Abstract
Purpose
To determine risk factors for systemic air embolism by percutaneous computed tomography (CT)-guided lung biopsy.
Methods
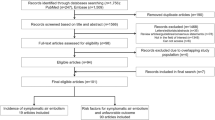
This case-control study used data from 2216 percutaneous lung biopsy procedures performed over 11 years at 12 institutions in Japan. Systemic air embolism was identified by retrospective review of CT images obtained during and immediately after the procedures. To fulfill our objective, multiple variables were compared between cases and controls with univariate analyses by using Student’s t test and Fisher’s exact test for numerical and categorical values, respectively. Multivariate logistic regression analysis was then performed using selected variables.
Results
Ten cases of systemic air embolism and 2,206 controls were identified. Univariate analyses showed that the lesions in the lower lobe (P = 0.025) and occurrence of parenchymal hemorrhage (P = 0.019) were significant risk factors. Multivariate analysis showed that the use of a larger biopsy needle was a significant risk factor (P = 0.014).
Conclusion
Parenchymal hemorrhage during the procedure, lesions in the lower lobe, and the use of larger biopsy needles may be risk factors for systemic air embolism by percutaneous CT-guided lung biopsy. Our findings may provide clues toward minimizing the risk of this complication.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous computed tomography (CT)-guided lung biopsy is a procedure that can provide high diagnostic accuracy for pulmonary lesions [1]. Systemic air embolism is a potentially fatal complication and is thus of considerable concern. The risk of this complication was thought to be quite low—0.02 to 0.07 % according to a review of the literature [2–4]. However, some recent studies show higher risks [5–8]. In 2007, Hiraki et al. [5] reported four cases of this complication from a single institution, for a risk of 0.4 % (4 of 1,010). Several researchers subsequently reported multiple cases from single centers with risks ranging from 0.16 to 0.27 % [6–8]. Recognizing the risk factors for this complication is important for minimizing the risk. In previous case reports, various factors have been assumed to contribute to this complication, including coughing during the procedure [9, 10], positive pressure ventilation [11, 12], needle tip placement within a pulmonary vein [13], procedure for a cystic or cavitary lesion [14–16], patients with vasculitis [17–19], and lesions exhibiting ground glass opacity [5]. However, risk analysis has been rarely performed because the rarity of this complication may interfere with performing such an analysis restricted to data from a single center. Therefore, we carried out a multicenter case-control study to determine the risk factors for systemic air embolism by percutaneous CT-guided lung biopsy.
Materials and Methods
Study Design and Study Population
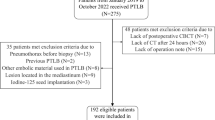
This was a case-control study using data collected between April 2000 and April 2011 from 12 institutions in Japan. These institutions were selected from 18 institutions in five prefectures in Western Japan that employed members of the Society of Angiography and Interventional Radiology Okayama (SAIRO). These 12 institutions were selected because members of SAIRO perform CT-guided lung biopsy; the other six institutions were excluded because they do not. During the 11-year period, a total of 2,216 procedures were performed, constituting the study population. Transthoracic biopsies for mediastinal or pleural lesions were excluded. This study included three cases of systemic air embolism by CT-guided lung biopsies that were reported previously [5]. Review board approval with a waiver of informed consent for performing the present study was obtained from the main institution (Okayama University Medical School) as well as the other six institutions. The remaining five institutions did not require review board approval for the use of data for the present study.
Percutaneous CT-guided Lung Biopsy Procedures
Informed consent, including acknowledgment of a risk of systemic air embolism, was obtained from patients before the procedure. Patients who received antiplatelet or anticoagulant drugs were asked to stop taking those before the procedure, if possible. Otherwise, the drugs were replaced by intravenous heparin, which was then stopped 4 h before the procedure. The patients with coagulopathy (e.g., platelet count <30,000/μl or prothrombin time-international normalized ratio >1.5) did not undergo the procedure.
All procedures at the main institution were performed percutaneously under CT guidance by an experienced radiologist or a radiology trainee under the direct supervision of an experienced radiologist. All procedures in other 11 institutions were performed by radiologists who had at least a few years of experience of CT-guided lung biopsy in a main institution. Positive pressure ventilation was not used during the procedure in any of the patients. A cutting biopsy needle was used in all procedures. Although two notch sizes (10 and 20 mm) were available, the notch length was always set at 20 mm because we believed that more specimens improving diagnostic accuracy could be obtained with this notch length. Although a 20-gauge coaxial biopsy needle system was selected in the majority of the cases, needles larger than 20 gauge (18 or 16 gauge) and noncoaxial methods were occasionally selected. The exact reasons for such selections were not determined in this retrospective study.
CT scans were obtained to target the lesion. Needle paths that did not cross visible bronchi and relatively large vessels were determined. After administration of a local anesthetic, the biopsy needle was advanced through or without an introducer needle until its tip was positioned in front of the lesion. Because no pathologist was available on site, specimen acquisition was repeated until the operators considered the specimens adequate. Immediately after the acquisition of the specimens, chest CT images were obtained to evaluate complications, including systemic air embolism. No other interventions that could cause systemic air embolism were performed.
Data Collection
The CT images obtained before, during, and after the procedure, patient charts, and procedure records of 2,216 patients were retrospectively reviewed to collect data between May 2011 and September 2011. For risk analysis, multiple variables related to the patients, lesions, and procedures were collected. The patient variables included age, sex, and the presence of pulmonary emphysema. Pulmonary emphysema was diagnosed if centrilobular or panlobular emphysema, bullae, and blebs were observed anywhere in the lung on CT images.
The lesion variables included size (long axis diameter), lobar location (upper and middle lobes or lower lobe), distance to the pleura, subtype of lesion (pure ground glass, partly solid, or solid), and biopsy diagnosis (malignant or benign). The distance to the pleura was the shortest length from the pleura to the lesion. Ground glass opacity was defined as a homogeneous appearance on high-resolution CT with hazy increased attenuation of the lung and preservation of the bronchial and vascular margins [20]. The lesions with a ground glass opacity component of >95 % were designated pure ground glass opacity lesions, whereas those with a ground glass opacity component of <5 % were designated solid lesions. The other lesions were designated as partly solid lesions.
The procedure variables included the patient position, use of a coaxial needle system, size of the biopsy needle used (20 gauge or larger [18 or 16 gauge]), number of specimens obtained, duration of the procedure, operator’s experience of the procedure, occurrence of pneumothorax, and occurrence of parenchymal hemorrhage. Operator’s experience was expressed as the number of years since the operator started performing CT-guided lung biopsy. The duration of the procedure was estimated as the time between CT scanning to target the lesion and CT scanning immediately after the procedure. Parenchymal hemorrhage was defined as new parenchymal infiltration on CT images obtained immediately after the procedure. However, haziness only along the needle tract was not considered to represent parenchymal hemorrhage.
Case Identification
To identify cases of systemic air embolism, CT images obtained during and immediately after the 2,216 lung biopsies were reviewed retrospectively. If a hypodense area suspected to represent air was found in the systemic circulation, the region of interest was placed on it. A Hounsfield unit value of less than −200 was indicative of systemic air.
Data Analysis
The missing data in the controls were excluded from the analysis. First, univariate analyses were performed by Student’s t test and Fisher’s exact test for numerical and categorical values, respectively. Second, crude and adjusted odds ratios (ORs) were calculated using univariate and multivariate logistic regression analyses, respectively. The multivariate analysis was performed by including all but one variable with zero value in a given category, which would interfere with the accurate estimation of the P value and OR. Third, supplementary analyses were subsequently performed to address the issue of overadjustment. Thus, we adjusted the variables for which the P value was <0.10 in the univariate or the multivariate analysis sequentially for patient factors, lesion factors, and procedure factors. The variable with a value of zero in a given category was also excluded from these supplementary analyses.
ORs were calculated with 95 % confidence intervals (CIs). A P value of <0.05 was considered statistically significant. Statistical analysis was performed by SPSS software, version 19.0 (IBM, Armonk, NY).
Results
We identified 10 cases of systemic air embolism at five institutions for an overall risk of 0.45 % (10 of 2,216). The remaining 2,206 procedures were served as controls. In the five asymptomatic cases, an operator incidentally noticed systemic air on CT images obtained immediately after biopsy. In four of the five symptomatic cases, an operator suspected systemic air embolism from the patients’ symptoms and then confirmed systemic air on CT images. In the remaining symptomatic case, an operator suspected systemic air embolism but did not detect it on the CT images. However, systemic air was found when the CT images were retrospectively reviewed at the time of this study.
The characteristics of the 10 cases are summarized in Tables 1 and 2. Briefly, systemic air was demonstrated in the left chamber of the heart (Figs. 1, 2), the aorta (Figs. 1, 2), and the coronary artery (Fig. 3). In two cases, systemic air was also detected in the cerebral or cerebellar artery on brain CT images obtained after the chest CT scan (Fig. 3). Patient symptoms and signs varied from no symptoms to signs to rapid manifestation of shock status with loss of consciousness. The treatments also varied among the cases and included no treatment, 100 % O2 administration, hyperbaric oxygen therapy, and suction of aortic air though a catheter. Regardless, all 10 cases were nonfatal with no sequelae.
Patient 6. CT fluoroscopic image obtained during biopsy with the patient in the prone position showing air (large arrows) in the descending aorta and the left atrium. The large arrowhead denotes the biopsy needle being introduced into the solid tumor (small arrowhead). Note the parenchymal hemorrhage (small arrows)
Patient 10. A CT fluoroscopic image obtained during biopsy with the patient in the prone position showing a coaxial biopsy needle (arrow) being introduced into the solid lesion (arrowhead). B CT image obtained immediately after biopsy with the patient in the prone position showing air (arrows) in the right coronary artery. C Brain CT image obtained after biopsy showing air (arrow) in the left cerebellar artery
Table 3 lists the distributions of all variables in both the cases and the controls and shows the results of univariate analyses by Student’s t test or Fisher’s exact test. The lobar location of the lesion and occurrence of parenchymal hemorrhage were significant risk factors (P = 0.025 and 0.019, respectively).
Table 4 presents the results of the univariate and multivariate logistic regression analyses. The univariate logistic regression analyses showed that the risk for systemic air embolism was 5.25 times higher for lesions in the lower lobe than for those in the upper and middle lobes, and it was infinitely higher for procedures accompanied with parenchymal hemorrhage than for those without. The variable of parenchymal hemorrhage was excluded from the multivariate logistic regression analysis because it accompanied all cases and absence of parenchymal hemorrhage in cases thus had zero value. The multivariate analysis showed that the use of biopsy needle >20 gauge was a significant risk factor (P = 0.014), posing a 10.1 times higher risk than the use of a 20-gauge needle. Smaller lesion size tended to increase the risk, although this trend was not significant (P = 0.08).
In the supplementary analyses, the effects of the lesion size, lobar location of the lesion, and size of the biopsy needle were adjusted sequentially for patient factors, lesion factors, and procedure factors. The variable of parenchymal hemorrhage was excluded from the analyses. The supplementary analyses yielded adjusted ORs of 0.93 to 0.95, 3.12 to 8.21, and 3.25 to 5.30 for procedures on larger lesions, the use of biopsy needles >20 gauge, and lesions in the lower lobe, respectively.
Discussion
Our study suggested that the use of a larger biopsy needle, parenchymal hemorrhage, and lesion in the lower lobe were risk factors for systemic air embolism. Among these, the use of a larger biopsy needle is an avoidable factor. The use of a larger biopsy needle as a risk factor can easily be explained by the creation of larger bronchovenous fistulas as a result of using larger biopsy needles, increasing the risk of systemic air embolism. Parenchymal hemorrhage was an important risk factor, with a crude OR of ∞. Parenchymal hemorrhage cannot always be avoided, but its risk may be reduced. Parenchymal hemorrhage may indicate injury of the pulmonary vessels. Alveolar air may be introduced into the pulmonary vein through the injured venous wall. Furthermore, parenchymal hemorrhage may promote the coughing up of blood. Although the pulmonary vein pressure is normally only 10 cm H2O, intrapulmonary pressure rises markedly to 180 cm H2O or even higher during the early phase of coughing before glottic opening [21]. Given these facts, coughing induced by parenchymal hemorrhage may facilitate the migration of alveolar air into the pulmonary vein as a result of the marked elevation of the pressure gradient. In fact, a coughing episode was observed in five of the 10 patients. Furthermore, parenchymal hemorrhage is theoretically attributable to a considerable extent to cutting of the lung parenchyma, which increases the risk of the creation of a bronchovenous fistula.
Location of the lesion in the lower lobe is another risk factor, but this is inevitable. The vessels are much larger in the lower lobes than those in other lobes. Thus, procedures performed in the lower lobe may pose a higher risk of injuring the veins and thereby causing systemic air embolism. Greater respiratory motion, which is more likely to enlarge the needle tract, occurs during the procedure in the lower lobe. Greater respiratory motion of the lung may also make the procedure more difficult and necessitate a greater number of redirections of the needle to reach the lesion. Injury to the pulmonary vein and airway by needle redirection and enlarged needle tracts may possibly increase the risk for systemic air embolism. Lobar location of the lesion is related to patient positioning during the procedure. Thus, the patient positioning was prone in seven cases because most of the patients with a lesion in the lower lobe were placed in the prone position. However, patient positioning was not significantly associated with the occurrence of systemic air embolism.
Smaller lesions tended to increase the risk for systemic air embolism. Biopsy for a smaller lesion is more likely to be accompanied with a cutting of the parenchyma that causes creation of a bronchovenous fistula. Especially for lesions <20 mm in size, the procedure could be accompanied with cutting of the parenchyma because we always selected 20 mm as the notch size of the biopsy needle regardless of lesion size.
The results of the present study may provide clues for designing methodological precautions to minimize the risk of systemic air embolism. Given that cutting the parenchyma causes parenchymal hemorrhage, specimens should be obtained only from the lesion, rather than from parenchymal areas, whenever possible. Therefore, the notch size of the biopsy needle should be set at 10 mm rather than 20 mm for lesions <20 mm in size. One might suggest that 20-mm notch size is preferable because the larger the tissue sample, the better it is for diagnosis; indeed, additional specimen is required especially for examination via immunohistochemistry and for analysis of gene mutation. In our opinion, however, greater sample can be obtained by repeating specimen acquisition with a 10-mm notch rather than by selecting the 20-mm notch. A coaxial needle system may facilitate repetition of specimen acquisition. When the specimen is deemed nevertheless inadequate, a 20-mm notch size may be selected. Furthermore, operators should use 20-gauge biopsy needles rather than larger needles. Despite the acquisition of a larger sample with the use of larger needles, Hiraki et al. [1] showed 95 % diagnostic accuracy with the use of 20-gauge needles for 1,000 lung lesions.
Our findings must be interpreted with caution because of the inherent and unavoidable limitations in the study. The data were collected from the institutions belonging to a specific society. Thus, the results might not be generalizable to other institutions. Data were missing for several variables. The rarity of this complication resulted in a small number of cases, leading to large CIs. Multiple testing is associated with an inflated type I error rate. Another limitation is the potential for residual confounders. For example, coughing during the procedure was not evaluated because of the considerable amount of missing data in the control group. Furthermore, parenchymal hemorrhage was excluded from the adjusted models but may act as a residual confounder. Therefore, we recognize that the present study is a preliminary one. Further larger studies are required to confirm or refute the present findings.
In conclusion, parenchymal hemorrhage during the procedure, the use of larger biopsy needles, and lesions in the lower lobe may be risk factors for systemic air embolism by percutaneous CT-guided lung biopsy. Our findings may provide clues toward minimizing the risk of this complication.
References
Hiraki T, Mimura H, Gobara H et al (2009) CT fluoroscopy-guided biopsy of 1000 pulmonary lesions performed with 20-gauge coaxial cutting needles: diagnostic yield and risk factors for diagnostic failure. Chest 136:1612–1617
Sinner WN (1976) Complications of percutaneous transthoracic needle aspiration biopsy. Acta Radiol Diagn 17:813–828
Richardson CM, Pointon KS, Manhire AR, Macfarlane JT (2002) Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol 75:731–735
Tomiyama N, Yasuhara Y, Nakajima Y et al (2006) CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 59:60–64
Hiraki T, Fujiwara H, Sakurai J et al (2007) Nonfatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest 132:684–690
Um SJ, Lee SK, Yang DK et al (2009) Four cases of a cerebral air embolism complicating a percutaneous transthoracic needle biopsy. Korean J Radiol 10:81–84
Ibukuro K, Tanaka R, Takeguchi T et al (2009) Air embolism and needle track implantation complicating CT-guided percutaneous thoracic biopsy: single-institution experience. AJR Am J Roentgenol 193:W430–W436
Kuo HL, Cheng L, Chung TJ (2010) Systemic air embolism detected during percutaneous transthoracic needle biopsy: report of two cases and a proposal for a routine postprocedure computed tomography scan of the aorto-cardiac region. Clin Imaging 34:53–56
Ishikawa Y, Matsuguma H, Nakahara R et al (2009) Arterial air embolism: a rare but life-threatening complication of percutaneous needle biopsy of the lung. Ann Thorac Surg 87:1622
Kau T, Rabitsch E, Celedin S et al (2008) When coughing can cause stroke: a case-based update on cerebral air embolism complicating biopsy of the lung. Cardiovasc Intervent Radiol 31:848–853
Baker BK, Awwad EE (1988) Computed tomography of fatal cerebral air embolism following percutaneous aspiration biopsy of the lung. J Comput Assist Tomogr 12:1082–1083
Worth ER, Burton RJ Jr, Landreneau RJ et al (1990) Left atrial air embolism during intraoperative needle biopsy of a deep pulmonary lesion. Anesthesiology 73:342–345
Mokhlesi B, Ansaarie I, Bader M et al (2002) Coronary artery air embolism complicating a CT-guided transthoracic needle biopsy of the lung. Chest 121:993–996
Ohashi S, Endoh H, Honda T et al (2001) Cerebral air embolism complicating percutaneous thin-needle biopsy of the lung: complete neurological recovery after hyperbaric oxygen therapy. J Anesth 15:233–236
Khalil A, Prigent H, Parrot A, Carette MF (2006) Systemic air embolism complicating percutaneous transthoracic needle biopsy. AJR Am J Roentgenol 187:W242–W243
Mammana RB, Petersen EA, Fuller JK et al (1983) Pulmonary infections in cardiac transplant patients: modes of diagnosis, complications, and effectiveness of therapy. Ann Thorac Surg 36:700–705
Aberle DR, Gamsu G, Golden JA (1987) Fatal systemic arterial air embolism following lung needle aspiration. Radiology 165:351–353
Regge D, Gallo T, Galli J et al (1997) Systemic arterial air embolism and tension pneumothorax: two complications of transthoracic percutaneous thin-needle biopsy in the same patient. Eur Radiol 7:173–175
Wong RS, Ketai L, Temes T et al (1995) Air embolus complicating transthoracic percutaneous needle biopsy. Ann Thorac Surg 59:1010–1011
Collins J, Stern EJ (1997) Ground-glass opacity at CT: the ABCs. AJR Am J Roentgenol 169:355–367
Agostoni E, Rahn H (1960) Abdominal and thoracic pressures at different lung volumes. J Appl Physiol 15:1087–1092
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ishii, H., Hiraki, T., Gobara, H. et al. Risk Factors for Systemic Air Embolism as a Complication of Percutaneous CT-guided Lung Biopsy: Multicenter Case-control Study. Cardiovasc Intervent Radiol 37, 1312–1320 (2014). https://doi.org/10.1007/s00270-013-0808-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0808-7