median follow-up time was 181 days (range 4–547 days). Outcomes were measured in terms of recurrent dysphagia (primary), technical success, clinical success, overall survival, and adverse events. Recurrent dysphagia was analyzed by Fine–Gray regression model.
Results
The technical success rate was 97.8% (87/89) in the FCIS group and 99.1% (105/106) in the PCIS group (P = 0.59). The clinical success rate was 100.0% in both groups. There was no statistically significant difference in the recurrent dysphagia rate between the FCIS and PCIS groups (21.8% vs. 28.6%; P = 0.12). Compared with PCISs, FCISs were associated with a decrease in tissue/tumor growth rate (11.5% vs. 21.9%; P = 0.01), while stent migration rates were statistically comparable (11.5% vs. 5.7%; P = 0.23). The median overall survivals were comparable between the FCIS and PCIS groups (164 days vs. 162 days; P = 0.70). A dysphagia score of 4 and metastasis were risk factors for survival. No significant differences were observed in the rates of adverse events, including chest pain, fistula formation, hemorrhage, and aspiration pneumonia (P > 0.05).
Conclusion
For patients with unresectable malignant dysphagia, this newly developed FCIS can provide efficacy and safety comparable to those of a PCIS. Compared with PCIS, this FCIS is more successful in preventing tissue/tumor growth, with a comparable stent migration rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant dysphagia is the major symptom of patients with esophageal or gastric cardia cancer. Surgical resection is the first-line treatment for early-stage esophageal and gastric cardia cancers; however, more than 50% of patients are identified at an advanced stage and are not eligible for surgery [1]. Patients with unresectable malignant dysphagia should be considered for palliative treatment. Placement of self-expandable metallic stents (SEMSs) and intraluminal brachytherapy are well-established procedures for the palliative treatment of malignant dysphagia [2]. SEMS placement provides rapid palliation of dysphagia, while intraluminal brachytherapy provides a durable effect on malignant dysphagia [3].
A partially covered irradiation stent (PCIS) loaded with iodine-125 (125I) seeds, which combines the advantages of SEMS placement and intraluminal brachytherapy, has been clinically used in China [4, 5]. A multicenter randomized controlled trial (RCT) demonstrated that, compared to a partially covered SEMS, this PCIS can offer longer relief of dysphagia and can prolong the survival in patients with advanced esophageal cancer [6]. However, PCIS placement did not reduce recurrent dysphagia, which was mainly caused by tissue/tumor growth. The recurrent dysphagia rate was up to 28–37% [5, 6] in patients who underwent PCIS placement, and this rate was similar to those reported in studies of common partially covered SEMSs (22–40%) [7,8,9].
In the past few years, various fully covered SEMSs have been designed and used in patients with malignant dysphagia, especially if they are receiving additional palliative therapy and require stent removal [10]. Because of the fully covered flanges, fully covered SEMSs could cause less tissue/tumor ingrowth than partially covered SEMSs may cause, with the potential disadvantage of a higher risk of stent migration [11, 12]. Therefore, it seems logical that a fully covered irradiation stent (FCIS) with anti-migration properties would be more favorable in preventing tissue/tumor growth and reducing recurrent dysphagia when compared with a PCIS.
Recently, a newly developed segmented FCIS loaded with 125I seeds was commercially available and clinically used in China. To the best of our knowledge, this is the first study to verify the roles of this newly developed FCIS in unresectable malignant dysphagia. The aim of this study is to assess the efficacy (with a particular focus on recurrent dysphagia) and safety of this FCIS compared with the PCIS in patients with unresectable malignant dysphagia.
Materials and Methods
Patients
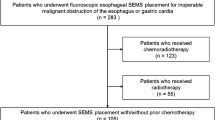
This retrospective study was approved by the institutional review board of the authors’ center. Electronic medical records of 210 consecutive patients who underwent FCIS or PCIS placement for unresectable malignant dysphagia in the authors’ center from January 2012 to November 2017 were reviewed. The PCIS was used from January 2012 to April 2016, and the FCIS was used from January 2015 to November 2017. Patients with a history of previous esophageal stent placement (n = 15) were excluded from this study. Of the remaining 195 patients, 89 were in the FCIS group and 106 in the PCIS group. The FCIS and PCIS groups were balanced in terms of demographic and clinical characteristics (Table 1). Per-protocol (PP) analysis was performed in 192 patients (Fig. 1).
Features of Stents
Both PCIS (Nanjing Micro-Tech, Nanjing, China) and the newly developed FCIS (Nanjing Micro-Tech) were dumbbell-shaped and constructed of nitinol wires. Both stents were covered with a silicon membrane, which is attached by the dipping method. The PCIS has a fully covered body with uncovered flanges on either end, while the FCIS has a fully covered body and flanges, with an extended 5-mm-long silicone layer on both ends. The body of FCIS is composed of several separate segments connected with 4–5-mm-long nylon wires, making it more flexible than an entirely braided one. Sheaths (4.8 mm long and 0.8 mm wide) were attached to the outer surface of the body. These sheaths can act as anti-migration struts and carriers of 125I radioactive seeds (CIAE-6711; Chinese Atomic Energy Science Institution, Beijing, China). The diameters of the stents are 16/22, 18/24, 20/26 mm (body/flange) at full expansion. Both stents would slightly foreshorten because of their design (Fig. 2).
The tissue penetration of each 125I seed was 20 mm, with a half-life of 59.4 days. The seeds were loaded into the sheaths immediately prior to stent placement. The number, activity, dose, and distribution of 125I seeds were determined according to the treatment planning system (TPS, University of Beijing Aeronautics and Astronautics, Beijing, China).
Procedure
The placement of irradiation stents was performed under a C-arm angiographic unit by two interventional radiologists (J.-H.G. and G.-Y.Z.) with ≥ 20 years of experience. A 5-F catheter was inserted transorally across the stricture and into the stomach, and then, iodinated contrast medium was injected via the catheter to confirm the stricture. A 0.035-inch guidewire (Amplatz Super Stiff; Boston Scientific, Natick, MA, USA) was exchanged through the catheter. A stent delivery catheter was then passed over the guidewire, and the stent was deployed on the lesion (Fig. 3). A stent at least 4 cm longer than the stricture was chosen to allow for a minimum of 2 cm extension on each side of the lesion. A balloon catheter (16/60 mm, Maxi LD, Cordis, Milpitas, CA, USA) was used to dilate the stricture if necessary.
A 72-year-old male underwent fully covered irradiation stent placement for malignant dysphagia caused by esophageal squamous cell carcinoma. A Esophagography showed a filling defect at the middle thoracic esophagus. B The stent delivery catheter, containing a 18 mm × 100 mm fully covered segmented stent loaded with 20 125I seeds, was passed over the guidewire and deployed across the stricture. C The irradiation stent was deployed in the target position. D Esophagography showed good flexibility of the stent and good passage of contrast medium through the stent
Follow-Up
Patients were required to undergo routine follow-up every month for the first 3 months and every 3 months thereafter. Clinical signs and imaging examinations (esophagography, CT scan, or endoscopy) were recorded. Patients who were unable to return for evaluation were followed up by phone. When dysphagia recurred, esophagography and/or endoscopic examination was performed.
Outcomes and Definitions
The primary outcome was recurrent dysphagia, defined as the recurrence of obstructive symptoms caused by tissue/tumor growth, stent migration, food obstruction, or stent fracture. Tissue/tumor growth was considered when soft tissue masses adjoining the stent were found by imaging examinations. The secondary outcomes included technical success, clinical success, overall survival, and adverse events. Technical success was defined as the placement of the stent in the target position and good passage of contrast medium through the stent. The dysphagia score used in this study was set by Ogilvie et al. [13]: 0, no dysphagia; 1, some solid diet; 2, semi-solid diet; 3, fluids only; and 4, complete dysphagia. Clinical success was defined as the relief of dysphagia with a decrease of at least one point in the dysphagia score within 3 days after successful stent placement. Adverse events after stent placement were evaluated according to Common Terminology Criteria for Adverse Events version 4.03 (CTCAE v4.03).
Statistical Analysis
Continuous data were analyzed with the independent-sample t test or the Mann–Whitney U test, and categorical data were analyzed with the Chi-square test or Fisher’s exact test. In the analysis of competing risk data, methods of standard survival analysis can lead to biased results [14]. Therefore, recurrent dysphagia, subdivided into tissue/tumor growth and stent migration, was analyzed by the cumulative incidence function (CIF)-based Fine–Gray competing risk regression model on the sub-distributional hazard ratio (SHR) [15]. Death was considered a competing event when analyzing recurrent dysphagia. Overall survival was estimated according to the Kaplan–Meier method and compared using the log-rank test. Predictive factors for survival were evaluated using the Cox proportional hazards model, and those factors with a P value of< 0.10 in the univariate analysis were entered into the subsequent multivariate analysis. A P value < 0.05 was considered statistically significant. All analyses were performed using STATA 14 (Stata Corp LP, College Station, TX, USA).
Results
Primary Outcome
Table 2 shows the cumulative rate of recurrent dysphagia at 3 months, 6 months, and at the time of the last follow-up in the two groups. The total rates of recurrent dysphagia were 21.8% for the FCIS group and 28.6% for the PCIS group, and no significant difference was found between the groups (SHR 0.63; 95% CI 0.35–1.12; P = 0.12; Fig. 4A).
Cumulative incidence of recurrent dysphagia from Fine–Gray model for stent types. A The cumulative incidence of recurrent dysphagia was statistically comparable in both groups (SHR 0.63; 95% CI 0.35–1.12; P = 0.12). Compared with the PCIS group, the FCIS group had B a lower tissue/tumor growth rate (SHR 0.39; 95% CI 0.19–0.81; P = 0.01), and C a comparable stent migration rate (SHR 1.86; 95% CI 0.68–5.10; P = 0.23). SHR, sub-distributional hazard ratio; FCIS, fully covered irradiation stent; PCIS, partially covered irradiation stent
Compared with the PCIS group, the FCIS group had a significantly lower tissue/tumor growth rate (11.5% vs. 21.9%; SHR 0.39; 95% CI 0.19–0.81; P = 0.01; Fig. 4B), and the type of stent was the only independent risk factor for tissue/tumor growth (Table 3). Tissue/tumor growth (n = 34) was treated by additional SEMS placement (n = 19), additional irradiation stent placement (n = 11), nasointestinal tube insertion (n = 2), or gastrostomy (n = 2).
Stent migration rates were statistically comparable between the two groups (11.5% for the FCIS group and 5.7% for the PCIS group; SHR 1.86; 95% CI 0.68–5.10; P = 0.23; Fig. 4C). One patient with stent migration did not experience recurrent dysphagia because there were no obvious dysphagia symptoms until his death 31 days later. In the FCIS group, 9 of 10 patients (90.0%) underwent successful stent retrieval, and 1 patient refused stent removal; in the PCIS group, 5 of 6 patients (83.3%) underwent successful stent retrieval, and the procedure failed in 1 patient (P > 0.99). Reinterventions included SEMS placement (n = 6), irradiation stent placement (n = 6), nasointestinal tube insertion (n = 2), parenteral nutrition (n = 1), and follow-up (n = 1). No food obstruction or stent fracture was found in this study.
Secondary Outcomes
The technical success rate was 97.8% (87/89) in the FCIS group and 99.1% (105/106) in the PCIS group (P = 0.59). Three cases of misplacement occurred, and an additional covered SEMS was deployed to cover the residual stricture. The matched peripheral dose at the reference point (10 mm from the stent surface) was approximately 35–45 Gy (Fig. 5). The clinical success rate was 100.0% in both groups. The mean dysphagia scores decreased from 3.28 ± 0.45 to 1.13 ± 0.63 in the FCIS group and from 3.35 ± 0.48 to 1.29 ± 0.51 in the PCIS group (each P < 0.01) within 3 days, and there was no difference in the variance between the two groups (P = 0.36).
The median follow-up time was 181 days (range 4–534 days) in the FCIS group and 181 days (range 4–547 days) in the PCIS group (P = 0.63). The median overall survival was 164 days (95% CI 134–194) in the FCIS group and 162 days (95% CI 134–190) in the PCIS group (P = 0.70; Fig. 6A). Univariate analysis demonstrated significant association of overall survival with pathology, dysphagia score before stent placement, ECOG score, and metastasis. In the multivariate analysis, a dysphagia score of 4 before stent placement (HR 1.54; 95% CI 1.07–2.23; P = 0.02; Fig. 6B) and metastasis (HR 3.85; 95% CI 2.53–5.85; P < 0.01; Fig. 6C) were jointly demonstrated as risk factors for survival (Table 4).
Kaplan–Meier curves for overall survival. A The overall survival was statistically comparable in both groups (P = 0.70). Multivariate analysis for Cox model showed that B a dysphagia score of 4 (HR 1.54; 95% CI 1.07–2.23; P = 0.02) and C metastasis (HR 3.85; 95% CI 2.53–5.85; P < 0.01) were risk factors for survival. HR, hazard ratio; FCIS, fully covered irradiation stent; PCIS, partially covered irradiation stent
Rates of adverse events, including chest pain, fistula formation, hemorrhage, and aspiration pneumonia, did not differ between the two groups (Table 5). A total of 31 events of grade ≥ 3 were recorded in 25 patients: 11 were in the FCIS group and 14 in the PCIS group (12.6% vs. 13.3%; P = 0.89). Chest pain was the most common adverse event. Seventy-seven patients (40.1%) reported mild retrosternal discomfort, which was tolerable and relieved spontaneously within 3 days. For patients who experienced moderate or severe chest pain, narcotic analgesics were used depending on the severity. All four tracheoesophageal fistulas were treated by the insertion of an additional covered SEMS. Of the eight patients who suffered grade ≥ 3 hemorrhage, two (one in each group) survived after blood transfusion, while six (three in each group) died. Aspiration pneumonia occurred in nine patients, and all of them recovered with medical intervention.
Discussion
The main goal of stent placement in patients with unresectable malignant dysphagia is to provide rapid and persistent relief of dysphagia. In this study, rapid relief was achieved comparably in both groups within 3 days after stent placement. It was hypothesized that the newly developed FCIS would provide less recurrent dysphagia than would a PCIS. However, although the recurrent dysphagia rate is numerically lower in the FCIS group (21.8% vs. 28.6%), there was no statistically significant difference between the FCIS and PCIS groups. This result was driven by different tissue/tumor growth rates and comparable stent migration rates.
The newly developed FCIS provided a significantly lower tissue/tumor growth rate than did the PCIS, which may be caused by the extended silicone layer at both ends as well as the design of the segmented stent. Compared with the straight tubular stent used in the PCIS group, the segmented stent provides lower axial force, which could make the stent adapt better to the local esophageal anatomy and cause less trauma to the esophageal wall [16]. A similar design of the segmented stent was previously reported by Shim and his colleagues [17]. However, to prevent stent fracture, connecting wires between adjacent segments are added on the basis of their design.
Compared with partially covered SEMSs, fully covered SEMSs were reported to be associated with a higher risk of stent migration [11]. In studies on common, commercially available fully covered SEMSs, the stent migration rate varied from 5.0 to 20.0% in patients with unresectable malignant dysphagia [7, 18,19,20]. Concomitant chemoradiotherapy was also considered to be a risk factor for stent migration, with a migration rate of 9.6–31.0% [21,22,23]. To prevent stent migration, several designs were applied, including the dumbbell-shaped flanges, the attached seed sheaths, which act as anti-migration struts, and the segmented stent, which is beneficial to keep both stent and seed sheaths in an adequate position in the esophagus. The stent migration rate was 11.5% in the FCIS group, which we think is acceptable, although this rate is numerically higher than that in the PCIS group (5.7%). Unlike tissue/tumor growth, stent migration could often be viewed as a positive finding, because it implies that the patient is responding to brachytherapy. In this study, no radioactive seed loss, acute gastritis, ulceration, or perforation was found after stent migration; thus, we believe that migrated irradiation stents would not cause additional injury to the patient.
Compared with the conventional partially covered SEMSs, PCISs prolonged the survival in patients with unresectable esophageal cancer in a meta-analysis [24]. In this study, FCISs did not provide a survival advantage over PCISs. In the multivariate analysis, metastasis and a dysphagia score of 4 before stent placement were associated with poorer survival. Patients with metastasis were in a more advanced stage, while brachytherapy merely provides local treatment; thus, it seems logical that their survival was shorter. A higher dysphagia score was often associated with greater tumor volume, which may lead to incomplete elimination of tumor tissue. A higher dysphagia score was also reported as a risk factor for survival in the study on the conventional fully covered SEMSs [25].
In this study, we used CTCAE v4.03 to define and classify adverse events. Compared with other studies on esophageal stents, higher rates of chest pain and hemorrhage were reported in our study. This is because different criteria were used and more mild cases which did not require additional intervention were recorded in this study. Theoretically, a flexible SEMS, such as FCIS, may reduce trauma-related adverse events, including chest pain, fistula formation, and hemorrhage, but no significant difference was observed.
This study had several limitations. First, in this single-center retrospective study, there were 43 patients lacking complete follow-up data and no strict guideline on stent choice; therefore, information bias and selection bias may exist. Besides, from January 2012 to December 2014, PCIS was the only option, so there may exist time bias. Further RCT is therefore required. Second, the quality of life was not analyzed in our study due to the insufficient data of a retrospective study. Finally, all stents were placed under fluoroscopy, and the feasibility of endoscopic placement warrants further investigation.
In conclusion, for patients with unresectable malignant dysphagia, this newly developed FCIS can provide comparable efficacy and safety to PCIS, but is more successful in preventing tissue/tumor growth considering a comparable stent migration rate. This sets the preference for the newly developed FCIS over the conventional PCIS for the treatment of unresectable malignant dysphagia.
References
Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390(10110):2383–96. https://doi.org/10.1016/S0140-6736(17)31462-9.
Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell A, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2016;48(10):939–48. https://doi.org/10.1055/s-0042-114210.
Homs MY, Steyerberg EW, Eijkenboom WM, Tilanus HW, Stalpers LJ, Bartelsman JF, et al. Single-dose brachytherapy versus metal stent placement for the palliation of dysphagia from oesophageal cancer: multicentre randomised trial. Lancet. 2004;364(9444):1497–504. https://doi.org/10.1016/S0140-6736(04)17272-3.
Zhongmin W, Xunbo H, Jun C, Gang H, Kemin C, Yu L, et al. Intraluminal radioactive stent compared with covered stent alone for the treatment of malignant esophageal stricture. Cardiovasc Interv Radiol. 2012;35(2):351–8. https://doi.org/10.1007/s00270-011-0146-6.
Guo JH, Teng GJ, Zhu GY, He SC, Fang W, Deng G, et al. Self-expandable esophageal stent loaded with 125I seeds: initial experience in patients with advanced esophageal cancer. Radiology. 2008;247(2):574–81. https://doi.org/10.1148/radiol.2472070999.
Zhu HD, Guo JH, Mao AW, Lv WF, Ji JS, Wang WH, et al. Conventional stents versus stents loaded with (125)iodine seeds for the treatment of unresectable oesophageal cancer: a multicentre, randomised phase 3 trial. Lancet Oncol. 2014;15(6):612–9. https://doi.org/10.1016/S1470-2045(14)70131-7.
Didden P, Reijm AN, Erler NS, Wolters LMM, Tang TJ, Ter Borg PCJ, et al. Fully vs. partially covered self-expandable metal stent for palliation of malignant esophageal strictures: a randomized trial (the COPAC study). Endoscopy. 2018;50(10):961–71. https://doi.org/10.1055/a-0620-8135.
van Heel NC, Haringsma J, Boot H, Cats A, Vanhoutvin SA, Kuipers EJ. Comparison of 2 expandable stents for malignant esophageal disease: a randomized controlled trial. Gastrointest Endosc. 2012;76(1):52–8. https://doi.org/10.1016/j.gie.2012.02.050.
van Boeckel PG, Repici A, Vleggaar FP, Solito B, Rando G, Cortelezzi C, et al. A new metal stent with a controlled-release system for palliation of malignant dysphagia: a prospective, multicenter study. Gastrointest Endosc. 2010;71(3):455–60. https://doi.org/10.1016/j.gie.2009.09.046.
Hourneaux de Moura EG, Toma K, Goh KL, Romero R, Dua KS, Felix VN, et al. Stents for benign and malignant esophageal strictures. Ann N Y Acad Sci. 2013;1300:119–43. https://doi.org/10.1111/nyas.12242.
Reijm AN, Didden P, Schelling SJC, Siersema PD, Bruno MJ, Spaander MCW. Self-expandable metal stent placement for malignant esophageal strictures—changes in clinical outcomes over time. Endoscopy. 2019;51(1):18–29. https://doi.org/10.1055/a-0644-2495.
Seven G, Irani S, Ross AS, Gan SI, Gluck M, Low D, et al. Partially versus fully covered self-expanding metal stents for benign and malignant esophageal conditions: a single center experience. Surg Endosc. 2013;27(6):2185–92. https://doi.org/10.1007/s00464-012-2738-x.
Ogilvie AL, Dronfield MW, Ferguson R, Atkinson M. Palliative intubation of oesophagogastric neoplasms at fibreoptic endoscopy. Gut. 1982;23(12):1060–7.
Kim HT. Cumulative incidence in competing risks data and competing risks regression analysis. Clin Cancer Res. 2007;13(2 Pt 1):559–65. https://doi.org/10.1158/1078-0432.CCR-06-1210.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. https://doi.org/10.2307/2670170.
Hirdes MM, Vleggaar FP, de Beule M, Siersema PD. In vitro evaluation of the radial and axial force of self-expanding esophageal stents. Endoscopy. 2013;45(12):997–1005. https://doi.org/10.1055/s-0033-1344985.
Shim CS, Jung IS, Bhandari S, Ryu CB, Hong SJ, Kim JO, et al. Management of malignant strictures of the cervical esophagus with a newly-designed self-expanding metal stent. Endoscopy. 2004;36(6):554–7. https://doi.org/10.1055/s-2004-814555.
Repici A, Jovani M, Hassan C, Solito B, Di Mitri R, Buffoli F, et al. Management of inoperable malignant oesophageal strictures with fully covered WallFlex((R)) stent: a multicentre prospective study. Dig Liver Dis. 2014;46(12):1093–8. https://doi.org/10.1016/j.dld.2014.08.037.
Kim ES, Jeon SW, Park SY, Cho CM, Tak WY, Kweon YO, et al. Comparison of double-layered and covered Niti-S stents for palliation of malignant dysphagia. J Gastroenterol Hepatol. 2009;24(1):114–9. https://doi.org/10.1111/j.1440-1746.2008.05674.x.
Persson J, Smedh U, Johnsson A, Ohlin B, Sundbom M, Nilsson M, et al. Fully covered stents are similar to semi-covered stents with regard to migration in palliative treatment of malignant strictures of the esophagus and gastric cardia: results of a randomized controlled trial. Surg Endosc. 2017;31(10):4025–33. https://doi.org/10.1007/s00464-017-5441-0.
Fuccio L, Scagliarini M, Frazzoni L, Battaglia G. Development of a prediction model of adverse events after stent placement for esophageal cancer. Gastrointest Endosc. 2016;83(4):746–52. https://doi.org/10.1016/j.gie.2015.08.047.
Siddiqui AA, Sarkar A, Beltz S, Lewis J, Loren D, Kowalski T, et al. Placement of fully covered self-expandable metal stents in patients with locally advanced esophageal cancer before neoadjuvant therapy. Gastrointest Endosc. 2012;76(1):44–51. https://doi.org/10.1016/j.gie.2012.02.036.
Mezes P, Krokidis ME, Katsanos K, Spiliopoulos S, Sabharwal T, Adam A. Palliation of esophageal cancer with a double-layered covered Nitinol stent: long-term outcomes and predictors of stent migration and patient survival. Cardiovasc Interv Radiol. 2014;37(6):1444–9. https://doi.org/10.1007/s00270-013-0829-2.
Chen HL, Shen WQ, Liu K. Radioactive self-expanding stents for palliative management of unresectable esophageal cancer: a systematic review and meta-analysis. Dis Esophagus. 2017;30(5):1–16. https://doi.org/10.1093/dote/dow010.
So H, Ahn JY, Han S, Jung K, Na HK, Lee JH, et al. Efficacy and safety of fully covered self-expanding metal stents for malignant esophageal obstruction. Dig Dis Sci. 2018;63(1):234–41. https://doi.org/10.1007/s10620-017-4839-9.
Acknowledgements
This study was funded by the Jiangsu Provincial Special Program of Social Development (BE2016783).
Funding
This study was funded by the Jiangsu Provincial Special Program of Social Development (BE2016783).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
For this type of study, consent for publication is not required.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This work was performed with the approval of the local ethics committee. For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study. This study was approved by our institutional review board, and the requirement for written informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, C., Lu, J., Wang, Y. et al. A New Fully Covered Irradiation Stent Versus a Partially Covered Irradiation Stent for Unresectable Malignant Dysphagia: A Single-Center Experience. Cardiovasc Intervent Radiol 42, 1142–1152 (2019). https://doi.org/10.1007/s00270-019-02252-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02252-3