Abstract
Purpose
To evaluate the feasibility of helical iodine-125 (I-125) seed portal vein implantation.
Materials and Methods
Helical I-125 seed implants were placed into the portal vein of healthy pigs through the transjugular (n = 3) or percutaneous transhepatic (n = 3) route. Six pigs received follow-up at 9 weeks after implantation. Blood tests were performed preimplantation, and at 1 and 9 weeks after implantation. Contrast-enhanced computed tomography (CT) and single-photon emission computed tomography combined with CT (SPECT-CT) were acquired after implantation. Post-implantation CT was imported to the treatment planning system (TPS) for dose verification. At 9 weeks after implantation, another CT was performed before histopathological examination.
Results
All implantations were successful, and the helical implants were fixed to the portal vein. CT showed no implant migration or portal vein thrombosis. The average dose to 90% of the target volume calculated from TPS was 68.4 Gy. SPECT-CT revealed an irregular isodose around the implant, in which the hottest spot was near the central portal vein lumen. All pigs were in good condition at the 9-week follow-up. Histopathology studies confirmed no portal vein thrombosis. Pigs showed no signs of bleeding, necrosis, or perforation of the peripheral tissue or organs. Intimal hyperplasia was observed at the two ends of the implant. A mild inflammatory response was detected in the bile duct and adjacent liver tissues, yet there was no apparent inflammation of the hepatic arteries.
Conclusion
The helical I-125 seed implants can be inserted into the portal veins of healthy pigs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies around the world with the sixth highest incidence rate and second highest mortality rate among all cancers [1]. Approximately, 10–40% of HCC patients present with portal vein tumor thrombus (PVTT) at the time of diagnosis, which is an independent predictor of a poor prognosis and decreased overall survival [2,3,4]. Oral sorafenib is the only recommended treatment for HCC with PVTT, yet the drug displays limited efficacy with an increase in the median overall survival [5, 6]. Numerous transarterial chemoembolization (TACE)-based combination therapy techniques have been suggested and achieved better prognosis [7,8,9,10,11,12,13]. In particular, iodine-125 (I-125) seed brachytherapy has shown promising results when combined with TACE therapy for treating HCC patients with PVTT [10,11,12,13]. The effectiveness and safety of the I-125 seed strands combined with stents alone or stents loaded with I-125 seed and TACE have been demonstrated in HCC patients with main portal vein tumor thrombus (MPVTT) [11, 12]. However, both techniques required placement of a stent to compress the seed strand or to carry the seed to achieve brachytherapy of MPVTT, which significantly introduced trauma and increased the difficulty and overall risk of implantation.
Our team developed the helical I-125 seed implant with the aim to fix the implant in the portal vein for endovascular brachytherapy, while minimizing potential liver injury and decreasing the overall risk of stent implantation. In this study, we evaluated the feasibility of helical I-125 seed portal vein implantation.
Materials and Methods
Animals
This study was approved by the Animal Ethics Committee of XXX University in China. The Experimental Animal Center of Soochow University (Suzhou, China) provided six pigs that were single-housed. Food intake was monitored, and the animals were housed according to the standard procedures.
Helical I-125 Seed Implant Preparation
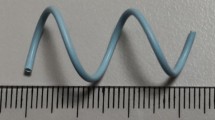
I-125 seeds were obtained from Seeds Biological Pharmacy Ltd. (Model 6711, Tianjin, China) with a diameter of 0.8 mm, length of 4.5 mm, 0.5 mCi (18.5 MBq) activity, and half-life of 59.6 days. The seeds release 35.5 keV γ ray, 27.4 and 31.4 keV X-ray with an effective half value layer of tissue, which is the thickness of tissue required to attenuate the intensity by half, of 17 mm. The helical implant consisted of 18 I-125 seeds that were continuously inserted into the helical sleeve (Fig. 1). The helical sleeve (diameter and pitch of 12 mm) was constructed using a 4F angiocatheter (Patent No. 201621449026.5, Zhejiang Barty Medical Technology Co., Ltd, Hangzhou, China), with the ends being sealed by heat. After completing the construction of the implant, the diameter was 20 mm and the pitch was 23 mm. The I-125 seeds were continuously inserted into the helical sleeve, in which the inner diameter of the sleeve was the same as the seed diameter. Thus, the seeds were aligned in a helical geometry similar to the sleeve.
Implantation Procedures
The pigs were fasted for 12 h and water deprived 6 h before surgery. Sodium pentobarbital (3%) was injected via the ear vein for anesthesia. A catheter sheath was introduced through the transjugular (n = 3) or percutaneous transhepatic (n = 3) route into the portal vein for seed implantation. For the transjugular route, the right internal jugular vein was punctured and the guide wire was sent to the inferior vena cava followed by the RUPS-100 puncture set (Cook, Inc., Bloomington, IN, USA) through the left or right branch of the portal vein from the beginning of the right hepatic vein. The guide wire and RUPS-100 outer sheath tube were sent to the main portal vein. For the percutaneous transhepatic puncture, the left or right portal vein secondary branch was punctured by a 22-gauge Chiba needle (Cook, Inc.) and a guide wire was introduced followed by a 4F catheter sheath with a length of 55 cm (Cook, Inc.) to the main portal vein with ultrasound guidance. After the catheter sheath was sent to the main trunk of the portal vein, the tip end of the catheter would pass the portal vein. The helical implant was inserted into the sheath and was pushed to the target area. The catheter sheath was withdrawn to release the helical implant. Upon release, the implant reshaped itself into the helical structure at the target site for permanent fixture to the portal vein. After implantation, the helical implant will be shaped relative to the portal vein with a diameter of 14 mm. Therefore, the diameter of the helical implant changed from 20 to 14 mm, while the pitch changed from 20 to 30 mm. The pitch of the helical implant can be formulated as p1 = √[(p2) + (πd)2 − (πd1)2], where p1 is the pitch after implantation, d1 is the diameter of main portal vein, p is the pitch before implantation (23 mm), and d is the diameter of the helical implant before implantation (20 mm).
Monitoring and Examination After Implantation
All animals received follow-up at 9 weeks after implantation, which is equivalent to the half-life of I-125 (59.6 days). Animals were monitored for the loss of appetite, vomiting, diarrhea, and weight loss after implantation.
Blood tests were performed before implantation and at 1 and 9 weeks after implantation to assess liver function and blood toxicity. Contrast-enhanced computed tomography (CT) and single-photon emission computed tomography (SPECT) combined with CT (SPECT-CT) were performed directly after the implantation procedure. For SPECT, the images were acquired with 1 × 105 counts on a 128 × 128 matrix. The energy peak for the camera was set to 37 keV, and the energy window was set to peak energy ± 30%, that is, 26–48 keV. Three-dimensional (3D) reconstructions of the CT scans showed the positioning of the helical implant, while SPECT-CT was used to measure the dose distribution of the implant [11]. A second CT scan was performed at 9 weeks post-implantation.
Animals were killed for pathological examination at 9 weeks post-implantation. The morphology of the portal vein wall, thrombosis in the portal vein, damage to the bile duct, hepatic artery, and adjacent liver tissue, as well as the shape and position of the helical implant, were assessed.
Postoperative Dose Verification
Postoperative abdominal-enhanced CT imaging of the portal vein (5 mm slice thickness) was imported to a 3D radiation treatment planning system (FtzyPlan 1.3.118, Beijing FTT Technology Ltd. Co., China). The I-125 seed was simplified to a point source for dose verification of the target area for simplicity. The portal vein and organs-at-risk (OARs, bile duct, hepatic artery, and the adjacent liver tissue) were delineated using the software. After verifying the prescription dose (100 Gy), the position, number of seeds (18), and activity of the seeds (0.5 mCi/seed), dose volume histogram (DVH) and dose distribution were computed. Since the bile duct and hepatic artery were difficult to accurately delineate in the CT images, a 5 mm annular radius extending from the portal vein wall was defined as the OARs (bile duct and hepatic artery). Adjacent liver tissue was defined as 17 mm from the portal vein, in which 17 mm was the equivalent tissue half value layer of I-125 seed.
Statistical Analysis
SPSS 19.0 (IBM, Chicago, IL, USA) was used to analyze the data in this study. The one-way analysis of variance (ANOVA) was used to compare the differences in hematological indices among the different time points. Measurement data were presented as mean ± standard deviation. P values of less than 0.05 were concerned statistically significant.
Results
Implantation and Postoperative Condition
The helical implants were successfully fixed to the portal vein (Fig. 2). There were no surgical complications, which may have included abdominal bleeding, acute portal vein thrombosis, or death. There was no loss of appetite, vomiting, diarrhea, or weight loss in the surgical animals. Hematological indices throughout the examination period were summarized, in which no significant differences were detected (Table 1). Abdominal CT scans after the procedure and 9 weeks post-implantation showed no implant displacement or signs of implant damage or portal vein thrombosis (Fig. 3). Postoperative abdominal SPECT-CT revealed an irregular isodose around the implant, in which the hottest spot was near the central portal vein lumen (Fig. 4).
Postoperative Dose Verification
The average of dose to 90% of the volume (D90) of the portal vein, bile duct and hepatic artery, as well as 17 mm adjacent liver tissue were 68.4 ± 3.3 Gy, 31.5 ± 3.6 Gy and 14.8 ± 2.1 Gy, respectively. The corresponding DVH is shown in Fig. 5. The isodose distribution and surface rendering of the dose is shown in Figs. 6 and 7.
Pathological Findings
Pathological examination showed no thrombus formation in the portal vein. A thin layer of proliferative intima at the two ends of helical implant was observed in all animals. Partially due to the larger portal vein lumen, the proliferative endothelium had no significant influence on the blood flow. There were no apparent hemorrhaging, necrosis, or perforations in the surrounding tissues or organs. Under light microscope, fibrous tissue hyperplasia was observed at both ends of the helical implant in all animals. A mild inflammatory response was observed in the bile duct and adjacent (17 mm) liver tissue, yet there was no apparent inflammation at the hepatic arteries (Fig. 8).
Peripheral changes in the portal vein and surrounding organs under light microscopy (Mag. ×40). A Apparent fibrous tissue proliferation (arrow) in the portal vein. B A mild inflammatory response of bile duct and focal epithelial shedding (arrow). C No obvious inflammatory reaction in hepatic artery (arrow). D) Hepatocellular mild edema of hepatic tissue (arrow) 17 mm adjacent to the portal vein
Discussion
A helical I-125 seed implant was developed to assess its feasibility in the portal vein of healthy pigs. Due to the helical geometry, the implant can self-attach to the portal vein without displacement. When the implant was loaded with I-125 seed, it delivered a therapeutic dose without causing apparent radiological toxicities.
Huang et al. [10] showed that TACE, when combined with direct implantation of seeds into the tumor thrombosis, significantly prolonged the survival of PVTT patients. However, the efficacy in treating MPVTT was limited. This was primarily due to the direct seed implantation into the tumor thrombus, which was only suitable for the branching tumor thrombus. Since the main portal vein was not surrounded by liver parenchyma, percutaneous transhepatic direct puncture of MPVTT could cause abdominal hemorrhaging. Thus, this technique cannot be applied in brachytherapy of MPVTT. However, brachytherapy of MPVTT can be achieved by the placement of seed strands combined with stents alone or stents loaded with seed into the main portal vein through a percutaneous puncture branching portal vein approach. These two techniques not only effectively inhibit MPVTT, but also open the main portal vein and restore the blood flow to the left or right lobes [11, 12]. Previously, Luo et al. showed that the effectiveness of seed strands combined with stent placement in treating severely obstructed main portal vein was lower when compared to partial main portal vein obstruction [14]. Yang et al. believed that, for severely obstructed main portal vein patients, seed strand placement alone should be considered to minimize implantation failure rates, potential complications, and economic burden caused by the stent. In 2014, the same group confirmed the feasibility and safety of seed strand placement alone for the treatment of MPVTT, and combined TACE treatment can lead to survival benefits when compared with TACE alone. Although the seed strand can be fixed next to the tumor thrombus, it may displace when the main portal vein was recanalized due to its compression against the wall in severely obstructed main portal vein patients [15]. More importantly, for partially obstructed main portal vein, seed strand alone cannot be fixed in the portal vein, but rather rely on the stent to be fixed next to the tumor thrombus.
The current study indicated that the helical I-125 seed implant can be self-fixed in the portal vein for endovascular brachytherapy without stent compression. Compared with seed strand combined with stent or stent loaded with seeds, the helical I-125 seed implant required only a 4F catheter sheath, whereas the former requires a 10–12F catheter sheath. Thus, the helical system greatly reduced the trauma and the risk of implantation. Seed strands combined with stents alone or stents loaded with seed placement were complicated, while helical implant placement was relatively simple. Nevertheless, the current study was only an animal experiment. Whether the helical implant can achieve the intended purpose for HCC patients with MPVTT remains to be elucidated by clinical trials. Upon deployment, the sleeve of the helical implant was shaped by a 4F catheter. Since the helical implant was fixed in the portal vein without a metal stent, the obstructed main portal vein cannot be opened.
Seed strands implantation gave dose distribution centered on the implant, whereas stents loaded with I-125 seeds formed dose distributions centered on the lumen of the portal vein [11,12,13,14,15,16]. The isodose of the helical implant in this study was irregular, in which the hottest spot was near the central portal vein lumen. A good dose distribution for all of these brachytherapy modes in the lumen was harder to achieve as compared to solid tumors according to the TPS plan, which was due to the fact that radioactive source was only to be placed in the lumen. However, the effectiveness of brachytherapy in the lumen (including blood vessels, biliary tract, and esophagus) has been confirmed by other studies [11,12,13,14,15,16,17,18]. The purpose of brachytherapy in the lumen and brachytherapy in solid tumors was different. In particular, I-125 seed brachytherapy in solid tumors aimed to kill tumors to the greatest extent, whereas the purpose of brachytherapy in the lumen was to effectively inhibit tumor invasion of the lumen. In clinical applications, 0.7 mCi (25.9 MBq) of I-125 provides a safe dosimetric dose [11,12,13,14,15]. In this study, taking into account that more I-125 seeds were used in the helix system, the 0.5 mCi (18.5 MBq) I-125 seed was used to produce an average D90 in the portal vein of 68.4 Gy. While the D90 was lower than the prescribed dose in this study (100 Gy), current helical implants still provided higher D90 to the target as compared with other preclinical studies using single seed strand implants (0.7 mCi; D90 32.2 Gy) [19]. Meanwhile, damage to the surrounding tissues and organs was within acceptable limits. Yao et al. simulated the dose distribution of seed strands combined with stent and showed the optimal seed activity and number to give a prescribed dose greater than 105 Gy [19]. However, the dose to the surrounding tissues and organs was not investigated, especially the bile duct.
In this study, the two ends of the helical implant were covered by a thin layer of proliferative intima, which may be related to the mechanical stimulation of the portal vein endothelium. Partially due to the relatively larger portal vein lumen, the proliferative endothelium had no significant influence on the blood flow. There were no apparent signs of radiological toxicity up to 9 weeks after implantation. The pigs maintained a viable state without portal vein thrombosis, without signs of bleeding, necrosis, or the perforation of surrounding tissues and organs. However, due to limited sample size, the safety of the helical I-125 seed portal vein implantation may require further verification. The situation for helical implant placement in HCC patients with MPVTT may deviate from current animal study. Nevertheless, the current study demonstrated the helical I-125 seed implants can be inserted into the portal veins of healthy pigs.
Abbreviations
- I-125:
-
Iodine-125
- CT:
-
Contrast-enhanced computed tomography
- SPECT:
-
Single-photon emission computed tomography
- TPS:
-
Treatment planning system
- D90:
-
Dose to 90% of the target volume
- HCC:
-
Hepatocellular carcinoma
- PVTT:
-
Portal vein tumor thrombus
- MPVTT:
-
Main portal vein tumor thrombus
- TACE:
-
Transarterial chemoembolization
- EBRT:
-
External beam radiotherapy
- 3D:
-
Three-dimensional
- OAR:
-
Organs-at-risk
- DVH:
-
Dose volume histogram
- ANOVA:
-
Analysis of variance
- PTV:
-
Planning target volume
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. https://doi.org/10.3322/caac.21262.
Minagawa M, Makuuchi M. Treatment of hepatocellular carcinoma accompanied by portal vein tumor thrombus. World J Gastroenterol. 2006;12(47):7561–7.
Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology (Baltimore, Md). 1999;29(1):62–7. https://doi.org/10.1002/hep.510290145.
Villa E, Moles A, Ferretti I, Buttafoco P, Grottola A, Del Buono M, et al. Natural history of inoperable hepatocellular carcinoma: estrogen receptors’ status in the tumor is the strongest prognostic factor for survival. Hepatology (Baltimore, Md). 2000;32(2):233–8. https://doi.org/10.1053/jhep.2000.9603.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. The New England journal of medicine. 2008;359(4):378–90. https://doi.org/10.1056/NEJMoa0708857.
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34. https://doi.org/10.1016/s1470-2045(08)70285-7.
Geschwind JF, Kudo M, Marrero JA, Venook AP, Chen XP, Bronowicki JP, et al. TACE Treatment in Patients with Sorafenib-treated Unresectable Hepatocellular Carcinoma in Clinical Practice: Final Analysis of GIDEON. Radiology. 2016;279(2):630–40. https://doi.org/10.1148/radiol.2015150667.
Chao Y, Chung YH, Han G, Yoon JH, Yang J, Wang J, et al. The combination of transcatheter arterial chemoembolization and sorafenib is well tolerated and effective in Asian patients with hepatocellular carcinoma: final results of the START trial. Int J Cancer. 2015;136(6):1458–67. https://doi.org/10.1002/ijc.29126.
Yu JI, Park HC. Radiotherapy as valid modality for hepatocellular carcinoma with portal vein tumor thrombosis. World J Gastroenterol. 2016;22(30):6851–63. https://doi.org/10.3748/wjg.v22.i30.6851.
Huang M, Lin Q, Wang H, Chen J, Bai M, Wang L, et al. Survival benefit of chemoembolization plus Iodine125 seed implantation in unresectable hepatitis B-related hepatocellular carcinoma with PVTT: a retrospective matched cohort study. Eur Radiol. 2016;26(10):3428–36. https://doi.org/10.1007/s00330-015-4198-x.
Luo JJ, Zhang ZH, Liu QX, Zhang W, Wang JH, Yan ZP. Endovascular brachytherapy combined with stent placement and TACE for treatment of HCC with main portal vein tumor thrombus. Hep Intl. 2016;10(1):185–95. https://doi.org/10.1007/s12072-015-9663-8.
Lu J, Guo JH, Zhu HD, Zhu GY, Chen L, Teng GJ. Safety and efficacy of irradiation stent placement for malignant portal vein thrombus combined with transarterial chemoembolization for hepatocellular carcinoma: a single-center experience. JVIR. 2017;28(6):786–94.e3. https://doi.org/10.1016/j.jvir.2017.02.014.
Zhang FJ, Li CX, Jiao DC, Zhang NH, Wu PH, Duan GF, et al. CT guided 125iodine seed implantation for portal vein tumor thrombus in primary hepatocellular carcinoma. Chin Med J. 2008;121(23):2410–4.
Luo J, Yan Z, Liu Q, Qu X, Wang J. Endovascular placement of iodine-125 seed strand and stent combined with chemoembolization for treatment of hepatocellular carcinoma with tumor thrombus in main portal vein. Journal of vascular and interventional radiology: JVIR. 2011;22(4):479–89. https://doi.org/10.1016/j.jvir.2010.11.029.
Yang M, Fang Z, Yan Z, Luo J, Liu L, Zhang W, et al. Transarterial chemoembolisation (TACE) combined with endovascular implantation of an iodine-125 seed strand for the treatment of hepatocellular carcinoma with portal vein tumour thrombosis versus TACE alone: a two-arm, randomised clinical trial. J Cancer Res Clin Oncol. 2014;140(2):211–9. https://doi.org/10.1007/s00432-013-1568-0.
Yu TZ, Zhang W, Liu QX, Li WH, Ma JQ, Zhang ZH, et al. Endovascular brachytherapy combined with portal vein stenting and transarterial chemoembolization improves overall survival of hepatocellular carcinoma patients with main portal vein tumor thrombus. Oncotarget. 2017;8(7):12108–19. https://doi.org/10.18632/oncotarget.14520.
Zhu HD, Guo JH, Mao AW, et al. Conventional stents versus stents loaded with (125)iodine seeds for the treatment of unresectable oesophageal cancer: a multicentre, randomised phase 3 trial. Lancet Oncol. 2014;15:612–9.
Zhu HD, Guo JH, Zhu GY, et al. A novel biliary stent loaded with (125)I seeds in patients with malignant biliary obstruction: preliminary results versus a conventional biliary stent. J Hepatol. 2012;56:1104–11.
Yao LH, Su L, Liu L, Sun HT, Wang JJ. Stenting of the Portal Vein Combined with Different Numbers of Iodine-125 Seed Strands: Dosimetric Analyses. Chin Med J. 2017;130(18):2183–9. https://doi.org/10.4103/0366-6999.213974.
Funding
This study was supported by Jiangsu Provincial Medical Talent funding (Grant Number ZDRCA2016038).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Animal Ethics Committee of Suzhou University in China. The Experimental Animal Center of Suzhou University provided six pigs that were single-housed. Food intake was monitored, and the animals were housed according to the standard procedures. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Wang, C., Wang, W., Shen, J. et al. Feasibility of Helical I-125 Seed Implant in the Portal Vein. Cardiovasc Intervent Radiol 42, 121–129 (2019). https://doi.org/10.1007/s00270-018-2059-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2059-0