Abstract
Objective
This study was designed to compare the clinical effectiveness of intraluminal radioactive stent loaded with iodine-125 seeds implantation versus covered stent alone insertion in patients with malignant esophageal stricture.
Methods
We studied two groups of patients with malignant esophageal stricture. Group A comprised 28 patients (19 men and 9 women) who underwent intraluminal radioactive stent loaded with iodine-125 seeds implantation and were followed prospectively. Group B comprised 30 patients (18 men and 12 women) who had previously received covered stent alone insertion; these patients were evaluated retrospectively. There was no crossover between the two groups during follow-up. Informed consent was obtained from each patient, and our institutional review board approved the study. The dysphagia score, overall survival rates, complication rates, and reintervention rates were compared in the two groups.
Results
There were no significant differences between the two groups in terms of baseline characteristics. Stent placement was technically successful and well tolerated in all patients. The dysphagia score was improved in both groups after stent placement. The median survival was significantly longer in group A than in group B: 11 versus 4.9 months, respectively (P < 0.001). The complications of chest pain, esophageal reflux, and stent migration was more frequent in group B, but this difference did not reach statistical significance. There was no statistical difference in reintervention between two groups.
Conclusions
Intraluminal radioactive stent loaded with iodine-125 seeds implantation was a feasible and practical management in treating malignant esophageal stricture and was superior to covered stent alone insertion, as measured by survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Esophageal carcinoma has a high mortality rate compared with other malignancies. Esophageal carcinoma can result in stenosis and obstruction or fistula combined with stenosis [1]. Esophageal stenosis, which is the main cause of dysphagia, seriously influences nutrient intake and threatens the lives of patients. Older patients who decline surgery and patients with postoperative stenosis comprise approximately 50% of all patients with advanced esophageal carcinoma [2–4].
Interventional therapy with a metal stent can help patients with advanced-stage esophageal carcinoma rebuild swallowing function. In 1983, Frimberger [5] treated esophageal stenosis with a metal stent. Placement of metal stents for esophageal stenosis has gained gradual popularity [6, 7]. However, the conventional metal stent provides only palliative treatment in mechanical support and improved eating ability, whereas intraluminal radioactive stent placement can treat the esophageal stricture much more effectively; in addition to providing mechanical expansion, intraluminal irradiation inhibits tumor growth via continuous low-dosage irradiation from the iodine-125 seeds [8]. In this study, we compared covered stent alone with intraluminal radioactive stent loaded with iodine-125 seeds to treat malignant esophageal stricture in esophageal carcinoma.
Materials and Methods
Informed consent was obtained from each patient, and our institutional review board approved this study.
Patient Population
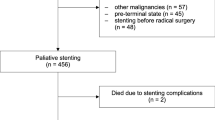
Between October 2004 and July 2008, 28 consecutive patients with malignant esophageal stricture were enrolled for selective intraluminal radioactive stent implantation (group A); for comparison, a retrospective evaluation was performed on 30 consecutive patients with malignant esophageal stricture (group B) who had received covered stent alone insertion between June 2004 and October 2008. There was no crossover between the two groups during follow-up. All patients underwent upper GI endoscopy, CT, and MRI for clinical staging. All patients had tumor invasion or compression resulting in malignant esophageal stenosis or obstruction. Oral food intake (solid or mixed food) was impossible in all patients.
Inclusion Criteria
All patients enrolled had contraindications to operative surgery or had rejected operative surgery due to personal reasons. The specific inclusion criteria for stent implantation used in this study were the following: (1) definite pathological results on CT or MRI, or other imaging evidence showing that the tumor was esophageal cancer; (2) tumor invasion or compression resulting in esophageal luminal stenosis or occlusion; (3) expected survival time longer than 1 month; (4) physical fitness score (Karnofsky score) ≥ 50; (5) no serious heart or lung, hematologic, nervous system, liver, or kidney dysfunction; and (6) no acute infection. The exclusion criteria included acute infection, severe cardiovascular or mental illness, and evidence of multiple small-bowel obstructions.
Preparation of Intraluminal Radioactive Stent
The radioactive seeds of 125I (Shanghai GMS Pharmaceutical Co., Ltd., Shanghai, China) are encased in cases of titanium alloy. Seeds specifications are as follows: 4.5 mm in length; 0.8 mm in diameter; 60.1 days of half-life; 27–35 keV mean photon energy; and 1.7 cm in tissue penetration. The initial dosage rate was 7 cGy/h. Activity per seed for clinical use is 0.80–0.90 mCi.
The system of metal stent combined with intraluminal irradiation of 125I seeds is composed of three parts: esophageal nitinol stent, covering of silicone membrane or polytetrafluoroethylene membrane, and nitinol sheaths fixed outside the membrane containing iodine seeds. According to the length of the esophageal lesion and degree of stenosis, a metal stent that provided suitable coverage was selected (Micro-tech [Nanjing] Co. Ltd, Nanjing, China). The outside of the stent was fixed with a specially designed nitinol sheath, which can contain 125I seeds. The 125I seeds were placed in the sheath with forceps according to the length and characteristics of the esophageal lesion. The seeds interval distance was 10–15 mm. Each layer contained four 125I seeds, which were placed in the same plane at 90º angles. The 125I seeds between two adjacent layers were intersected to form a diamond shape.
Fixation of 125I Seeds
A metal stent of suitable length and shape was selected by barium meal esophageal angiography. Then, according to the length of the esophageal lesion and the extent of the lesion in each layer shown by chest computed tomography (CT), Treatment Planning System (TPS) was applied for construction of a three-dimensional image of the tumor. The amount of 125I seeds to be implanted and distribution ratio of dosage were calculated. The sheaths containing 125I seeds were distributed symmetrically in a diamond shape along the axis of the stent. The seeds interval distance was approximately 10–15 mm. The researcher made certain that there would not be a “cold point” after filling the radioactive seeds in the sheath (Fig. 1).
Implantation of Metal Stent and Intraluminal Radioactive Stent
The site, severity, and length of the stricture were determined by endoscopy and esophagography before a decision was made to place a stent. Topical anesthesia of the pharynx was performed before the procedure with a 2% lidocaine spray. A Headhunter catheter (H1, Cook, Bloomington, IN) was guided with a 0.035-in. 260-cm hydrophilic guide wire (Radifocus M, Terumo, Tokyo, Japan) through the mouth to the segment of stenosis under fluoroscopic guidance; A Headhunter catheter supported the hydrophilic guidewire to pass the segment of stenosis, which then curled in the stomach. After crossing the stenosis, the hydrophilic wire was exchanged for a floppy-tipped, stiff guidewire (SuperStiff, Boston Scientific/Medi-tech, Natick, MA). The catheter was removed and a balloon catheter of a diameter of 15–20 mm was inserted. Contrast agent diluted by normal saline was injected to expand the balloon until the patient could not tolerate it. A small amount of liquid was removed for mediating the pressure to a certain degree so that the patient could bear it for 5–10 min. Another possible technique is via the utilization of balloon catheter with measuring scale for the selection of stent length to cover the lesion. Stent was inserted to the segment of stenosis by a pusher and then released. The inserting system was removed and some contrast reagent was swallowed to observe the stent implantation in the stenosis segment. If necessary, the position of the stent could be altered by balloon catheter. After it has been implanted, the distal end of the stent should be 10–20 mm beyond that the stenosis segment, and the proximal end should be approximately 20 mm above it (Figs. 2, 3).
Radiographs of a 67-year man with esophageal cancer with incomplete obstruction of the upper esophagus. A Contrast medium could barely pass the obstruction of upper esophagus (arrow). B, C After placement of intraluminal radioactive stent, water-soluble nonionic contrast medium shows good flow of contrast medium through the stent. The sheaths containing 125I seeds were distributed symmetrically in a diamond shape along the axis of the stent (arrows). D CT 3D reconstruction shows sheaths containing 125I seeds that are evenly distributed along the intraluminal radioactive stent (arrows)
Radiographs obtained of a 69-year-old man with anastomotic recurrence after radical resection of esophageal cancer involving complete obstruction of the anastomosis. A Contrast medium could barely pass the obstruction of anastomotic recurrence (arrow). B Balloon catheter of 15 mm diameter was inserted. Contrast agent diluted by normal saline was injected to expand the balloon (arrow). C After placement of intraluminal radioactive stent, the sheaths containing 125I seeds were distributed symmetrically in a diamond shape along the axis of the stent (arrow). D After placement of intraluminal radioactive stent, water-soluble nonionic contrast medium shows good flow of contrast medium through the stent (arrows). E CT 3D reconstruction shows sheaths containing 125I seeds that are evenly distributed along the intraluminal radioactive stent (arrows)
Postoperative Follow-up and Observation
Both groups underwent esophagography 1–3 days after stent placement to verify the position and patency of the stent. Patients were instructed not to start eating solid food until there was full stent expansion. After the procedure, routine blood tests, barium meal, endoscopy, chest CT, and plain X-ray were ordered at regular intervals to check for complications. Patients were advised to follow-up in the outpatient clinic. Computed tomography images were used to assess changes of the original lesions and to detect complications of perforation, fistula, or bleeding. Thereafter, patients were advised to visit the outpatient clinic and follow-up esophagography was obtained to evaluate stent patency and potential complications after 1 month for routine follow-up and then every 2 months or whenever dysphagia recurred. To assess clinical improvement, dysphagia score before and after stent placement was graded on a scale of 0 to 4 as follows, according to the CIRSE guidelines [9]: grade 0 = normal diet; 1 = ability to swallow some solid food; 2 = ability to swallow semisolids only; 3 = ability to swallow liquids only; and 4 = complete dysphagia. The score was recorded in all patients before and after intervention.
Statistical Analysis
Numeric data were expressed as mean ± standard deviation and range. Statistical significance of the parametric data was determined with the Student’s t test, and for nonparametric data with the χ2 or Fisher’s exact test. The dysphagia grades were examined with the Kruskal–Wallis test. Comparison of the complications and reinterventions related to stent placement between the two groups also was analyzed with χ2 test or Fisher’s exact test. The Kaplan–Meier method was used to analyze overall survival in both groups, and the log-rank test was used to test the statistics for equality of survival distributions between the two groups. Statistical analyses were performed using statistical software package SPSS 13.0 (SPSS, Inc., Chicago, IL). EpiData 2.0 (EpiData Association, Odense, Denmark) was used to establish the database. P < 0.05 was considered statistically significant.
Results
Patient Characteristics
Two groups of subjects were studied, and the baseline characteristics of the two groups are detailed in Table 1. There were no significant differences in the age, sex, mean tumor length, site of lesion, and dysphagia score before stent placement between the two groups. Preoperative esophageal barium, chest CT, and endoscopic and pathological examinations demonstrated all cases to be circular lesions surrounding the esophagus. Biopsy results demonstrated esophageal carcinomas. There were two pathological types: squamous cell carcinoma or adenocarcinoma. Cancer stage ranged from II to IV stage according to the clinical staging of esophageal carcinoma. The stent was successfully implanted into the target esophageal segment in all patients. No dislodgement of iodine-125 seeds was detected during the study and follow-up period. Six patients in the intraluminal radioactive stent group and five patients in the covered stent alone group received chemotherapy before stent placement. No patients in both groups were treated with chemotherapy after the stent placement. Also, no patients in both groups were treated with external beam radiation therapy (EBRT) before or after the stent placement.
Dysphagia Score
The mean degree of dysphagia before stent insertion was similar in both groups. The effect of stent placement on the dysphagia score is shown in Fig. 4. One week after stent placement, the mean dysphagia score improved significantly in both group A (3.43 ± 0.50–1.00 ± 0.77; P < 0.001) and group B (3.40 ± 0.50–1.00 ± 0.79; P < 0.001). Median dysphagia score also improved from 3 to 1 in both groups. The dysphagia score was significantly improved in both groups after stent placement (P < 0.01). However, there was no statistically significant difference in dysphagia score improvement between the two groups (P > 0.05).
Complications and Reinterventions
No procedural complications occurred in any of these study patients. Complications during follow-up and their reinterventions are shown in Table 2. Fifteen patients of group A and 24 patients of group B experienced dull chest pain for 1–3 days after the procedure, which was alleviated by the use of narcotic analgesics. The pain was worse with implanted stent in the upper two thirds of the esophagus. Postoperative esophageal reflux occurred in two patients of group A and three patients of group B who had stenosis near the cardia of stomach. Those patients were advised not to eat before sleeping. Furthermore, they were instructed to maintain a standing or sitting position after eating. Antacids were used to relieve symptoms caused by reflux. Medicines to promote gastric motility were used to decrease the occurrence of esophageal reflux. Stent migration was detected approximately 4 weeks after stent placement. One patient in group A showed complete migration of the stent into the stomach at the time of elective stent removal; one additional covered stent was implanted. In group B, two patients with stent migration were managed with stent removal and additional covered stent placement. Complications due to local irradiation of 125I seeds, such as leukopenia and gastrointestinal reaction, were not detected. The complications of chest pain, esophageal reflux, and stent migration was more frequent in group B, but this difference did not reach statistical significance.
Recurrent dysphagia occurred in all patients with restenosis. Endoscopy demonstrated tumor tissue growing into the stent from its superior margin, resulting in restenosis. One patient from group A and two patients from group B received additional covered stent placement. There was no statistical difference in reintervention between two groups.
Overall Survival
The median overall survival period was longer in group A than in group B: 11 (range, 3–18) months versus 4.9 (range, 1–12) months, respectively. This difference was statistically significant (P = 0.01, log-rank test; Fig. 5).
Discussion
Esophageal carcinoma has a poor prognosis. Because malignant esophageal tumor has no specific symptoms in its early stage, 60–80% of esophageal carcinomas are diagnosed at middle or advanced stage [10]. Surgery is not indicated for these patients, and metal stent can be used as a treatment option to relieve the dysphagia, thus improving the patients’ quality of life. This technique also facilitates chemical therapy, radiotherapy, and surgical therapy [11]. Compared with other treatments for esophageal stricture, metal stent placement has shown favorable characteristics. The procedure is relatively simple, rapidly effective, and generally well-tolerated [12, 13].
At present, implantation of covered or uncovered metal stent remains the major interventional approach to esophageal stenosis and fistula [14, 15]. However, a conventional metal stent does not provide the additional effect of local treatment and is used only for mechanical support and obstruction relief. Numerous studies have confirmed that implantation of iodine-125 radioactive seeds is a safe and effective method for the treatment of malignant tumors, including lung, liver, prostate, and pancreatic [16–19]. In the animal study, the use of iodine-125 seeds loaded metal stent in the esophageal application proved to be mechanically stable and biologically tolerable by the recipients [20]. Therefore, we performed this prospective study to evaluate the clinical effectiveness of intraluminal radioactive stents on malignant esophageal stricture. These patients were compared with a retrospective control group of patients who underwent covered stent alone insertion. The required amount of radioactive iodine-125 seeds was calculated according to the result of CT scanning and three-dimensional imaging technique of a Treatment Planning System [21]. A specially made sheath was fixed to the outside of the stent. The effective radius of the 125I seed was calculated to be between 15 and 20 mm for commonly selected beads with an activity of 22.2 MBq. To prevent the local “cold point” of irradiation caused by the irregular alignment of the seeds, seeds were aligned regularly and symmetrically in a diamond shape configuration. The seed interval was 10–15 mm. Each layer had four 125I seeds in the same plane at a 90º angle. The 125I seeds in the upper layer intersected those in the lower layer.
Implantation of esophageal stents in patients with advanced esophageal carcinoma can improve the quality of life. However, it cannot prolong the survival period significantly. It has been reported that the survival period of patients with stage II and III esophageal carcinoma is approximately 5 months; the survival period of patients with stage IV is 3.5 months [22, 23] or even shorter [24]. Guo et al. [8] reported the response to treatment with a self-expandable esophageal stent loaded with iodine-125 seeds for intraluminal brachytherapy versus the response to treatment with a conventional self-expandable covered stent in patients with advanced esophageal cancer. The median survival in the irradiation stent group was 7 months versus a median survival in the control group of 4 months. In our study, the median survival period of patients who received the implantation of intraluminal radioactive stent was 11.6 months, which is significantly longer than the survival period reported in the literature and those in group B (4.9 months; P < 0.001). This is because the esophageal intraluminal radioactive stent not only improves dysphagia but also allows intraluminal radiotherapy. Therefore, the outcome of the intraluminal radioactive stents reached statistically significance and encouraged further evaluation.
Possible complications after implantation of esophageal stents include hemorrhage, perforation, stent migration, reobstruction, and tracheoesophageal fistula [1, 25–27]. Hemorrhage has been reported in 3–8% and is usually self-limited [1]. Guo et al. [8] reported that hemorrhage occurred in 16 (30%) patients in both groups during implantation and follow-up. However, in our study, no patient with severe hemorrhage was reported. Stent migration was detected approximately 4 weeks after stent placement. One patient in group A showed complete migration of the stent into the stomach at the time of elective stent removal; one additional covered stent was implanted. In group B, two patients with stent migration were managed with stent removal and additional covered stent placement. There was no statistically significant difference in complication rates between the two groups.
The advantages of intraluminal radioactive stents for clinical application are as follows: (1) the radiating distance is short, with a distance of only approximately 1.7 cm, which eliminates any chance of injury to the physician and family; (2) the internal irradiation has a long-acting period of effectiveness, which can last as long as 180 days; (3) this method improves the effect of local therapy and decreases the general side effect of chemotherapy; and (4) the distribution of 125I seeds can be arranged selectively according to the asymmetrical growth of tumor.
Treating tumor with radioactive seeds from a short distance is a new technique developed during the last 20 years. Short-distance therapy with radioactive beads showed its advantage especially after the successful production of new, low energy, safe, and easily protective radioactive 125I and 103Pb [28], the development of ultrasound and CT imaging, and the introduction of a computerized three-dimensional therapy designing system. The intraluminal radioactive stent allows local iodine seed to provide a continuous low dosage, which can irradiate the tumor cells in different division cycles without interruption. Thus, it can effectively prevent restenosis and avoid the side effects of systemic chemotherapy.
Our study had certain limitations. First, because of the time limitation and inclusion criteria, the sample size of our study was considered small, although it reached statistical significance. Further study with bigger sample size might yield more accurate results. Second, we did not manage to include quality of life, which is one of the important parameters of outcomes for the palliative treatment, such as inoperable esophageal cancer into our study analysis.
In conclusion, our data demonstrate the intraluminal radioactive stent to be a relatively safe, feasible, and effective method to treat esophageal stenosis caused by advanced esophageal carcinoma. The method is improving continuously with the development of newer materials and techniques. Its long-term prognosis and effectiveness should be evaluated by further observation and research.
References
Katsanos K, Sabharwal T, Adam A (2010) Stenting of the upper gastrointestinal tract: current status. Cardiovasc Interv Radiol 33:690–705
Park JG, Jung GS, Oh KS et al (2010) Double-layered PTFE-covered nitinol stents: experience in 32 patients with malignant esophageal strictures. Cardiovasc Interv Radiol 33:772–779
Kim KR, Shin JH, Song HY et al (2009) Palliative treatment of malignant esophagopulmonary fistulas with covered expandable metallic stents. AJR Am J Roentgenol 193:W278–W282
White RE, Parker RK, Fitzwater JW et al (2009) Stents as sole therapy for oesophageal cancer: a prospective analysis of outcomes after placement. Lancet Oncol 10:240–246
Frimberger E (1983) Endoscopic treatment of benign esophageal stricture. Endoscopy 1:199–202
Song HY, Park SI, Do YS et al (1997) Expandable metallic stent placement in patients with benign esophageal strictures: results of long-term follow-up. Radiology 203:131–136
Zelenák K, Mistuna D, Lúcan J et al (2010) Broken esophageal stent successfully treated by interventional radiology technique. Cardiovasc Interv Radiol 33:643–645
Guo JH, Teng GJ, Zhu GY et al (2008) Self-expandable esophageal stent loaded with 125I seeds initial experience in patients with advanced esophageal cancer. Radiology 247:574–581
Sabharwal T, Morales JP, Irani FG, Adam A (2005) Quality improvement guidelines for placement of esophageal stents. Cardiovasc Interv Radiol 28:284–288
Huang GJ, Wang LJ, Liu JS et al (1985) Surgery of esophageal carcinoma. Semin Surg Oncol 1:74–83
Cwikiel W, Tranberg KG, Cwikiel M et al (1998) Malignant dysphagia: palliation with esophageal stents-long-term results in 100 patients. Radiology 207:513–518
McQueen AS, Eljabu W, Latimer J et al (2011) Thoracic discitis as a complication of self-expanding metallic stents in esophageal carcinoma. Cardiovasc Interv Radiol 34(Suppl 2):S300–S302
Wenger U, Luo J, Lundell L et al (2005) A nationwide study of the use of self-expanding stents in patients with esophageal cancer in Sweden. Endoscopy 37:329–334
Richard R, Katherine EM, Paul CL et al (1997) Malignant esophageal and esophagorespiratory fistula: palliation with polyethylene covered Z-stent. Radiology 202:349–354
Shin JH, Song HY, Ko GY et al (2004) Esophagorespiratory fistula: long-term results of palliative treatment with covered expandable metallic stents in 61 patients. Radiology 232:252–259
Heelan RT, Hilaris BS, Anderson LL et al (1987) Lung tumors: percutaneous implantation of I-125 sources with CT treatment planning. Radiology 164:735–740
Zhongmin W, Yu L, Fenju L et al (2010) Clinical efficacy of CT-guided iodine-125 seed implantation therapy in patients with advanced pancreatic cancer. Eur Radiol 20:1786–1791
Koutrouvelis PG (1998) Three-dimensional stereotactic posterior ischiorectal space computerized tomography guided brachytherapy of prostate cancer: a preliminary report. J Urol 159:142–145
Armstrong JG, Anderson LL, Harrison LB (1994) Treatment of liver metastases from colorectal cancer with radioactive implants. Cancer 73:1800–1804
Guo JH, Teng GJ, Zhu GY et al (2007) Self-expandable stent loaded with 125I seeds: feasibility and safety in a rabbit model. Eur J Radiol 61:356–361
Chen HH, Jia RF, Yu L et al (2008) Bystander effects induced by continuous low-dose rate 125I seeds potentiate the killing action of irradiation on human lung cancer cells in vitro. Int J Radiat Oncol Biol Phys 72:1560–1566
Costamagna G, Shah SK, Tringali A et al (2003) Prospective evaluation of a new self-expanding plastic stent for inoperable esophageal strictures. Surg Endosc 17:891–895
Mosca F, Consoil A, Stracqualursi A et al (2002) Our experience with the use of a plastic prosthesis and self-expanding stents in the palliative treatment of malignant neoplastic stenoses of the esophagus and cardia. Comparative analysis of results. Chir Ital 54:341–350
Sumiyoshi T, Gotoda T, Muro K et al (2003) Morbidity and mortality after self-expandable metallic stent placement in patients with progressive or recurrent esophageal cancer after chemoradiotherapy. Gastrointest Endosc 57:882–885
McGrath JP, Browne M, Riordan C et al (2001) Expandable metal stents in the palliation of malignant dysphagia and oesophageal-respiratory fistulae. Ir Med J 94:270–272
Sarper A, Oz N, Cihangir C et al (2003) The efficacy of self-expanding metal stents for palliation of malignant esophageal strictures and fistulas. Eur J Cardiothorac Surg 23:794–798
Bartelsman JF, Bruno MJ, Jensema AJ et al (2000) Palliation of patients with esophagogastric neoplasms by insertion of a covered expandable modified Gianturco-Z endoprosthesis: experiences in 153 patients. Gastrointest Endosc 51:134–138
Raben A, Mychalczak B, Brennan MF et al (1996) Feasibility study of the treatment of primary unresectable carcinoma of the pancreas with 103PD brachytherapy. Int J Radiat Oncol Biol Phys 35:351–356
Acknowledgments
Supported by grant from the National Scientific Foundation Committee of China (Grant No. 30870585/81071244) and from the Shanghai Luwan District Scientific Foundation (Grant No. LKW08001).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhongmin, W., Xunbo, H., Jun, C. et al. Intraluminal Radioactive Stent Compared with Covered Stent Alone for the Treatment of Malignant Esophageal Stricture. Cardiovasc Intervent Radiol 35, 351–358 (2012). https://doi.org/10.1007/s00270-011-0146-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0146-6