Abstract
Systemic artery embolism is a rare complication of CT-guided lung biopsy. Immediate clinical and radiological recognitions are crucial for rapid intervention and prevention of fatal outcome. Although hyperbaric oxygen is the suggested treatment of mildly symptomatic systemic artery embolization, aspiration of air should be considered as part of the management in cases of cardiac arrest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous computed tomography-guided thoracic needle biopsy is widely used for characterization of lung nodules and establishment of final diagnosis. Its major complications include pneumothorax and hemorrhage; its rarest complications are air embolism and tumor seeding to the pleura and chest wall [1]. The clinical manifestations of systemic air embolism are cardiac arrhythmias and collapse if air enters the coronary arteries or drowsiness and seizures if air enters the cerebral circulation [1, 2]. We present a case of percutaneous computed tomography (CT) scan-guided trans-thoracic needle biopsy in a patient complicated by systemic air embolism (SAE) and cardiac arrest and discuss the management.
Case Report
A 57-year-old man with a history of lung cancer and brain metastases treated with chemoradiation and craniotomy presented with a new 1.2-cm nodule in the lateral basal segment of the left lower lobe that was mildly avid on the PET-CT. No other avid disease was seen on the PET-CT. The patient was referred for a CT-guided lung biopsy for confirmation of pathology and to rule out progression of the disease, as well as consideration of immune therapy.
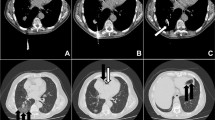
The procedure was performed under general anesthesia because of the patient’s body habitus and inability to cooperate with breathing instructions. Controlled breathing was utilised using pressure control volume guarantee and breathing was always stopped during inspiration. The patient was positioned in the right decubitus position. A 5.0-cm co-axial 20-gauge/22-gauge core biopsy set (Cook, Denmark) was used to access the left lower lobe nodule. Intermittent CT scanning was performed to confirm an appropriate trajectory, followed by the advancement of the needle to the lesion. A small pneumothorax developed which did not affect the position of the needle, and a single core biopsy was obtained under water seal (Fig. 1). Air was noticed to come out of the co-axial needle; therefore, another CT was performed prior to any further biopsies to confirm position. Air was seen in the left pulmonary vein, left atrium and left ventricle, aortic arch, left coronary artery, left vertebral artery and left subclavian artery and its branches in the arm (Fig. 2). There was no obvious bronchus in the trajectory of the needle. A small amount of parenchymal hemorrhage was noted near the tip of the needle.
As images were being evaluated, the patient developed cardiac arrest and code was activated.
The patient was immediately turned on his back to facilitate CPR. Left femoral artery access was obtained on the CT table using anatomical landmarks, and a 120-cm 5F pigtail catheter (Cook, Denmark) was inserted over the wire over what was judged to be the length sufficient to reach the left ventricle. Using negative suction on a 20-ml syringe, air and blood were aspirated blindly from the left ventricle and aorta during the withdrawal of the catheter back to the descending aorta. This maneuver was repeated several times confirming adequate positioning. During this time, advanced cardiovascular life support (ACLS) algorithm was followed; cardiopulmonary resuscitation (CPR) was performed intermittently, and the patient received several shocks.
Once the patient was stabilized after 30 min, he was transferred to the adjoining angiography suite, and the catheter position was confirmed under fluoroscopy to be in the left ventricle, and further aspiration and pullback was continued (Fig. 3); simultaneously, a left pleural 8F pigtail catheter (Argon, USA) was inserted to evacuate the left pneumothorax. The patient went into cardiac arrest on two more occasions, but resuscitation was successful each time. Final cone beam CT performed showed resolution of all the air in the left ventricle and aorta, as well as in the remaining arteries. Transesophageal ultrasound did not show any significant cardiac dyskinesia.
CT of brain, chest and abdomen were performed thereafter, confirming complete resolution of air in the left ventricle, aorta, coronaries and pulmonary veins (Fig. 4). No large territorial infarct was seen in the brain.
The patient was then transferred to the ICU. Hypothermia was not considered necessary after clinical evaluation. The following day, he was extubated and had normal neurological examination with minimal disorientation. He was transferred to the floor and discharged the day after.
Discussion
Complications of CT-guided needle biopsy based on a study including 9783 biopsies in Japan were pneumothorax (35%), tumor seeding at the site of the biopsy route (0.061%), tension pneumothorax (0.1%) and systemic air embolism (SAE) (0.061%) [3]. A study performed by Freund et al. of a smaller cohort of over 610 patients postulated a higher incidence of radiological incidence of SAE estimated at 3.8% with only a clinically significant incidence of 0.49% [4]. However, it is not clear how many of their patients had the procedure under general anesthesia.
There are three possible mechanisms for air entering the systemic circulation [5]. The first mechanism is air entering the systemic circulation secondary to a communication between the pulmonary vein and the atmosphere. The second mechanism is secondary to communication between a bronchus and the pulmonary vein or other communication between air-containing spaces and pulmonary veins. The third mechanism may occur when air crosses the pulmonary microvasculature from the pulmonary arterial system to the pulmonary venous circulation. No obvious broncho-venous communication was seen in our case; however, the source of the SAE may have been the pneumothorax.
There are postulated independent risk factors for the development of SAE: depth of the needle in the lesion, endotracheal intubation, lesion located above the level of the left atrium and prone position [4]. In our case, the lesion was below the left atrium, and the patient was in decubitus position; however, he was intubated.
SAE results in end-artery obstruction. If air enters the coronary circulation, the patient may develop cardiac arrhythmias and secondary circulatory collapse. If air enters the cerebral circulation, the patient may develop seizures with neurological deficits and stroke [1, 2].
Once SAE occurs and the symptoms are mild, the patient should be positioned in the Trendelenburg position to prevent the air from traveling to the cerebral circulation. 100% oxygen should be promptly administered, to help the exchange of oxygen for nitrogen within the air bubbles and fasten their resorption [1].
There are no available data to support the success of air aspiration by catheter insertion into the left ventricle during a SAE-induced hemodynamic compromise [6], although the procedure was reported in two patients in the literature, one in the large study in Japan [7] and the second in a recent case report [8]. Both of the patients did not appear to have had cardiac compromise. However, this instantaneous maneuver of aspirating large amount of free air has proven to be lifesaving in our case. The success of the maneuver is directly related to the quantity of air removed [9] in a study performed in animals. Although this maneuver is not well studied due to the incidental cases of SAE, it should be considered part of the management.
Therefore, immediate trans-catheter removal of systemic air embolism may be a lifesaving maneuver and should be considered part of the management in the case of severe cardiac compromise following the rare complication of arterial air embolism.
References
Wu C, Maher M, Shepard J. Complications of CT guided percutaneous needle biopsy of the chest: prevention and management. AJR. 2011;196(6):W678e82.
Hare S, Gupta A, Goncalves A, Souza C, Matzinger F, Seely J. Systemic arterial air embolism after percutaneous lung biopsy. Clin Radiol. 2011;66(7):589e96.
Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. 2006;59:60e4.
Freund MC, Petersen J, Goder KC, Bunse T, Wiedermann F, Glodny B. Systemic air embolism during percutaneous core needle biopsy of the lung: frequency and risk factors. BMC Pulm Med. 2012;12:2.
Mansour A, AbdelRaouf S, Qandeel M, Swaidan M. Acute coronary artery air embolism following CT-guided lung. Cardiovasc Intervent Radiol. 2005;28:131–4.
Mirski MA, Lele AV, Fitzsimmons L, Toung TJ. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007;106:164–77.
Ishii H, Hiraki T, Gobara H, Fujiwara H, Mimura H, Yasui K. Factors for systemic air embolism as a complication of percutaneous CT-guided lung biopsy: multicenter case-control study. Cardiovasc Interv Radiol. 2014;37(5):1312–20.
Chamsuddin A, Ashou R. Treatment of massive systemic air embolism during lung biopsy. Arab J Interv Radiol. 2017;1(1):33–6.
Colley PS, Artu AA. Bunegin-albino catheter improves air retrieval and resuscitation from lethal air embolism in up-right dogs. Anesth Analg. 1989;68:298–301.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
El Homsi, M., Haydar, A., Dughayli, J. et al. Trans-Catheter Aspiration of Systemic Air Embolism Causing Cardiac Compromise During CT-Guided Lung Biopsy, a Potentially Lifesaving Maneuver. Cardiovasc Intervent Radiol 42, 150–153 (2019). https://doi.org/10.1007/s00270-018-2055-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2055-4