Abstract
Background
Radioembolization induced liver disease (REILD) is a possible sequela of transarterial radioembolization (TARE), particularly in cases of whole-liver treatment. To mitigate this problem, the safety and efficacy of combined transarterial chemoembolization (TACE) and TARE were evaluated for patients with bilobar hepatocellular carcinoma (HCC).
Materials and Methods
Nineteen patients (mean age 60 years; range 27–82 years) treated for HCC between June 2012 and September 2014 were included in the analysis. Each patient was treated with combined TARE and TACE for bilobar HCC, with or without portal vein thrombosis. The hepatic lobe with large HCC was treated with TARE, and the other lobe with small HCC(s) was treated with TACE. Laboratory and clinical data were investigated to determine REILD occurrence. Survival data were analyzed to compare the treatment efficacy of alternative treatment modalities, including TACE and sequential TARE.
Results
All patients underwent TARE for a dominant tumor in one lobe and TACE for small nodule(s) in the other lobe of the liver. The mean yttrium-90 microspheres used in TARE were 2.8 GBq (range; 1.0-3.5 GBq), and the mean doses of doxorubicin and iodized oil were 24.5 mg and 5.2 mL, respectively, for TACE. No statistical differences were noted between laboratory data measured before and after treatment, and no procedure-related major clinical complications occurred. The median time-to-progression of patients was 10.0 months, and the median overall survival was 27.3 months.
Conclusion
Combined radioembolization and chemoembolization appears to be a safe and effective treatment modality for bilobar HCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is among the most common cancers and the second most common cause of cancer-related mortality [1, 2]. Despite improvements in early diagnosis, 40–60% of patients are diagnosed in the intermediate stage [Barcelona clinic liver cancer stage B (BCLC-B)] or the advanced stage (BCLC-C) [3].
The BCLC guideline stipulates that transarterial chemoembolization (TACE) is the primary treatment for intermediate-stage HCC, and systemic treatment with sorafenib is recommended for advanced-stage HCC [4, 5]. Transarterial radioembolization (TARE) is a novel treatment using intra-arterial infusion of yttrium-90 (Y90)-loaded microspheres, which serve as sources of internal radiation. Recently, TARE has emerged as an alternative treatment to TACE in patients with intermediate and advanced multinodular HCC (BCLC-B/C), or HCC with portal vein thrombosis [6, 7]. According to a recent study, although no difference in overall survival at 1 year was noted between TARE and TACE (42 vs. 46%, p = 0.33), TARE was associated with less postprocedural pain and a shorter hospital stay [8].
However, whole-liver treatment with TARE can cause radioembolization induced liver disease (REILD) [9]. REILD was first reported in 2008 by Sangro et al. [10], describing various signs of hepatic dysfunction, including jaundice, ascites, and increased serum levels of bilirubin, alkaline phosphatase (ALP), and γ-glutamyl transpeptidase. The risk factors of REILD include whole-liver treatment and sequential lobar treatment less than 6 weeks [11]. For multiple and bilobar HCC with a large tumor burden, treatment should be performed sequentially, and spacing treatments more than 4–6 weeks apart are recommended to avoid possible liver toxicity [9, 12]. Unfortunately, the lag period between procedures may increase the risk of tumor progression, and the additional procedure necessitates further hospital visits along with high costs.
In order to overcome these limitations, our study combined radioembolization and chemoembolization for the treatment of bilobar HCC to evaluate the safety and effectiveness of the combined therapy.
Materials and Methods
Patients
The institutional review board approved this retrospective study and waived written informed consent. The cohort included 19 patients (mean age 60 years; range 27–82 years) who received combined TARE and TACE for bilobar HCC in our institution from June 2012 to September 2014. For each patient, demographics, BCLC stage, Child–Pugh score, tumor characteristics, procedure-related factors, and laboratory findings were evaluated. The tumor characteristics, including type, size, and presence of portal vein, hepatic vein, and bile duct invasion, were evaluated based on liver dynamic computed tomography (CT) and magnetic resonance imaging (MRI) scans.
Interventional Techniques
Planning Angiography
Planning angiography was performed for radioembolization. Celiac, superior mesenteric artery arteriography, and cone beam CT of the hepatic artery were performed to evaluate tumor distribution and feeding arteries. The right common femoral artery was used for US-guided access. After inserting a 5-Fr sheath (Terumo Corp, Tokyo, Japan), a 5-Fr catheter (Yashiro; Terumo Corp) was advanced in the common hepatic artery, and a hepatic artery arteriography was obtained to evaluate tumor distribution and feeding arteries. Then, cone beam CT of the hepatic artery was performed to accurately evaluate hepatic artery distributions and tumor-feeding arteries.
We planned to treat the lobe with the dominant or larger tumor using TARE and the lobe containing small tumor(s) using TACE. Hepatopulmonary shunting was evaluated by injecting technetium-99 m-labeled macroaggregated albumin (Tc-99MAA) into the target lobar artery.
Conventional TACE
TACE was performed during planning angiography for the tumor(s) in the lobe with small tumor burden. Iodized oil (Lipiodol; Andre Guerbet, Aulnay-sous-Bios, France) and doxorubicin hydrochloride (Adriamycin RDF; Ildong Pharmaceutical, Seoul, Korea) emulsions were infused selectively into tumor-feeding vessels. The doses of iodized oil and doxorubicin were determined according to tumor size. Additional embolization using gelatin sponge particles (Cali-gel; Hangzhou Alicon Pharm SCI&TEC, China) was performed for patients in whom the tumor-feeding artery was superselected (Fig. 1). By contrast, when TACE was performed at the lobar or segmental artery level, additional gelatin sponge particle embolization was not performed to prevent liver function deterioration.
68-year-old woman with hepatocellular carcinoma (HCC). A Gadolinium-enhanced MRI of the liver showing a large arterially enhancing heterogeneous mass (arrow) in the left hepatic lobe with a tumor thrombus in the left portal vein. An arterially enhancing small nodule (arrowhead) existed in the right lobe of the liver. B MRI of the kidneys shows multiple arterially enhancing nodular lesions (arrowheads) in the right lobe of the liver. C A large vascular mass existed in the left lobe of the liver supplied by the left hepatic artery and multiple small vascular lesions (arrows) in the right lobe. Conventional TACE (cTACE) was performed at the level of right hepatic artery with emulsions of Lipiodol (6 cc) and doxorubicin (30 mg) for the small tumors in the right lobe. D Celiac angiogram obtained before TARE demonstrates hypervascular mass in the left lobe and no residual tumor stains in the right hepatic lesions (arrows) after TACE. A total of 1.0 GBq of Y90 was administered to the left hepatic artery to treat the left lobar tumor. E Contrast-enhanced CT obtained one month after combined treatment with cTACE and TARE shows poor enhancement of the left hepatic tumor and Lipiodol retention in the non-enhancing lesions (arrow) in the right lobe of the liver
TARE
TARE was performed within 2 weeks of the planning angiography/chemoembolization for patients whose hepatic function reverted to baseline and those who had clinical symptoms after TACE. The administered dose was calculated using partition model [11, 13, 14]. The doses to the normal liver and the lung were adjusted so as not to exceed 70 and 25 Gy, respectively. The calculated dose of Y90 resin microsphere (SIR-Spheres; Sirtex Medical, Sydney, Australia) was injected in the feeding artery of the dominant tumor as selectively as possible (Fig. 1). After radioembolization, hepatic arteriography was performed to confirm that the entire tumor bed was treated.
Follow-Up Monitoring
To evaluate possible hepatic toxicity caused by TARE and TACE, the liver enzymes, including serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), and ALP, and serum total bilirubin levels were measured before and 3 days after TACE, and before, 3 days after and 1 month after TARE. Follow-up imaging was performed using liver dynamic CT or MRI at 1, 3, and 6 months and then annually after TARE to evaluate disease progression. Postprocedural adverse effects were classified according to severity using the NCI Common Terminology Criteria for Adverse Events (CTCAE) v.3.0.
Definitions and Statistical Analysis
Disease progression was defined using criteria form either the Modified Response Evaluation Criteria in Solid Tumor (mRECIST) or the European Association for the Study of Liver (EASL). REILD was defined as jaundice (total bilirubin > 3 mg/dL) and ascites and an increasing ALP level after TARE without tumor progression or bile duct dilatation [11]. A procedure-related adverse event was defined as a complication occurring within 1 month of treatment. Major complications were defined as grade 3 or higher according to CTCAE v.3.0.
Differences in liver enzymes before and after treatment were assessed via a paired t-test. Time-to-progression (TTP) and overall survival (OS) were calculated using the Kaplan–Meier method. SPSS 23.0 (SPSS, Chicago, IL) was used for data management and analysis.
Results
Baseline patient and tumor characteristics are shown in Table 1. Nineteen patients (13 men, 6 women; mean age 60 years; range 27–82 years) were included in this study. Among them, 17 patients had underlying hepatitis B, one had hepatitis C, and one had non-B, non-C HCC. Six patients were in BCLC-B stage, and 13 patients were in BCLC-C stage. Child–Pugh classifications were A in 14 patients and B in five patients.
All patients had a dominant tumor (mean size 105 mm; range 55–170 mm) in one hepatic lobe and small tumor nodule(s) in the other lobe. Portal vein tumor invasion was noted in seven cases (36.8%), right hepatic vein invasion in two (10.5%), and bile duct invasion in two (10.5%, right anterior duct in one and left superior duct in one).
The mean lung shunt fraction was 11.94% (range 2.12–26.3). During TARE, a mean of 2.8 GBq (range 1.0–3.5 GBq) of Y90 microspheres was administered. Eleven patients were infused with Y90 microspheres at the level of the lobar artery, two were infused at the segmental artery, and six patients were infused at the lobar and segmental arteries.
Conventional TACE was performed for a single nodule in 10 patients and for multiple nodules in nine patients. TACE was performed at the lobar artery in six patients and at the segmental artery in 13. The mean doses of doxorubicin and iodized oil were 24.5 mg and 5.2 mL, respectively. Eight patients underwent additional embolization using gelatin sponge particles. TACE for parasitic tumor supply through the right inferior phrenic artery was performed in four patients.
Results of the liver function tests and complications are shown in Table 2. The liver enzymes and serum total bilirubin significantly increased 3 days after TACE. However, before TARE, they reverted to baseline after conservative treatment. No significant elevation of liver enzymes was noted 3 days and 1 month after TARE. Total bilirubin level was increased 3 days after TARE and reverted to baseline after 1 month. No procedure-related major complications occurred. Sixteen patients (84.2%) had minor complications after TACE, namely, transient fever (n = 5), abdominal pain (n = 10), and nausea (n = 1). However, these symptoms improved within a few days after conservative treatment, and no subsequent delay of TARE schedule due to minor complications occurred. After TARE, two patients (10.5%) had minor complications (one with transient fever and one with nausea), which improved with conservative management.
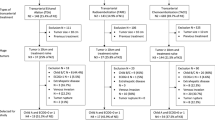
The median TTP of patients was 9.0 months (range 1–37 months). During follow-up, nine patients died, and the median OS was 28.0 months (range 3–39 months) (Fig. 2). Sixteen patients (84.2%) underwent subsequent treatment, namely, TACE (n = 7), TACE and resection (n = 2), systemic chemotherapy with sorafenib (n = 6), and radiofrequency ablation with palliative radiotherapy (n = 1), due to remained viable tumor, tumor progression, or recurrence. Three other patients (15.8%) had disease progression but could no longer be treated due to poor underlying condition.
Discussion
HCC is among the most common malignancies and is the leading cause of death among cirrhotic patients [1, 2]. Despite improvements in surveillance programs to detect HCC earlier, a significant proportion of patients are still diagnosed with unresectable HCC, including intermediate (BCLC-B) to advanced stage (BCLC-C) [3]. Intermediate stage is defined by multinodularity (more than three nodules) without portal invasion of extrahepatic metastasis in asymptomatic patients. Advanced stage includes patients with symptoms and/or invasive tumoral behavior, such as vascular invasion or extrahepatic metastasis [15].
TACE is the mainstay of treatment for HCC patients contraindicated for standard curative approaches, such as surgical resection or ablation therapy [4]. However, a high recurrence rate was noted in cases of bilobar, multiple, or large-sized (> 5 cm) lesions treated with TACE [16]. TACE is also contraindicated in patients with portal vein occlusion because of the increased risk of liver decompensation [4].
TARE, using microspheres loaded with Y90, involves an injection of short-range radioactive compounds into the hepatic artery, creating a microembolic effect without resulting in arterial occlusion [17, 18]. Because of this minimal embolic effect, TARE can be used in patients with portal vein thrombosis, and yields an acceptable treatment outcome, including a median survival of 13.8 months [6, 19, 20]. As such, TARE is an emerging alternative treatment to TACE in patients with intermediate and advanced HCC (BCLC-B/C) who have multinodular HCC or HCC with portal vein thrombosis [6, 7].
REILD is among the complications following TARE. It can result in significant morbidity and may become potentially life-threatening [21]. The incidence of REILD ranges from 0 to 4% [10, 21, 22]. One important risk factor of REILD is whole-liver treatment. [9, 10] Therefore, it should be avoided and replaced with superselective catheterization that reduces the risk of REILD [9].
Other risk factors for REILD include a tumor volume greater than 70% of the liver volume and/or a dose of ≥ 150 Gy administered to the whole liver [22]. In cases of multiple and bilobar HCC with a large tumor burden, multiple treatments should be performed sequentially, and the interval between treatments should be greater than 4-6 weeks to avoid potential liver toxicity [9, 12].
Although sequential treatment is generally recommended, this protocol has disadvantages. The tumor may progress during the lag period. Moreover, sequential treatments require additional hospital visits, resulting in high costs. To overcome these limitations, we performed TARE/TACE combination therapy within 2 weeks to treat bilobar HCC. Hepatic function tests revealed no significant hepatic toxicity after this combined treatment. Although hepatic function temporarily deteriorated after TACE, this was recovered before TARE and no schedule delay due to hepatic dysfunction occurred. We consider the reasons for this is as follows: (1) we performed selective TACE whenever possible; (2) gelatin sponge particle embolization was not performed when selective TACE was not possible; and (iii) the tumor burden of nondominant lobe was relatively small.
Radiation pneumonitis (RP) is also a major complication of TARE. It can result from deposition of microspheres in the lungs via excessive hepatopulmonary shunting [21, 23]. The risk of RP can increase in patients with hepatopulmonary shunt fraction (HPSF) > 13%, and guidelines for using resin microspheres recommend avoiding TARE treatment in patients with HPSF > 20% [23, 24]. Also, restricting radiation absorbed dose to the lungs to < 30 Gy in a single treatment or 50 Gy over a lifetime is recommended [25].
Several treatments have been recently reported to overcome RP in patients with high HPSF [23, 26]. In our study, two patients had high HPSF (23.21 and 26.3%). For the patient with HPSF of 23.21%, balloon occlusion of the right hepatic vein was performed to prevent the microsphere shunts to the lung. Meanwhile, in the other patient who had a high HPSF of 26.3%, the tumor-to-normal uptake ratio was high as 6.45, and the target lobe volume was small. In the partition model, the tumor dose was 147.02 Gy, and the lung dose was 13.06 Gy when 1 GBq was injected. Thus, the patient was routinely treated without additional procedures. No adverse effect, including RP, occurred in both patients.
Previous studies have been conducted to compare OS and TTP of TARE and TACE [17, 27,28,29,30,31,32]. In patients treated with TARE, the OS ranged from 6 to 20.5 months, whereas it ranged from 6 to 18 months in patients treated with TACE [17, 27,28,29,30,31,32]. Meanwhile, TTP ranged from 10 to 17.7 months for patients treated with TARE and from 6.8 to 8.4 months for patients treated with TACE [17, 31, 32]. In our study, the median OS was 28.0 months, and the median TTP was 9 months, indicating that our data are comparable with results from previous studies.
This study has some research limitations, including its retrospective design and the relatively small number of patients (n = 19). Another limitation is that all patients were treated using resin microspheres because glass microspheres are unavailable in our country. However, published data show comparable toxicity profiles and treatment outcomes for glass and resin microspheres following TARE treatment [33]. The third limitation is that 10 patients (52.6%) had a single lesion in the nondominant lobe, which means relatively small tumor burden. This can be a cause of the relatively good OS and TTP compared with previous studies. Finally, there is no comparative study of the clinical outcomes of TARE for bilobar HCC. Although our study showed better clinical outcomes compared to the TARE for intermediate/advanced HCC, further study for bilobar HCC is needed.
Our study demonstrates that combined radioembolization and chemoembolization can be a safe and effective treatment modality for bilobar HCC patients. In comparison with sequential treatment, additional benefits of the combined treatment include time and cost savings for both the community and the patients.
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365(12):1118–27.
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245–55.
Sangro B. Chemoembolization and radioembolization. Best Pract Res Clin Gastroenterol. 2014;28(5):909–19.
Di Marco V, De Vita F, Koskinas J, et al. Sorafenib: from literature to clinical practice. Ann Oncol. 2013;24(Suppl 2):ii30–7.
Cho YY, Lee M, Kim HC, et al. Radioembolization is a safe and effective treatment for hepatocellular carcinoma with portal vein thrombosis: a propensity score analysis. PLoS ONE. 2016;11(5):e0154986.
Rostambeigi N, Dekarske AS, Austin EE, et al. Cost effectiveness of radioembolization compared with conventional transarterial chemoembolization for treatment of hepatocellular carcinoma. J Vasc Interv Radiol. 2014;25(7):1075–84.
Lobo L, Yakoub D, Picado O, et al. Unresectable hepatocellular carcinoma: radioembolization versus chemoembolization: a systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2016;39(11):1580–8.
Gil-Alzugaray B, Chopitea A, Inarrairaegui M, et al. Prognostic factors and prevention of radioembolization-induced liver disease. Hepatology. 2013;57(3):1078–87.
Sangro B, Gil-Alzugaray B, Rodriguez J, et al. Liver disease induced by radioembolization of liver tumors: description and possible risk factors. Cancer. 2008;112(7):1538–46.
Denys A, Pracht M, Duran R, et al. How to prepare a patient for transarterial radioembolization? A practical guide. Cardiovasc Intervent Radiol. 2015;38(4):794–805.
Piana PM, Gonsalves CF, Sato T, et al. Toxicities after radioembolization with yttrium-90 SIR-spheres: incidence and contributing risk factors at a single center. J Vasc Interv Radiol. 2011;22(10):1373–9.
Kao YH, Tan EH, Ng CE, et al. Clinical implications of the body surface area method versus partition model dosimetry for yttrium-90 radioembolization using resin microspheres: a technical review. Ann Nucl Med. 2011;25(7):455–61.
Salem R, Thurston KG. Radioembolization with yttrium-90 microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies: part 3: comprehensive literature review and future direction. J Vasc Interv Radiol. 2006;17(10):1571–93.
Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19(3):329–38.
Kim DY, Ryu HJ, Choi JY, et al. Radiological response predicts survival following transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma. Aliment Pharmacol Ther. 2012;35(11):1343–50.
El Fouly A, Ertle J, El Dorry A, et al. In intermediate stage hepatocellular carcinoma: radioembolization with yttrium 90 or chemoembolization? Liver Int. 2015;35(2):627–35.
Salem R, Lewandowski RJ. Chemoembolization and radioembolization for hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2013;11(6):604–11 (quiz e43–4).
Sangiovanni A, Prati GM, Fasani P, et al. The natural history of compensated cirrhosis due to hepatitis C virus: a 17-year cohort study of 214 patients. Hepatology. 2006;43(6):1303–10.
Kulik LM, Carr BI, Mulcahy MF, et al. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology. 2008;47(1):71–81.
Riaz A, Lewandowski RJ, Kulik LM, et al. Complications following radioembolization with yttrium-90 microspheres: a comprehensive literature review. J Vasc Interv Radiol. 2009;20(9):1121–30 (quiz 1131).
Kennedy AS, McNeillie P, Dezarn WA, et al. Treatment parameters and outcome in 680 treatments of internal radiation with resin 90Y-microspheres for unresectable hepatic tumors. Int J Radiat Oncol Biol Phys. 2009;74(5):1494–500.
Ward TJ, Tamrazi A, Lam MG, et al. Management of high hepatopulmonary shunting in patients undergoing hepatic radioembolization. J Vasc Interv Radiol. 2015;26(12):1751–60.
Leung TW, Lau WY, Ho SK, et al. Radiation pneumonitis after selective internal radiation treatment with intraarterial 90yttrium-microspheres for inoperable hepatic tumors. Int J Radiat Oncol Biol Phys. 1995;33(4):919–24.
Ho S, Lau WY, Leung TW, et al. Clinical evaluation of the partition model for estimating radiation doses from yttrium-90 microspheres in the treatment of hepatic cancer. Eur J Nucl Med. 1997;24(3):293–8.
Bester L, Salem R. Reduction of arteriohepatovenous shunting by temporary balloon occlusion in patients undergoing radioembolization. J Vasc Interv Radiol. 2007;18(10):1310–4.
Moreno-Luna LE, Yang JD, Sanchez W, et al. Efficacy and safety of transarterial radioembolization versus chemoembolization in patients with hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2013;36(3):714–23.
Kolligs FT, Bilbao JI, Jakobs T, et al. Pilot randomized trial of selective internal radiation therapy vs. chemoembolization in unresectable hepatocellular carcinoma. Liver Int. 2015;35(6):1715–21.
Kooby DA, Egnatashvili V, Srinivasan S, et al. Comparison of yttrium-90 radioembolization and transcatheter arterial chemoembolization for the treatment of unresectable hepatocellular carcinoma. J Vasc Interv Radiol. 2010;21(2):224–30.
Carr BI, Kondragunta V, Buch SC, et al. Therapeutic equivalence in survival for hepatic arterial chemoembolization and yttrium 90 microsphere treatments in unresectable hepatocellular carcinoma: a two-cohort study. Cancer. 2010;116(5):1305–14.
Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140(2):497–507 (e2).
Hilgard P, Hamami M, Fouly AE, et al. Radioembolization with yttrium-90 glass microspheres in hepatocellular carcinoma: European experience on safety and long-term survival. Hepatology. 2010;52(5):1741–9.
Bhangoo MS, Karnani DR, Hein PN, et al. Radioembolization with yttrium-90 microspheres for patients with unresectable hepatocellular carcinoma. J Gastrointest Oncol. 2015;6(5):469–78.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts to report.
Ethical Approval
For this type of study formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kwon, J.H., Kim, G.M., Han, K. et al. Safety and Efficacy of Transarterial Radioembolization Combined with Chemoembolization for Bilobar Hepatocellular Carcinoma: A Single-Center Retrospective Study. Cardiovasc Intervent Radiol 41, 459–465 (2018). https://doi.org/10.1007/s00270-017-1826-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1826-7