Abstract
Objective
The aim of this study was to evaluate the efficacy and safety of endovascular embolization of post-tonsillectomy pseudoaneurysm with the usage of monomeric n-butyl-2-cyanoacrylate (NBCA) glue as a first intention.
Methods
We retrospectively analyzed the technical details and clinical outcome of ten consecutive children presented with delayed post-tonsillectomy bleeding, caused by lingual or facial artery pseudoaneurysm, which was treated by endovascular embolization.
Results
Seven patients had lingual artery pseudoaneurysm, and three patients had injury of a common linguo-facial trunk. Eight patients were treated by endovascular embolization using NBCA glue, and two patients had to be embolized using microcoils. All patients were successfully embolized with no clinical complications. One patient suffered from bleeding during the interventional procedure that was controlled by NBCA which infiltrated normal branches with no clinical sequelae.
Conclusion
NBCA glue can be used as an effective appropriate embolizing material in endovascular embolization of post-tonsillectomy pseudoaneurysm. However, certain precautions are mandatory to avoid distal infiltration of normal arteries or proximal reflux that may endanger the internal carotid artery.
Level of Evidence
Level 4, case series.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Hemorrhage is the most common post-tonsillectomy complication, reported in about 3–4% of cases [1]. Early bleeding (within the first 24 h after surgery) is caused by operative technique or coagulopathy. Delayed post-tonsillectomy hemorrhage typically occurs from 5 to 10 days after surgery and is usually caused by a pseudoaneurysm, most commonly involving the lingual artery [1,2,3,4]. Less frequently, a common linguo-facial trunk pseudoaneurysm was reported. In a limited number of cases, facial artery involvement was reported [3,4,5,6,7]. The traditional ways of management are local maneuvers or surgical ligation of external carotid artery branches. The role of endovascular embolization in treatment of such cases is progressively increasing over the last years [2, 6]. Different embolic materials were described in the literature, including coils, ethylene vinyl alcohol (EVOH) copolymer and particles [1,2,3,4,5,6,7,8,9]. To the best of our knowledge, this is the first series of post-tonsillectomy pseudoaneurysm embolization with first intention to use n-butyl-2-cyanoacrylate (NBCA) glue.
Materials and Methods
The Institutional Review Board of our Radiology Department approved the design of the study and the use of clinical data. Written consent was obtained from the parents of all patients.
We performed a retrospective analysis of all patients referred from the “Ear–Nose–Throat” (ENT) Department to our Interventional Radiology Unit in our tertiary care University hospital, during the period from January 2009 to April 2018, for embolization of delayed post-tonsillectomy bleeding.
All patients were treated by endovascular embolization under general anesthesia. Right femoral puncture was performed in all cases introducing 4 French femoral sheaths and then using 4 French vertebral catheters to perform a diagnostic digital subtraction angiogram of both external and internal carotid arteries.
The presence of arterial pseudoaneurysm or contrast leakage was considered a sure evidence of the bleeding site. Otherwise, the presence of arterial mural irregularities at the side of recurrent bleeding described by the ENT surgeon was considered the site of arterial injury.
All patients were treated by superselective catheterization of the injured artery using Renegade (HI-FLO, Boston scientific, USA) microcatheter. Endovascular embolization was performed under road-map control, by injection of concentrated NBCA (histoacryl) glue (B. Braun, Tuttlingen, Germany) diluted with lipiodol (Guerbet, Aulnay-sous-Bois, France) in 2:1 ratio. The aim of the injection was to fill the segment of the parent artery harboring the pseudoaneurysm with glue and to avoid distal infiltration of normal branches or proximal reflux into the main stem of the external carotid artery (Fig. 1). In all cases, the volume of histoacryl/lipiodol mixture injected did not exceed 1 ml. The coils used were IDC-18 interlocking detachable coils (Boston Scientific, USA).
Large pseudoaneurysm involving the proximal segment of the facial artery, which is originating from a common linguo-facial trunk. A External carotid artery angiogram shows a post-tonsillectomy large pseudoaneurysm (black arrow), B selective angiogram shows the pseudoaneurysm (black arrow) arising from the proximal segment of the facial artery, which is originating from a linguo-facial trunk (white arrow), with filling of the lingual artery arising from the same linguo-facial trunk (double arrows), C superselective angiogram with the tip of microcatheter at the neck of the aneurysm, D cast of histoacryl glue filling the pseudoaneurysm (black arrow) with no distal infiltration of the facial artery branches and E right external carotid artery angiogram, showing total occlusion of the pseudoaneurysm
Results
Patients were seven males and three females with age ranging between 3 and 7 years old.
All patients, except one, were operated on in other hospitals and were referred to the ENT Department in our tertiary university hospital after recurrent attacks of delayed post-tonsillectomy bleeding. The bleeding started from 3 to 11 days after surgery. The number of bleeding episodes before presentation to our unit ranged from 2 to 6. We are reporting the results of ten patients referred consecutively to our Interventional Radiology Unit from the ENT Department for endovascular management. Until 2016, these cases were managed by either surgical or endovascular approach in our hospital. Starting from 2016, all cases of delayed post-tonsillectomy bleeding were routinely referred for endovascular management (Table 1).
The diagnostic angiogram performed revealed pseudoaneurysm involving the lingual artery in seven cases. In one case, the pseudoaneurysm of the proximal segment of the lingual artery was associated with occlusion of the facial artery 1 cm after its origin, likely related to surgical suturing during operation.
One patient had mural irregularities and narrowing of the proximal segment of the lingual artery arising from a common linguo-facial trunk.
Two patients had a pseudoaneurysm of a common linguo-facial trunk. One patient had a pseudoaneurysm arising from the proximal segment of the facial artery originating from a common linguo-facial trunk, while the other had a pseudoaneurysm at the bifurcation point of a common linguo-facial trunk with occlusion of the facial artery.
Eight patients were treated by endovascular embolization using concentrated NBCA (histoacryl) glue. Two patients had to be embolized using microcoils.
In nine cases, the procedure passed uneventfully. The pseudoaneurysm was totally occluded with occlusion of the whole injured segment of the artery. The injection of the histoacryl glue was well controlled. Therefore, no distal infiltration of the branches of the injured artery occurred. Microcoils—whenever used—were well deployed and resulted in occlusion of the whole injured segment of the artery.
One patient suffered from bleeding during the interventional procedure that was controlled. Superselective catheterization of the site of extravasations from the pseudoaneurysm was done. Rapid injection of concentrated histoacryl glue was performed. The histoacryl filled the pseudoaneurysm and occluded the parent artery. The bleeding stopped immediately. However, the histoacryl inadvertently infiltrated the proximal segment of the suprahyoid branch and a few dorsal lingual branches (Fig. 2). Nevertheless, the patient did not experience any complication in the 3 months follow-up period. This was explained by the rich collateral circulation at this area.
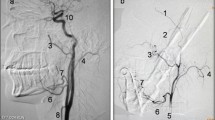
Linguo-facial trunk pseudoaneurysm. Severe bleeding occurred during the procedure, and rapid external compression by the ENT surgeon was performed until the pseudoaneurysm was embolized. A Left common carotid artery angiogram in lateral view, showing a post-tonsillectomy pseudoaneurysm (black arrow) considered to be at the bifurcation point of the common linguo-facial trunk, with non-filling of the facial artery, B left carotid artery angiogram in AP view, confirming the presence of post-tonsillectomy pseudoaneurysm (black arrow), C superselective angiogram shows extravasations of contrast medium from the pseudoaneurysm during the active bleeding (black arrow). The forceps used by the ENT surgeon for external compression to control bleeding is seen (white arrow), D non-subtracted image after injection of glue, showing the histoacryl occluding the pseudoaneurysm (black arrow). Some extravasations of the injected histoacryl glue occurred in the pharynx during injection (white arrows). It was seen by the ENT surgeon exerting external compression and was then cleaned up. Inadvertent distal infiltration of the lingual artery branches occurred (double arrows) and E selective angiogram of the left external carotid artery after embolization shows no more leakage from the pseudoaneurysm which is successfully occluded
All patients were discharged home 2–3 days after the interventional procedure with no further bleeding episodes. All patients were reviewed in the ENT outpatient clinic 1 month after discharge, except the patient with inadvertent histoacryl distal infiltration who was followed up for 3 months. In all cases, no further attacks of bleeding occurred after the endovascular embolization and no complications arose.
Discussion
Post-tonsillectomy pseudoaneurysm can be treated either by surgical ligation of suspected bleeding vessel or by endovascular embolization [2, 6].
Endovascular embolization has some advantages compared to surgical ligation. First, in the endovascular approach, diagnostic angiogram can be performed in the same session prior to therapeutic embolization, making sure of the bleeding vessel before its treatment. Second, it allows more selective occlusion of the injured artery compared to surgical ligation. In addition, it avoids the risk of injury of superior laryngeal or vagus nerves that can occur in the surgical approach [6].
Different embolic materials have been described for embolization of post-tonsillectomy pseudoaneurysm, trapping using microcoils, occlusion of parent artery using PVA (polyvinyl alcohol) particles, Gelfoam, detachable balloon or ethylene vinyl alcohol copolymer, e.g., Onyx (EV3, Irvine, CA, USA) [1,2,3,4,5,6,7,8,9].
Most cases reported in the literature have been treated by trapping using microcoils, as it appears as the safest technique [6, 8, 9]. However, liquid embolic material can be an alternative to occlude the pseudoaneurysm and its parent artery. Some advantages of the NBCA glue are assumed: The liquid embolic materials are considered to have more permanent occlusive effect, with no incidence of vessel recanalization, in contrast to delayed coil extrusion which may occur with microcoils [1]. Proximal occlusion of the injured artery using microcoils risks developing recurrent backdoor bleeding by retrograde filling of the injured artery from collateral pathways; therefore, trapping of the injured segment is needed [5, 6, 9]. In case of coil embolization, this necessitates passing the tip of the microcatheter distal to the pseudoaneurysm for trapping. This carries the risk of injuring the pseudoaneurysm during catheter navigation through it, and may even be technically impossible in some cases. The use of liquid embolic material allows injection from the tip of the microcatheter positioned proximal to the pseudoaneurysm, infiltrating the whole segment without the need of distal microcatheterization. NBCA glue is a cheaper embolizing material compared to microcoils, which is an important issue, especially in places with limited financial facilities.
The decision to use glue as a first embolizing material in our study was due to the presumed advantages it offered with regard to its relatively low cost, in addition to its availability in our unit. However, liquid embolic material carries a risk of inadvertent distal embolization in case of distal infiltration of the branches of the embolized artery [6]. Unilateral proximal occlusion of external carotid branches is usually without clinical complications, due to the rich collateralization [6]. Nevertheless, the infiltration of the distal end-artery branches may be of serious clinical consequences as with the lingual artery branches of the tip of the tongue [6]. The choice of dilution ratio and rate of injection is mandatory to avoid complication. We recommend using concentrated liquid embolic material [10]. One of the useful technical tips is to wedge the tip of the guiding catheter into the lingual artery before injection of the NBCA through the microcatheter. This may stop the incoming flow, which will allow better control of the NBCA glue during its injection and prevents its distal infiltration. This may also help in preventing the possible proximal reflux of the injected NBCA glue into the main stem of the external carotid artery or even into the internal carotid artery which may have catastrophic sequelae. In the case of use of liquid embolic material a possible advantage of histoacryl glue (NBCA) over Onyx, is that it has faster rate of polymerization, so distal infiltration of the normal vessels is more unlikely to occur with it [10].
In the case who bled actively during the procedure, hurried injection of the NBCA glue without road-map control caused inadvertent distal infiltration of normal branches.
In the two cases embolized by microcoils, injection of histoacryl was considered unsafe as the tip of the microcatheter was positioned very proximal to the main stem of the external carotid artery and the risk of proximal reflux was a justification to use microcoils instead of histoacryl (Fig. 3).
Injury of the proximal segment of the lingual artery, which is originating from a common linguo-facial trunk in a patient with post-tonsillectomy bleeding, treated by coiling. A External carotid artery angiogram shows wall irregularity and narrowing involving the proximal segment of the lingual artery (white arrow), which is originating from a common linguo-facial trunk. This was considered the site of vascular injury and the source of bleeding, B common carotid angiogram shows total occlusion of the site of vascular injury and the whole linguo-facial trunk from its origin (white arrow). Collaterals (double black arrows) from the internal maxillary artery are seen filling the facial artery in a retrograde manner (black arrow), C superselective angiogram of the internal maxillary artery, showing the collaterals (double black arrows) from the internal maxillary artery filling the facial artery in a retrograde manner (black arrow). Coils occluding the linguo-facial trunk are seen (white arrow) and D, E AP angiography of contralateral right common carotid artery showing collaterals from the right lingual artery filling the left lingual artery (white arrow) with the coils occluding the common linguo-facial trunk on the left side (black arrow)
The limitations of our study included the relatively small number of patients, the retrospective type of the study and the lack of sizeable comparative control group using another embolic material.
Conclusion
NBCA glue can be used as an effective and safe embolizing material in endovascular embolization of most cases of post-tonsillectomy pseudoaneurysm. However, certain precautions during its injection are mandatory to avoid possible complications that may be induced by distal embolization or proximal reflux.
References
Gratacap M, Couloigner V, Boulouis G, et al. Embolization in the management of recurrent secondary post-tonsillectomy haemorrhage in children. Eur Radiol. 2015;25(1):239–45. https://doi.org/10.1007/s00330-014-3387-3.
Kleinso GHD, de Sousa AM, Botelho LF, et al. Endovascular treatment of delayed bleeding after tonsillectomy. J Vasc Bras. 2015;14(4):356–9. https://doi.org/10.1590/1677-5449.07514.
Van Cruijsen N, Gravendeel J, Dikkers FG. Severe delayed posttonsillectomy haemorrhage due to a pseudoaneurysm of the lingual artery. Eur Arch Otorhinolaryngol. 2008;265:115–7. https://doi.org/10.1007/s00405-007-0391-0.
Juszkat R, Korytowska A, Lukomska Z, et al. Facial artery pseudoaneurysm and severe bleeding after tonsillectomy-endovascular treatment with PVA particle embolization. Pol J Radiol. 2010;75(1):88–91.
Choi KJ, Cheng T, Cobb MI, et al. Recurrent post-tonsillectomy bleeding due to an iatrogenic facial artery pseudoaneurysm. Acta Oto Laryngol Case Rep. 2017;2(1):103–6. https://doi.org/10.1080/23772484.2017.1330122.
Manzato L, Trivelato FP, Alvarenga AYH, et al. Endovascular treatment of a linguo-facial trunk pseudoaneurysm after tonsillectomy. Braz J Otorhinolaryngol. 2013;79(4):524. https://doi.org/10.5935/1808-8694.20130094.
Baik FM, Chang AA, Green DA, et al. Post-tonsillectomy lingual artery pseudoaneurysm. Laryngoscope. 2011;121(54):S61. https://doi.org/10.1002/lary.21931.
Hsu WC, Lim KE, Hsu YY. Emergency endovascular balloon embolization of an active oral bleeder-a case report. Tzu Chi Med J. 2006;18:221–4.
Opatowsky MJ, Browne JD, McGuirt WF Jr, et al. Endovascular treatment of hemorrhage after tonsillectomy in children. AJNR Am J Neuroradiol. 2001;22:713–6.
Rifai M, Younes A, Hassan F. Recurrent post tonsillectomy hemorrhage: an alarming complication. Otolaryngol Open Access J. 2016;1(2):00111. https://doi.org/10.23880/OOAJ-16000111.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of our Radiology Department approved the design of the study and the use of clinical data.
Informed Consent
Informed consent was obtained from the parents of all individual participants included in the study.
Consent for Publication
For this type of study, consent for publication is not required.
Rights and permissions
About this article
Cite this article
Hassan, F., Younes, A. & Rifai, M. Endovascular Embolization of Post-tonsillectomy Pseudoaneurysm: A Single-Center Case Series. Cardiovasc Intervent Radiol 42, 528–533 (2019). https://doi.org/10.1007/s00270-018-2131-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2131-9