Abstract
Purpose
Portal vein embolization (PVE) is applied in patients with extended oncologic liver disease to induce hyperplasia of the future liver remnant and make resection feasible. Ultrasound (US) guidance is the gold standard for percutaneous portal vein access. This study evaluated feasibility and safety of C-arm cone beam computed tomography (CBCT) for needle guidance.
Materials and Methods
In 10 patients, puncture was performed under 3D needle guidance in a CBCT data set. Contrast-enhanced (CE) CBCT was generated (n = 7), or native CBCT was registered to pre-examination CE-CT via image fusion (n = 3). Technical success, number of punctures, puncture time (time between CBCT acquisition and successful portal vein access), dose parameters and safety were evaluated. For comparison, 10 patients with PVE under US guidance were analyzed retrospectively. Study and control group were matched for age, BMI, INR, platelets, portal vein anatomy.
Results
All interventions were technically successful without intervention-related complications. In the study group, the mean number of puncture attempts was 3.1 ± 2.5. Mean puncture time was 12 min (±10). Mean total dose area product (DAP) was 288 Gy cm2 (±154). The mean relative share of CBCT-related radiation exposure was 6% (±3). Intervention times and DAP were slightly higher compared to the control group without reaching significance.
Conclusion
CBCT-guided PVE is feasible and safe. The relative dose of CBCT is low compared to the overall dose of the intervention. This technique may be a promising approach for difficult anatomic situations that limit the use of US for needle guidance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary and secondary liver malignancies are a substantial cause of cancer-related morbidity and mortality; prevalence and incidence have been increasing over recent years [1]. Whenever possible, patients with liver malignancies are subjected to surgical resection [2,3,4]. More than 70% of the tumors are not primarily amenable to hepatic resection as the expected remaining future liver remnant (FLR) would be too small to work as functional reserve. Initially, too extended liver tumors can be rendered surgically resectable by either minimizing the tumor burden, e.g., by neoadjuvant chemotherapy [2, 4, 5] or by inducing hyperplasia and hypertrophy of healthy, non-tumor-bearing liver tissue, e.g., by portal venous embolization (PVE), portal venous ligation [6, 7] or less commonly radioembolization [8].
Portal vein embolization (PVE) is usually performed in an angiography suite under ultrasound (US) and fluoroscopic guidance. Depending on the FLR, projected type of hepatic resection, tumor extension and custom at the respective medical center, either the right or the left intrahepatic portal venous branch is punctured percutaneously under US guidance. Subsequently, typically the right portal venous system is embolized under fluoroscopic guidance, whereas embolization of the proximal 1 cm is to be avoided to facilitate surgical ligation at the time of liver resection. The embolization materials used for PVE include non-spheric polyvinyl alcohol (PVA) particles, gelatin sponge, fibrin glue, n-butyl cyanoacrylate (NBCA) with lipiodol, polidocanol foam, or combinations of these materials with coils or Amplatzer vascular plugs [6, 7, 9,10,11]. At our institution, preferably PVA particles in combination with plugs or coils are used.
Most of the generally rare but potentially serious adverse events (AE) of PVE are associated with the percutaneous liver puncture and comprise, among others, severe intraperitoneal hemorrhage, infections or portal vein thrombosis [6, 9, 12,13,14]. Minimizing the number of puncture attempts means to minimize these associated risks.
Cone beam computed tomography (CBCT) means the acquisition of a volumetric data set by rotation of the C-arm cone beam around the patient. Many applications of CBCT for transarterial interventions in neuroradiology or interventional oncology as well as percutaneous interventions like drainage placements have already been described [15,16,17]. A potential benefit of CBCT for PVE has not been investigated yet.
In this study, we evaluated feasibility and safety of CBCT for needle guidance for PVE in comparison with a retrospective group treated with PVE under US guidance.
Methods
Study Design and Patient Characteristics
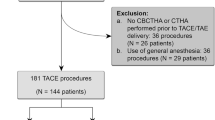
A total of 10 patients who underwent CBCT-guided PVE (study group; median age 61 years and 8 months, SD 13 years, 8 months) were enrolled. In this small-scale feasibility study, every patient who matched the inclusion criteria for PVE was considered eligible for CBCT-guided liver puncture. Patients were more likely to receive a CBCT-guided procedure if the patient had an unsuccessful US-guided PVE attempt in the past, if tumor portions in potential puncture trajectories were difficult to visualize with US or conditions for US were challenging due to anatomic peculiarities of the rib cage or adipositas. None of the patients included in this study matched the criteria of severe obesity. Underlying oncologic liver diseases were cholangiocarcinoma (CC, n = 6 in the study group, n = 7 in the control group), carcinoma of the gallbladder (n = 4 in the study group, n = 0 in the control group) and liver metastasis from colorectal cancer (LMCRC, n = 0 in the study group, n = 3 in the control group). The CBCTs were either acquired without (non-contrast-enhanced CBCT (NC-CBCT) subgroup) or with (contrast-enhanced CBCT (CE-CBCT) subgroup) intravenous contrast enhancement in portal venous phase. As control group, 10 PVE interventions (median patient age 56 years and 8 months, SD 10 years, 4 months) with conventional US guidance were retrospectively analyzed for comparison of radiation exposure as well as overall duration of the intervention. The CBCT group was matched with the US group for age, BMI, INR and platelet counts as these could interfere as potential confounders with technical success, dose parameters and patient safety. The PVE interventions were performed by two interventional radiologists with about 7 and 11 years of experience in this field. Patient characteristics are summarized in Tables 1 and 2.
Patient Preparation and CBCT Acquisition
The PVE procedures were indicated interdisciplinarily according to current guidelines. Guidelines for minimum FLR before hepatic resection recommend at least 20% for an otherwise healthy liver, 30% in fibrosis or severe parenchymal damage, e.g., after extensive chemotherapy, and at least 40% for patients with significant liver cirrhosis [12, 18, 19]. Absolute contraindications for PVE included an extensive ipsilateral tumor thrombus of the portal vein and clinically evident portal hypertension. Relative contraindications were tumor portions situated in the puncture trajectory, advanced grade liver insufficiency (Child–Pugh score C), polycystic liver disease, complete cavernous transformation of the portal vein, severe hepatic encephalopathy and severe congestive heart failure. An INR above 1.3, platelet counts below 60,000/μl, an aPTT longer than 50 s or a hemoglobin value lower than 6 mg/dl required administration of blood products prior to the intervention to minimize the risk of life-threatening hemorrhage.
Before PVE, informed consent was obtained from all patients in the study and the control group. The patient was placed in supine position with both arms elevated, and the surroundings were draped in a sterile way. CBCT was performed in lateral acquisition using a C-arm flat panel detector (Allura Xper FD20 and XperCT, Philips Healthcare, Andover, MA, USA). Within 10 s, 312 projections were acquired during a 180°–240° rotation with an automated dose modulation according to patient body weight, filtered back projection and iterative reconstruction algorithms were used to further minimize radiation dose. Projection images were automatically transferred to a commercially available workstation (XtraVision, Philips Healthcare, Andover, MA, USA) allowing for multiplanar reformatting, volume rendering and automated artifact reduction when necessary [20].
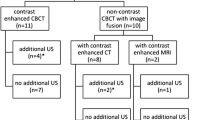
For CBCT-guided puncture trajectory planning, two different approaches were used. The first approach (NC-CBCT subgroup, Fig. 1) involved the acquisition of a non-contrast-enhanced CBCT during one breath hold in flat inspiration and a registration with the most recent CE-CT imaging of the liver in portal venous phase by means of anatomic features such as liver contours and vertebrae. Planning of the puncture trajectory was performed with the registered CE imaging.
CBCT-guided PVE in a patient with cholangiocarcinoma. Image fusion of a native CBCT acquired in the angio suite with previous CE-CT for puncture planning: A axial CE-CT slice in portal venous phase which is used for puncture trajectory planning, B anatomically corresponding native CBCT slice which is used for registration of (A). In (C) CE-CT (green) and CBCT (red) are merged by anatomic landmarks. The intended puncture trajectory is marked in violet/green. Images (D–F) show the diagnostic CT, CBCT and image fusion as well as the intended puncture trajectory in coronal reconstruction. Images (G–I) show coronal CT being superimposed and rigidly registered with fluoroscopy. Depiction of a successful puncture (G), confirmation portography (H) and the status post embolization of the right liver lobe with PVA particles and an Amplatzer plug in DSA (I). Note the biliary drains in both liver lobes
The second approach (CE-CBCT subgroup, Fig. 2) was to generate a CE-CBCT during one breath hold in flat inspiration and portal venous phase timing which was accomplished by injection of 100 ml Imeron 300 and 20-ml NaCl with a flow of 4 ml/s and a scan delay of 55 s. The resulting volumetric data set was used directly for puncture trajectory planning without further registration to preexisting imaging.
42-year-old woman who suffered from a locally recurrent carcinoma of the gall bladder. As sonographic visualizablitiy of the cholangiocarcinoma was poor, CE-CBCT was used for intraprocedural image fusion and 3D guidance of the portal vein puncture. In (A) and (B) pre-interventional CE-CT and Gd-EOB-DTPA-enhanced MRI show a central cholangiocarcinoma in liver segment 4a/b. Axial (C) and coronal (D) CE-CBCT reconstructed images allowed for clear identification of the main portal vein and proximal right portal vein branch for virtual needle track planning (green scale). Entry and target point for portal vein puncture were marked manually, and the volumetric data set then was laid over the real-time fluoroscopy image (E). The wire inside the portal vein is marked with arrow tips; the asterisk marks the sheath/entry point. Successful puncture of the right portal vein branch along the planned trajectory is documented (E), contrast medium was injected to confirm the access to the portal venous system. F DSA shows successful embolization of the right anteromedial and posterolateral portal vein branches, the former arising from the left portal vein as an anatomic variant
CBCT-Guided PVE Procedure
The PVE procedure was performed under adequate intravenous analgosedation (15 mg piritramid, Dipidolor®; 5 mg midazolam, Dormicum®) and local anesthesia in line with standards of care; a general anesthesia was not necessary for any patient.
After acquisition of the CBCT, a dedicated software for real-time 3D needle guidance (XperGuide; Philips Healthcare, Andover, MA, USA) was used for both marking a suitable cutaneous needle entry point and a target point in the right portal vein. Once the puncture trajectory was planned and co-registered, the volumetric data set was rigidly linked and superimposed with 2D fluoroscopic imaging. Thus, any C-arm movement was followed by real-time correction of the respective multiplanar reconstruction.
PVE was then performed according to the standards of the institution as follows. Along the planned trajectory, a right portal venous branch was punctured with a 21 G/ 15 cm puncture needle. After successful portal vein puncture and insertion of a NEFF-set (Cook) over a 0.018″ stiff wire, an initial portography in antero-posterior (AP) or 30° right anterior oblique (RAO) projection was acquired. By using a 0.035″ wire, a 4-F Cordis brite tip sheath was inserted. After insertion of a sidewinder-1 tempo catheter (Cordis) into the right portal vein branches, embolization was carried out by injection of non-spheric PVA particles ranging between 500 and 700 µm (Contour, Boston Scientific). Once stasis of portal venous blood flow in the respective branch was seen, preferably an Amplatzer plug type I or II (12–16 mm, St. Jude Medical) was placed if embolization of the proximal 1 cm right portal vein could be avoided for surgical resection purposes. Whenever this was not possible, coil embolization (Tornado 8–10 mm, Cook) was performed instead. In a pull-back maneuver, the puncture tract was closed by using fibrin glue (Tisseel, Baxter).
Data Analysis
A portal vein puncture and access verified by a consecutive portography were considered as technical success. The number of puncture attempts necessary, the time span between CBCT acquisition and successful puncture of the portal vein (planning and puncture time), the effects on overall duration of the procedure (defined from first to last documented image) and dose parameters [dose area product (DAP) according to the dose report] as well as incidence and severity of intervention-related complications were analyzed.
Statistics
Statistics were performed using the statistical software SPSS 23.0 (SPSS Inc., New York, NY, USA). p ≤ 0.05 was considered statistically significant, and p ≤ 0.1 was considered a trend. The Mann–Whitney U test for non-normal distributed, independent samples was applied to assess level of significance.
Results
The technical success rate of CBCT-guided PVE was 100%.
Virtual puncture trajectory planning and real-time 3D needle guidance were feasible in all patients of the study subgroups. The mean number of puncture attempts to gain portal venous access was 3.1 (±2.5) for all patients treated with CBCT-guided PVE (Table 3). Within the study groups, there were less puncture attempts necessary in the subgroup that received a CE-CBCT (2.6 ± 2.1) compared to the subgroup with prior diagnostic imaging being registered to native CBCT scans (4.3 ± 3.2, p = 0.30) (Table 4).
Mean planning and puncture time averaged for both study subgroups were 12 min (±10), whereas mean puncture times tended to be shorter in the CE-CBCT subgroup with 8.7 min (±7.5) compared to the NC-CBCT subgroup with 18 min (±15) (p = 0.25) (Table 4). As the expended time for sonography was not documented in the control group, only the mean procedure times after successful portal vein access were compared between study groups and control. Those were longer in the study groups with 61 min (±27) compared to 41.6 min (±15.2) in the control group (p = 0.04). Mean total procedure times that comprise the CBCT acquisition as well as planning and successful execution of the puncture were 73 min (±27) in the study groups (Table 3). Within the study groups, the NC-CBCT subgroup had shorter total procedure times with 63 min (±21) than the CE-CBCT subgroup with 77 min (±30) (p = 0.67) (Table 4). In the CE-CBCT subgroup, three out of seven patients showed a complex portal vein anatomy with the right anterior segmental branch arising from the left portal vein, requiring a more careful embolization; in the control group, one patient had the variant of a portal vein trifurcation.
Mean total DAP was higher in the study group (288,060 ± 154,383 mGy cm2) compared to the control group (178,501 ± 115,221 mGy cm2, p = 0.12) (Table 3). The mean dose share of the CBCT made up 6.0% (±3.1) (14,323 ± 5116 mGy cm2) of total DAP in the study group. In comparison, the mean DAP in the CE-CBCT subgroup of 354,085 mGy cm2 (±131,145) was higher than the average total DAP in the NC-CBCT subgroup with 134,001 mGy cm2 (±69,262). In the NC-CBCT subgroup, the additional CBCT made up 8.72% (±4.6) of the total DAP; in the CE-CBCT subgroup, it was 4.9% (±1.5) (p = 0.07) (Table 4).
No major intervention-related complications in terms of relevant internal bleeding, liver hematoma, portal vein thrombosis, liver failure, pneumothorax or infection were seen.
In all cases, sufficient growth of the FLR was achieved and hepatic resection, mostly trisectionectomy, could be performed within 3–4 weeks post-PVE.
Discussion
PVE has become a standard procedure to render initially nonresectable oncologic liver disease resectable. Puncture of the intrahepatic portal vein is the first and crucial step of PVE and bears most of the risks associated with the procedure [6, 9, 12, 13]. Gold standard for percutaneous puncture of the portal vein is US guidance which requires favorable conditions for sonography and becomes more difficult in obese patients or in advanced liver steatosis. Furthermore, sonographic visualization of tumor portions or metastasis in an intended puncture trajectory can be challenging. The potential contribution of CBCT guidance for PVE to address these challenges as well aspects of general feasibility and safety was subject of this study.
For this study, either non-enhanced CBCT scans were merged with previously acquired CE cross-sectional imaging (NC-CBCT subgroup) or CE-CBCT scans were acquired and directly used for puncture planning (CE-CBCT subgroup). In patients without renal impairment (glomerular filtration rate >90 ml/min), the second approach was indicated whenever pre-interventional diagnostic imaging was not up-to-date or not suitable for puncture planning e.g., due to image quality issues. Both approaches proved feasible for puncture planning and 3D real-time navigation. PVE could be performed safely and successfully in all patients enrolled in the study without any major AE. When simulating different puncture trajectories in a 3D data set, tumor masses were clearly visible in any reconstruction and could systematically be avoided for puncture trajectory planning which we see as a major advantage of the method over the sonographic gold standard.
Comparing the data between the two study subgroups, CE-CBCT imaging (CE-CBCT subgroup, 2.6 ± 2.1 attempts) seemed to allow for a more accurate planning of the puncture trajectory compared to CBCT-merged pre-interventional imaging without reaching significance given the small case number (NC-CBCT subgroup, 4.3 ± 3.2 attempts, p = 0.30). Correspondingly, puncture times in the CE-CBCT subgroup tended to be lower than in the NC-CBCT subgroup. This is a conclusive finding as the liver follows any diaphragmatic excursion and the anatomic situation captured in two different cross-sectional imagings is highly influenced by the depth of inspiration. In addition, there can be motion artifacts and, depending on how much time there is between two time points, progress of the disease. When two imagings are to be merged for registration there are always sacrifices to be made as 100% congruence is almost impossible to accomplish. The resulting imprecision in registration directly affects the quality for 3D procedure planning. Furthermore, diagnostic cross-sectional imaging of the abdomen usually is carried out in deep inspiration. For interventions under fluoroscopic guidance, however, the anatomic situation at breath hold flat inspiration is more representative. This is something a peri-interventional CE-CBCT can deliver. Nevertheless, the advantages of merging previous diagnostic imaging with a non-CE-CBCT over a CE-CBCT are a lesser radiation exposure, avoidance of additional contrast agent application and potentially higher image quality of previously acquired diagnostic multislice CT for puncture planning due to a better signal to noise ratio. The possibility to merge and overlay MRI and fluoroscopic imaging with a native CBCT is another interesting option to benefit from the advantages of different imaging modalities for puncture trajectory planning.
In procedure times after successful portal vein puncture, we found the interventions in the study subgroup to have taken longer than the interventions in the control group and the average DAP to be higher. It must be pointed out that the dose share of the additional CBCT made up only 8.7 ± 4.6% of the total DAP in the NC-CBCT subgroup and 4.9 ± 1.5% in the CE-CBCT subgroup (p = 0.07). The aforementioned difference in radiation exposure and intervention times can partly be attributed to a selection bias as technically challenging cases due to limited sonographic visualization of the intrahepatic portal vein or unsuccessful previous PVE procedures were elected for CBCT-guided portal vein puncture.
Another explanation is the technically more complex, and thus more time-consuming anatomic variant of the right anterior segmental branch arising from the left portal vein that 3 out of 7 patients in the CE-CBCT subgroup featured. This variant in the branching pattern of the portal vein occurs with a frequency of 2.9–4.3% and requires particular precaution to prevent accidental embolization of the left portal vein [21,22,23]. Total intervention times for two of these patients ranged well above average between 106 and 122 min with DAPs as high as 548,610 and 490,985 mGy cm2, respectively. Among the patients of the control group, just one patient showed the variant of a portal vein trifurcation.
There is no additional radiation exposure for the medical staff as the CBCT can be acquired from the control room after the personnel left the angiography suite. With iterative reconstruction algorithms for CBCT on the rise, overall patient radiation exposure as well as CBCT dose share of fluoroscopic interventions is expected to keep decreasing.
There are several limitations in this small-scale feasibility study. Study numbers were relatively low (10 patients each for study and control group), and patients were not prospectively randomized to different treatment arms. The documentation in the study and control groups were of varying levels of detail, e.g., there was a lack on data concerning the number of puncture attempts and intervention times for US guidance in the control group. In addition, procedure times were reconstructed as time span from first to last documented image, allowing potential inaccuracies. In order to make this alternative approach attractive for other institutions, larger-scaled studies should confirm our findings. In particular, further studies should corroborate the finding that the additional radiation exposure is low in proportion to the overall radiation dose of the intervention.
Conclusion
CBCT-guided PVE is feasible and safe and allows for an operator-independent visualization of potential puncture trajectories as opposed to an US-guided intervention. Beside the US-guided approach as the gold standard to gain access to the portal vein, CBCT-guided PVE can be a potentially valuable alternative in selected cases when previous US-guided PVE attempts have not been successful, conditions are not favorable for US guidance due to steatosis, high BMI or anatomic peculiarities of the rib cage or if there are liver tumor masses extending into puncture trajectories that are hard to visualize with US. It can both help to reduce the number of puncture attempts for portal venous access and to avoid accidental tumor puncture which might cause internal bleeding from aberrant tumor vessels or inoculation metastasis. CBCT only slightly increases dose exposition for patients compared to traditional US guidance; the exposition for medical staff is not elevated. A relevant impairment of renal function should be excluded if additional contrast medium was to be applied; otherwise, the technique via native CBCT and image fusion can be used.
Abbreviations
- AE:
-
Adverse effects
- BMI:
-
Body mass index
- CBCT:
-
Cone beam computed tomography
- CE:
-
Contrast enhanced
- DAP:
-
Dose area product
- FLR:
-
Future liver remnant
- INR:
-
International normalized ratio
- PVE:
-
Portal vein embolization
- US:
-
Ultrasound
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Garden OJ, Rees M, Poston GJ, et al. Guidelines for resection of colorectal cancer liver metastases. Gut. 2006;55(Suppl 3):iii1–8.
Geoghegan JG, Scheele J. Treatment of colorectal liver metastases. Br J Surg. 1999;86(2):158–69.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–83.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240(4):644–57 (discussion 657–648).
May BJ, Madoff DC. Portal vein embolization: rationale, technique, and current application. Semin Intervent Radiol. 2012;29(2):81–9.
May BJ, Talenfeld AD, Madoff DC. Update on portal vein embolization: evidence-based outcomes, controversies, and novel strategies. J Vasc Interv Radiol. 2013;24(2):241–54.
Lewandowski RJ, Kulik LM, Riaz A, et al. A comparative analysis of transarterial downstaging for hepatocellular carcinoma: chemoembolization versus radioembolization. Am J Transplant. 2009;9(8):1920–8.
Abulkhir A, Limongelli P, Healey AJ, et al. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247(1):49–57.
Geisel D, Malinowski M, Powerski MJ, et al. Improved hypertrophy of future remnant liver after portal vein embolization with plugs, coils and particles. Cardiovasc Interv Radiol. 2014;37(5):1251–8.
van Lienden KP, van den Esschert JW, de Graaf W, et al. Portal vein embolization before liver resection: a systematic review. Cardiovasc Interv Radiol. 2013;36(1):25–34.
Denys A, Bize P, Demartines N, Deschamps F, De Baere T. Quality improvement for portal vein embolization. Cardiovasc Interv Radiol. 2010;33(3):452–6.
Di Stefano DR, de Baere T, Denys A, et al. Preoperative percutaneous portal vein embolization: evaluation of adverse events in 188 patients. Radiology. 2005;234(2):625–30.
Kodama Y, Shimizu T, Endo H, Miyamoto N, Miyasaka K. Complications of percutaneous transhepatic portal vein embolization. J Vasc Interv Radiol. 2002;13(12):1233–7.
Floridi C, Radaelli A, Abi-Jaoudeh N, et al. C-arm cone-beam computed tomography in interventional oncology: technical aspects and clinical applications. Radiol Med. 2014;119(7):521–32.
McKay T, Ingraham CR, Johnson GE, Kogut MJ, Vaidya S, Padia SA. Cone-beam CT with fluoroscopic overlay versus conventional CT guidance for percutaneous abdominopelvic abscess drain placement. J Vasc Interv Radiol. 2016;27(1):52–7.
Lucatelli P, Corona M, Argiro R, et al. Impact of 3D rotational angiography on liver embolization procedures: review of technique and applications. Cardiovasc Interv Radiol. 2015;38(3):523–35.
Ribero D, Chun YS, Vauthey JN. Standardized liver volumetry for portal vein embolization. Semin Interv Radiol. 2008;25(2):104–9.
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol. 2006;13(10):1271–80.
Tacher V, Radaelli A, Lin M, Geschwind JF. How I do it: cone-beam CT during transarterial chemoembolization for liver cancer. Radiology. 2015;274(2):320–34.
Couinaud C. Liver anatomy: portal (and suprahepatic) or biliary segmentation. Dig Surg. 1999;16(6):459–67.
Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22(1):141–59.
Fraser-Hill MA, Atri M, Bret PM, Aldis AE, Illescas FF, Herschorn SD. Intrahepatic portal venous system: variations demonstrated with duplex and color Doppler US. Radiology. 1990;177(2):523–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lüdemann, W.M., Böning, G., Chapiro, J. et al. C-Arm Cone Beam CT for Intraprocedural Image Fusion and 3D Guidance in Portal Vein Embolization (PVE). Cardiovasc Intervent Radiol 41, 424–432 (2018). https://doi.org/10.1007/s00270-017-1782-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1782-2