Abstract
Purpose
To analyze the safety, efficacy and outcome of angio-embolization in the management of refractory oro-nasal bleeding in patients of severe maxillofacial trauma.
Materials and Methods
It was a retrospective analysis of 21 patients who were managed by angio-embolisation to control refractory oro-nasal bleeding in severe maxillofacial trauma from December 2010 to December 2013. The patient population included 19 males and 2 females and the age ranged from 16 to 55 years (mean age of 29.6 years). Gelfoam pledgets and coils were used as embolising agents in branches of external carotid arteries. Embolising coils were preferably used to block actively bleeding vessels on angiography.
Results
Road traffic accidents were the etiology in 17 patients and fall from height (two), assault (one) and gunshot injury (one) in the rest. Twelve (52 %) patients showed active contrast extravasation on angiography. Active arterial bleeding was observed from branches of internal maxillary [11], facial [2] and lingual arteries [4]. Gel foam embolisation alone was done in 16 patients, coil embolisation alone in two patients and both coil and gel foam embolisation in three patients. The procedures were technically successful in twenty (95 %) patients. None of the patients had procedure related complications. Nine patients (42 %) succumbed to their associated injuries later, in which five patients had severe head injuries and four patients had history of hemorrhagic shock and cardiac arrest prior to the procedure.
Conclusion
Angio-embolisation is a safe and effective technique in managing intractable bleeding in maxillofacial injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maxillofacial injuries are unusual causes of life threatening haemorrhage in the setting of accidental trauma [1, 2]. The primary methods to control traumatic oro-nasal bleeding include application of pressure, nasal packing, correction of coagulopathy and surgical ligation of bleeding vessels. These measures are often ineffective when there is active bleeding from major vessels. Surgical approach also will be difficult in patients with profuse bleeding. Ligation of external carotid arteries (ECAs) to achieve control of bleeding is non-selective and is associated with high morbidity. Selective angiography and embolisation of bleeding vessels is highly accurate and effective to achieve hemostasis in uncontrollable bleeding. In this retrospective study, we intend to analyze the safety, technical success and clinical outcome of patients treated with angioembolisation for traumatic maxillofacial bleeding.
Materials and Methods
It was a retrospective analysis of 21 patients who were managed by angio-embolisation to control refractory oro-nasal bleeding in severe maxillofacial trauma from December 2010 to 2013. The patient population included 19 males and 2 females and the age ranged from 16 to 55 years (mean age of 29.6 years). The clinical records of the patients were reviewed to analyze the preprocedure condition of the patients in terms of hemodynamic status, Glasgow Coma scale (GCS), amount of blood loss and associated injuries. The interval from the time of injury to the time of procedure was assessed. Available imaging data was also analyzed for associated injuries.
Indication for Angioembolisation
All these patients were initially managed by application of pressure, nasal packing with Foley catheters and blood transfusion. All these patients continued to bleed inspite of above measures, hence taken for angioembolisation.
Angiographic Technique
Angiography was performed commonly by right transfemoral approach. After obtaining arterial access the carotid arteries were cannulated using 4F diagnostic catheter (VERT slip-cathBeacon Tip Catheter; Cook, Bloomington, IN, USA) and selective angiograms of common carotid arteries (CCAs), internal carotid arteries (ICAs) and ECAs were obtained (Fig. 1). If the bleeding was from a single nostril or if it was predominantly from one side, the ipsilateral arteries were interrogated first. Initially, angiographic studies of ICAs were done to rule out an ICA source of bleed, to verify supply of ophthalmic artery (choroidal blush) and to rule out communication between branches of ICA and ECAs (Fig. 2). In such cases surgery is preferred over embolisation due to higher risk of complications from accidental non-target embolisation. Selective angiographic studies of ECAs were done to look for source of bleed and to rule out potentially dangerous collaterals (Fig. 1). Superselective cannulation of ECA branches was done using hydrophilic microcatheters (Progreat 2.7 F microcatheter, Terumo; Terumo Corporation, Tokyo, Japan) in selective cases with active bleeding in distal branches or with tortuous anatomy of parent vessel.
Lateral angiogram of common carotid (a) and external carotid arteries (b) show major branches; 1 superficial temporal artery (STA), 2 middle meningeal artery, 3 internal maxillary artery (IMA), 4 posterior auricular artery, 5 external carotid artery, 6 lingual artery, 7 facial artery, 8 superior thyroid artery, 9 common carotid artery, 10 internal carotid artery
Gelfoam pledgets (Gelfoam; Pfizer, NewYork, NY) and fibered coils were used as embolising agents. Gel foam was the most commonly used agent. In cases in which angiographic study did not reveal active contrast leak, the internal maxillary arteries (IMAs) of both sides were empirically embolised using gelfoam particles. To avoid non-target embolisation the catheter tip was placed distal to the meningeal and deep temporal branches. Facial, lingual and superficial temporal arteries (STAs) were also embolized in case of evident contrast leak. Coils were preferably used in cases of active contrast leaks.
Definition of Results
Technical success was defined as successful embolisation of either all bleeding vessels of external carotid arteries or empirical embolisation of bilateral IMAs in case of bleeding not seen on angiography.
Technical failure is defined as failure to embolise one or more bleeding vessels from ECAs or failure to embolise one or both internal maxillary arteries empirically.
Clinical success was defined as control of oro-nasal bleed after the successful embolisation.
Clinical failure is defined as failure to achieve hemostasis even after successful embolisation.
Results
A total of 21 patients were managed by angio-embolisation to control refractory oro-nasal bleeding in severe maxillofacial trauma. Majority of the cases were road traffic accidents (Table 1). Twelve patients had significant bleeding before reaching the hospital and were hemodynamically unstable. Majority of patients had poor neurological status at admission (Table 2) with an average of GCS score of 7.8.
Angiography findings: Active contrast extravasation was observed in twelve (52 %) patients on angiography. Active arterial bleeding was observed from branches of internal maxillary, facial and lingual arteries (Table 3; Figs. 3, 4). In rest of nine patients we could not see any extravasation of contrast on angiography.
Embolisation
Majority of the patients were managed with gelfoam embolisation (Figs. 5, 6, 7; Table 4). Coils were used in selective cases of active contrast leak (Fig. 8). Internal maxillary artery was the most common culprit vessel to be targeted (Table 5).
Outcome
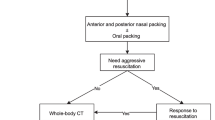
The procedures were technically successful in twenty (95 %) patients. One patient had cardiac arrest in intervention theatre and hence the procedure could not be completed. None of the patients had procedure related complications. Nine patients (42 %) succumbed to their associated injuries later, in which five patients had severe head injuries and four patients had history of hemorrhagic shock and cardiac arrest prior to the procedure (Fig. 9).
Two out of the nine patients who were hemodynamically stable at admission died because of severe head injury. These two patients had an average GCS of 4.5. Seven out of 12 patients who were hemodynamically unstable died because of repeated cardiac arrests despite resuscitation due to marked blood loss prior to admission (four) and severe head injury (three).
Among the 11 patients with poor neurological status (GCS < 7) at presentation, nine patients died (severe head injury in five and hemorrhagic shock in four patients). All the patients (ten) with a GCS of seven or above at admission had clinical success.
Complications
Two patients had local soft tissue swelling post embolisation, which got resolved with conservative measures. No major procedure related complications were encountered in our study group.
Discussion
Angioembolisation has been an accepted technique in the management of refractory epistaxis [3, 4]. It is especially sought in cases of posterior epistaxis, which fails to respond to nasal packing and medical measures. Maxillofacial trauma is a common cause for posterior epistaxis. Trauma can also result in refractory oral bleeding, which along with associated injuries can lead to airway compromise. Although life threatening hemorrhage is considered rare in maxillofacial injuries, exsanguinating bleeding can occur from rupture of branches of carotid arteries [5]. Blunt maxillofacial trauma is the most common mechanism of injury leading to torrential oro-nasal bleeding [2]. Blunt trauma from road traffic accidents was the most common etiology in our series.
The primary concern in maxillofacial injury is patency of airway. Airway can be compromised by bleeding into oral cavity, facial fractures and soft tissue edema. After securing the airway the next priority is to arrest bleeding. Various methods for treating bleeding from maxillofacial trauma include nasal packing, reduction of fracture, arterial ligation, angiography and selective embolisation. Nasal packing is done with gauze, foley catheter or triple-lumen balloon catheter with a reported success rate of 48–83 % in posterior nasal bleeding [6–8]. Temporary reduction of fractures can stop bleeding from intraosseous vessels. The next step in intractable bleeding is surgical ligation of external carotid artery, IMA branches or rarely ethmoidal arteries. Surgical arterial ligation is often not effective because of involvement of multiple vessels and rich collateral network in the region. Fracture fixation and surgical arterial ligation are not often technically feasible in complex facial injuries with incessant bleeding.
Angioembolisation was introduced as a novel technique, alternate to surgery to treat uncontrollable bleeding by Sokoloff et al. [9] in 1974. For controlling idiopathic intractable epistaxis, angioembolisation is reported to have a success rate of 75–97 % [7, 10]. Endovascular techniques have an added advantage in complex maxillofacial injuries where other modalities face technical difficulties [4, 11].
The most commonly observed culprit artery in traumatic maxillofacial bleeding was IMA followed by facial and lingual arteries. IMA and its branches are reported to be responsible for approximately 70 % cases of uncontrolled bleeding. Thus the empirical embolisation of terminal branches of IMA is justified even if active contrast extravasation is not evident on angiography. Bleeding can also be from ethmoid branches of ophthalmic artery and directly from ICA into the sphenoid sinus. In such cases involving ICA or its branches, surgery is preferred to avoid the potential neurological complications during embolisation.
Embolising agents used to treat traumatic oro-nasal bleeding includes pledgets of gelatin sponge and stainless steel or platinum coils [3, 12]. Gel foam particles are the most commonly used embolising agents. In our series 16 (76 %) patients were treated by gelfoam alone. Communicating channels between the branches of ECA and ICA in the embolising field has to be carefully ruled out before particle embolisation. Embolising coils can be safely used when such communications are evident on diagnostic angiography. Coils are also preferred in case of active contrast extravasation seen on angiography. Superselective catheterization of bleeding branches is necessary for coil deployment. Coil was used in cases where active bleeding seen on angiography and that site can be reached selectively by microcatheter. Whereas, gelfoam was used in cases where we could not selectively reach the site of active bleed or in cases where there was diffuse blush seen on angiography due to small distal vessel ooze. In few cases, gelfoam embolisation was done prophylactically to reduce the perfusion pressure to take care of venous bleeds. Combination of coil and gelfoam was done in three patients, as sandwich technique to reinforce the embolisation and achieve immediate hemostasis.
Angioembolisation is reported to have a high technical and clinical success in dealing intractable epistaxis. Our patients showed good technical and clinical success comparable to previous studies. However the clinical outcome in these high velocity trauma patients with severe maxillofacial injuries depended on associated injuries.
The most important prognostic factors include degree of blood loss, hemodynamic and neurologic status at admission. In our series, despite procedural success, nine patients died due to severe head injury and pre-procedural blood loss. GCS score at presentation is seen to have a direct correlation with outcome. All those who had a good GCS score at presentation had good clinical outcome.
The potential complications reported in literature are because of non-target embolisation and local ischemic changes. They include cerebrovascular accidents, blindness, lip-tongue necrosis, facial nerve palsy and trismus [12]. No major procedure related complications were observed in our series.
To conclude, angio-embolisation is an effective technique in managing intractable bleeding in maxillofacial injuries. The procedure is safe so long as appropriate care is taken to ensure delivery of embolic agent into target vessels and avoid delivery into intracranial branches and dangerous collaterals.
References
Ardekian L, Samet N, Shoshani Y, Taicher S (1993) Life-threatening bleeding following maxillofacial trauma. J Cranio-Maxillo fac Surg 21(8):336–338
Bynoe RP, Kerwin AJ, Parker HH 3rd, Nottingham JM, Bell RM, Yost MJ et al (2003) Maxillofacial injuries and life-threatening hemorrhage: treatment with transcatheter arterial embolization. J Trauma 55(1):74–79
Willems PWA, Farb RI, Agid R (2009) Endovascular treatment of epistaxis. AJNR Am J Neuroradiol 30(9):1637–1645
Kurata A, Kitahara T, Miyasaka Y, Ohwada T, Yada K, Kan S (1993) Superselective embolization for severe traumatic epistaxis caused by fracture of the skull base. AJNR Am J Neuroradiol 14(2):343–345
Sakamoto T, Yagi K, Hiraide A, Takasu A, Kinoshita Y, Iwai A et al (1988) Transcatheter embolization in the treatment of massive bleeding due to maxillofacial injury. J Trauma 28(6):840–843
Pollice PA, Yoder MG (1997) Epistaxis: a retrospective review of hospitalized patients. Otolaryngol-Head Neck Surg 117(1):49–53
Klotz DA, Winkle MR, Richmon J, Hengerer AS (2002) Surgical management of posterior epistaxis: a changing paradigm. The Laryngoscope 112(9):1577–1582
Schaitkin B, Strauss M, Houck JR (1987) Epistaxis: medical versus surgical therapy: a comparison of efficacy, complications, and economic considerations. The Laryngoscope 97(12):1392–1396
Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberger LE (1974) Therapeutic percutaneous embolization in intractable epistaxis. Radiology 111(2):285–287
Vitek J (1991) Idiopathic intractable epistaxis: endovascular therapy. Radiology 181(1):113–116
Dimitroulis G, Steidler N (1992) Massive bleeding following maxillofacial trauma. Case report. Aust Dent J 37(3):185–188
Liu WH, Chen YH, Hsieh CT, Lin EY, Chung TT, Ju DT (2008) Transarterial embolization in the management of life-threatening hemorrhage after maxillofacial trauma: a case report and review of literature. Am J Emerg Med 26(4):516e3–516e5
Conflict of interest
No conflict of interest from any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gamanagatti, S., Prasad, T.V., Kumar, A. et al. Angioembolisation in Maxillofacial Trauma: An Initial Experience in a Tertiary Care Center. J. Maxillofac. Oral Surg. 15, 59–66 (2016). https://doi.org/10.1007/s12663-015-0792-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-015-0792-3