Abstract
Background
Postoperative cholangitis is a common complication of pancreaticoduodenectomy. Frequent cholangitis impairs patients’ quality of life after pancreaticoduodenectomy. However, the risk factors for recurrence of cholangitis remain unclear. Hence, this retrospective study aimed to identify risk factors for recurrence of cholangitis after pancreaticoduodenectomy.
Methods
The medical records of patients who underwent pancreaticoduodenectomy between 2015 and 2019 in our institution were retrospectively reviewed. At least two episodes of cholangitis a year after pancreaticoduodenectomy were defined as ‘recurrence of cholangitis’ in the present study. Univariate and multivariate analyses were performed.
Results
The recurrence of cholangitis occurred in 40 of 207 patients (19.3%). Multivariate analysis revealed that internal stent (external, RR: 2.16, P = 0.026; none, RR: 4.76, P = 0.011), firm pancreas (RR: 2.61, P = 0.021), constipation (RR: 3.49, P = 0.008), and postoperative total bilirubin>1.7 mg/dL (RR: 2.94, P = 0.006) were risk factors of recurrence of cholangitis. Among patients with internal stents (n = 54), those with remnant stents beyond 5 months had more frequent recurrence of cholangitis (≥5 months, 75%; <5 months, 30%).
Conclusions
Internal stents, firm pancreas, constipation, and postoperative high bilirubin levels are risk factors for cholangitis recurrence after pancreaticoduodenectomy. In addition, the long-term implantation of internal stents may trigger cholangitis recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreaticoduodenectomy (PD) is a common surgical procedure for periampullary disease with various postoperative complications. Early postoperative complications, such as pancreatic fistula and delayed gastric emptying, have been well investigated, leading to a decrease of their incidence in recent decades [1]. In contrast, cholangitis can occur at any time during the postoperative course and remains a common complication. Furthermore, some patients experience not only a single episode of cholangitis but also multiple subsequent episodes. Even if not severe, frequent cholangitis may lead to repeated hospitalization, increased healthcare costs, and impaired quality of life. Moreover, in cancer patients, frequent cholangitis may interfere with adjuvant chemotherapy or treatment for recurrence, potentially affecting patient prognosis. Although a few studies have shown the incidence of cholangitis after PD and its risk factors [2, 3], the characteristics and risk factors of repeated cholangitis remain unclear.
In the present study, recurrence of cholangitis was defined as repeated episodes of cholangitis that occurred at least twice within 1 year. We retrospectively investigated the risk factors and clinical features for recurrence of cholangitis after PD.
Material and methods
Patients
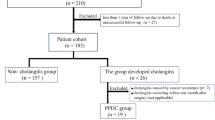
The medical records of patients who underwent PD at Kobe University Hospital between January 2015 and December 2019 (n = 244) were retrospectively reviewed. Patients who discontinued follow-up within 1 year after surgery (n = 34), those who underwent prior hepaticojejunostomy (n = 2) and had other malignancies (n = 1) were excluded. Ultimately, 207 patients were included in the analysis. Data on preoperative patient characteristics, surgical findings, and postoperative course were retrospectively collected. In addition, the highest laboratory test values within 7 days after PD were collected.
This study was conducted in accordance with the principles of the Declaration of Helsinki. Institutional review board certification for this study was obtained from Kobe University Hospital (B220039).
Preoperative management
Preoperative biliary drainage was performed when jaundice was apparent. Endoscopic biliary stenting using a plastic tube was the first choice if appropriate. When preoperative cholangitis was present, antibiotic chemotherapy was additionally administered to improve the septic condition before surgery. In general, surgery was performed after the serum total bilirubin level decreased to < 3 mg/dL.
Surgical procedure
Most patients underwent subtotal stomach-preserving PD, and reconstruction was performed using the modified Child method without Braun anastomosis. Pancreaticojejunostomy was performed using a modified Blumgart method. Hepaticojejunostomy was performed with a single-layer interrupted suture using an absorbable 5–0 thread. Bile ducts were transected above the cystic duct regardless of disease. During hepaticojejunostomy, the bile duct’s diameter was routinely measured. Stenting requirements and types of stents for hepaticojejunostomy were planned as preferred by the surgeon in each case. A 2.5 mm polyethylene tube was placed through the hepaticojejunostomy and positioned 2–3 cm into the bile duct as an external or internal stent. One end of the tube was pierced through the jejunum to the outside of the abdominal cavity in the external stent group, whereas the other end was placed in the distal intestine of the hepaticojejunostomy in the internal stent group. The stent was anchored to the middle of the posterior wall by absorbable sutures. External biliary stents were routinely removed within 1–2 months postoperatively. Gastrojejunostomy was performed 40 cm downstream from the hepaticojejunostomy and side-to-side anastomosed at the antecolic pathway.
Postoperative complications
Postoperative pancreatic fistula was diagnosed according to the International Study Group on Pancreatic Fistula guidelines [4]. In addition, postpancreatectomy hemorrhage was diagnosed according to the International Study Group of Pancreatic Surgery guidelines [5]. Bile leakage was diagnosed according to the International Study Group on Liver Surgery guidelines [6]. These complications were clinically relevant if they were classified as grade B or C of severity. Postoperative constipation was assessed at discharge or postoperative outpatient according to the Common Terminology Criteria for Adverse Events Ver 5.0. Patients with grade 2 (laxative use) or higher were recorded as having constipation.
Routine follow-up protocol after hospital discharge
All patients underwent follow-up computed tomography (CT) every 3 months postoperatively for 2 years and every 6 months. Some patients underwent additional CT scans when necessary. Follow-up CT was routinely contrast-enhanced in patients without renal dysfunction or allergy. All CT scans were reviewed for the present study and checked for pneumobilia, hepatolithiasis, and remnant internal biliary stents. The interval from surgery to the last follow-up CT in which the remnant internal biliary stent was present at the hepaticojejunostomy site was defined as the remaining time of the stent.
Definition of cholangitis
Cholangitis was diagnosed based on the 2018 Tokyo Guidelines (TG18) diagnostic criteria [7]. In the TG18, diagnosis of acute cholangitis consists of three categories: systemic inflammation (A), cholestasis (B), and imaging (C). Each has two items as follows: A-1, fever and/or shaking chills; A-2 laboratory data: evidence of inflammatory response; B-1 Jaundic; B-2 Laboratory data: abnormal liver function tests; C-1 Biliary dilation; C-2 Evidence of the etiology on imaging (stricture, stone, and stent, among others). A definite diagnosis is the presence of one item in A, one in B, and one in C; a suspected diagnosis is the presence of one item in A and one in either B or C.
Cholangitis was defined in the present study when the criteria for either a suspected or definite diagnosis based on the TG18 were met. Furthermore, patients with cholangitis included both those who were hospitalized and those who received only outpatient treatment. Recurrence of cholangitis was defined in the present study as repeated episodes of cholangitis at least twice a year, regardless of the period after PD. All patients with cholangitis in this study underwent CT scans, and endoscopic observation of the hepaticojejunostomy was performed in cases where biliary strictures were suspected. Any other possible inflammatory findings on CT scans were ruled out. Patients with cholangitis due to tumor recurrence (malignant stricture) or afferent loop syndrome were not recorded as having cholangitis.
Statistical analyses
Continuous data were expressed as median (range) and compared for cholangitis using logistic regression analysis. Categorical variables were compared using the chi-squared or Fisher’s exact tests, as appropriate. Variables with a P-value of < 0.05 in the univariate analysis were included in the multivariate analysis. The multivariate analysis was performed using a logistic regression model. Continuous variables that were significant in univariate analysis were divided into two values for multivariate analysis based on ROC (Receiver Operating Characteristic) analysis. Statistical significance was set at P < 0.05, and statistical analyses were performed using the JMP Pro 15.1.0 software (SAS Institute Inc., USA).
Results
Patients’ characteristics
The clinical characteristics of the patients who underwent PD are shown in Table 1 and Supplementary Table 1. In total, 207 patients (123 male and 84 female) with a median age of 68 (range: 27–89) years were analyzed. Indications for PD were pancreatic ductal adenocarcinoma (n = 111, 53.6%), ampullary carcinoma (n = 30, 14.4%), intraductal papillary mucinous neoplasm (n = 26, 12.5%), cholangiocarcinoma (n = 21, 10.1%), neuroendocrine tumor (n = 12, 5.8%), and other benign disease. Malignancy was defined as pancreatic cancer, bile duct cancer, or papillary carcinoma. Preoperative biliary drainage was performed in 106 (51.2%) patients. The median follow-up duration was 32 (range: 12–80) months.
Incidence of recurrence of cholangitis
Postoperative cholangitis developed in 87 patients (43%), of whom 40 (45.9%) experienced recurrence of cholangitis. Four patients (10%) with recurrence of cholangitis had benign biliary strictures diagnosed by endoscopy. The median maximum number of episodes in a year was three (range: 2–7). Eighteen patients had episodes twice a year, and 22 patients had more than three episodes per year.
Factors associated with recurrence of cholangitis
Table 1 shows the results of the univariate analysis of the incidence of recurrence of cholangitis. The univariate analysis showed that a firm pancreas (risk ratio (RR): 2.34; 95% confidence interval (CI) 1.093–5.008; P = 0.025), internal stent use during hepaticojejunostomy (P = 0.009), postoperative total bilirubin (RR: 3.07; 95% CI 1.506–6.269; P = 0.013), and constipation (OR: 2.59; 95% CI 1.09–6.13; P = 0.025) were significantly associated with the incidence of recurrence of cholangitis. The two groups had no significant differences in bile duct diameter, preoperative biliary drainage, pancreatic fistula, or pneumobilia. Given that internal stent placement was risk factor for recurrence of cholangitis, the characteristics of patient with each stent was analyzed (Table 2). Preoperative biliary drainage and operative bile duct diameter that showed significant differences in the characteristics of each stent were also included in the multivariate analysis. The multivariate analysis showed that a firm pancreas (RR: 3.10; 95% CI 1.298–7.427; P = 0.011), internal stent (/external stent RR: 2.52; 95% CI 1.012–6.296; P = 0.047, /none RR: 5.47; 95% CI 1.303–22.99; P = 0.020), constipation (RR: 3.75; 95% CI 1.41–9.99; P = 0.008), and postoperative total bilirubin > 1.7 mg/dL (RR: 3.18; 95% CI 1.405–7.229; P = 0.006) were independently associated with recurrence of cholangitis (Table 3).
Biliary stent analysis
Biliary stents were used in 160 patients during hepaticojejunostomy (external stent, n = 103; internal stent, n = 57). The characteristics of patients with internal biliary stents were compared with those of patients with external stents and those with no stents (Table 2). Patients with internal stents had smaller intraoperative bile duct diameters and lower preoperative biliary drainage rates compared to those with external stents and no stents. In patients with narrow bile duct diameters (< 8 mm, n = 33), recurrence of cholangitis tended to occur more frequently in internal stents (no stent, 0/1; internal stent, 7/20; external stent, 2/12). Given that internal stent placement was an independent risk factor for recurrence of cholangitis, the relationship between the duration of the remnant internal stent and cholangitis was analyzed. In 47 of the 54 patients with internal stents, follow-up CT scans revealed removal of stents at the anastomosis site. Figure 1 shows the cumulative incidence rate of internal stents removed at the anastomosis site; the incidence rate was 50% at 5 months. The median time from PD to the first cholangitis in patients with internal stents was 4 months. Among patients with internal stents, those with remnant stents for longer than 5 months were found to have a more frequent recurrence of cholangitis (≥5 months, 75%; <5 months, 30%).
Discussion
The present study demonstrated that 42.0% of patients who underwent PD experienced cholangitis, and 45.9% (19.3% of the total number of patients) developed recurrence of cholangitis after PD. In addition, internal stent placement during hepaticojejunostomy, a firm pancreas, constipation, and postoperative total bilirubin > 1.7 mg/dL were independently associated with postoperative recurrence of cholangitis. Of note, an internal stent remaining at the anastomosis site for > 5 months was found to be a risk factor for recurrence of cholangitis. To the best of our knowledge, this is the first study to reveal an association between biliary stenting during hepaticojejunostomy and recurrence of cholangitis after PD.
Biliary stent during hepaticojejunostomy is assumed to prevent anastomotic stenosis and bile leakage [8]. There are two types of stents, external and internal, which are used at the discretion of institutions and surgeons. External stents can show stent occlusion and allow for control of the timing of stent removal; however, they have risks of accidental removal or kinking, loss of bile, and stress to the patient because the stent is outside the body. Internal stents are less stressful to the patient. However, there is no method for surgeons to detect stent occlusion and control the timing of stent removal in patients with internal stents. In the present study, patients with internal stents had significantly more recurrence of cholangitis than others. Suspecting selection bias, bile duct diameters and preoperative drainage with different backgrounds for each stent in Table 2 were included in the multivariate analysis; however, internal stent remained a significant factor. In patients with a narrow bile duct diameter (< 8 mm), recurrence of cholangitis tended to occur more frequently in patients with internal stents than in those with external stents and no stents. In treating obstructive jaundice, long-term plastic stent placement causes stent occlusion and stent-stone complex formation, the sequelae of which increase the incidence of cholangitis [9, 10]. Similar mechanisms might have contributed to the increased incidence of cholangitis in patients with internal stents during hepaticojejunostomy. While external stents are usually removed within 2 months after PD, half of the internal stents remain at the site of hepaticojejunostomy for longer than that. In addition, there were two patients with remaining internal stents at the anastomosis site beyond 2 years and one patient beyond 3 years. There were three patients who required additional endoscopic intervention to remove the internal stent due to hepatolithiasis at the anastomosis. The longitudinal placement of internal stents may increase recurrence of cholangitis because internal stents remaining at the site of anastomosis for > 5 months was a risk factor for recurrence of cholangitis in the present study. The present study showed no benefit of stents during hepaticojejunostomy compared to no stent, and a high rate of recurrence of cholangitis with internal stents. Therefore, the use of internal stents during hepaticojejunostomy should be avoided.
In the present study, a firm pancreas and constipation were risk factors for recurrence of cholangitis. A firm pancreas may include chronic pancreatitis associated with exocrine insufficiency. The prevalence of bacteria in the gastrointestinal tract has been reported to depend on its pH [11]. Patients with pancreatic exocrine insufficiency are known to have a high incidence of small intestinal bacterial overgrowth and an increase in the Firmicutes: Bacteroidetes ratio due to a decreased gastric acid-neutralizing function [12, 13]. Changes in the intestinal microbiota might have increased the retrograde infection of the bile ducts. Since the present study did not examine the pathogenesis of cholangitis, further investigations are needed to reveal an association between cholangitis, intestinal bacteria, and a firm pancreas. Constipation is associated with gut motility. There has been increasing research regarding the importance of gastrointestinal microbiota in gut function and the effect of probiotics on gut motility and constipation [12]. It has been reported that patients with constipation have abnormal upper gut motility, including the small intestine [13]. A possible explanation is that intestinal dysmotility contributes to intestinal stagnation and bile reflux, thereby increasing the recurrence of cholangitis.
High bilirubin levels after PD are also significantly associated with recurrence of cholangitis in the present study. High postoperative bilirubin levels might reflect temporary functional cholestasis and be predictive for the recurrence of cholangitis; however, the mechanism is unclear because many factors may have influenced the laboratory data.
Previous studies reported several risk factors for cholangitis after PD: an alkaline phosphatase level ≥ 410 IU/L, a small ratio of the postoperative bile duct diameter to the preoperative bile duct diameter, benign disease, long operation time, elevated C-reactive protein, and the presence of pneumobilia [2, 3, 14]. The risk factors identified in these previous studies were not significantly associated with recurrence of cholangitis in the present study. This difference could be explained by the patients’ backgrounds. First, the studies mentioned above included a single episode of cholangitis. Moreover, internal stent placement, constipation, and postoperative high bilirubin levels were not identified as risk factors for patients with a single episode, but only in those with recurrence of cholangitis in this study’s cohort (data not shown). Second, 25–50% of the cholangitis cases in the mentioned studies had postoperative biliary strictures. In contrast, in the present study, four of the forty patients had biliary strictures. Considering the small number of cases of strictures, the impact of biliary structures on the recurrence of cholangitis is probably limited. Running sutures during hepaticojejunostomy have been reported to be a risk factor for biliary strictures after PD [15]. In our institution, biliary strictures could be prevented caused by interrupted suturing and the use of biliary stents for hepaticojejunostomy. Finally, previous studies [2, 3, 14] included 130–160 patients, which are smaller sample sizes compared to that of the present study.
This study had several limitations. First, there was some unavoidable bias because this study was conducted retrospectively; the selection of stents was performed at the discretion of the individual surgeon, which might have impacted baseline characteristics. However, as mentioned above, our multivariate analysis showed that the internal stent was an independent risk factor for the recurrence of cholangitis even after adjusting for operative bile duct diameter. Second, there was uncertainty regarding the diagnosis of cholangitis. Postoperative cholangitis was diagnosed based on the TG18 criteria, including suspected diagnoses, because it was difficult to identify the etiology of postoperative cholangitis without biliary dilatation or stricture with imaging. However, suspected diagnoses might have included postoperative inflammation, fever during chemotherapy, and other conditions that are different from cholangitis. On the other hand, some patients with cholangitis may have been missed because they did not visit our hospital at the onset.
In conclusion, internal stents, a firm pancreas, constipation, and high postoperative bilirubin levels were found to be risk factors for the recurrence of cholangitis after PD. In addition, internal stents which remain at the hepaticojejunostomy site for several months may trigger recurrence of cholangitis. The surgeon's choice of stent type (no-stent or external stent) has the potential to reduce postoperative cholangitis.
References
Gouma DJ, van Geenen RC, van Gulik TM et al (2000) Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg 232:786–795
Ito Y, Abe Y, Kitago M et al (2018) Predictive factors of late cholangitis in patients undergoing pancreaticoduodenectomy. World J Surg Oncol 16:19
Hiyoshi M, Wada T, Tsuchimochi Y et al (2016) Hepaticoplasty prevents cholangitis after pancreaticoduodenectomy in patients with small bile ducts. Int J Surg 35:7–12
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591
Rahbari NN, Garden OJ, Padbury R et al (2011) Post-hepatectomy haemorrhage: a definition and grading by the International study group of liver surgery (ISGLS). HPB (Oxford) 13:528–535
Koch M, Garden OJ, Padbury R et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International study group of liver surgery. Surgery 149:680–688
Kiriyama S, Kozaka K, Takada T et al (2018) Tokyo guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci 25:17–30
Fuyo Y, Hisayuki O, Yuji A et al (1996) Internal Stenting of the hepaticojejunostomy and pancreaticojejunostomy in patients undergoing pancreatoduodenectomy to promote ealier discharge discharge from hospital. Surg Today 26:665–667
Tang SJ, Armstrong L, Lara LF et al (2007) De novo stent-stone complex after long-term biliary stent placement: pathogenesis, diagnosis, and endotherapy. Gastrointest Endosc 66:193–200
Kaneko J, Kawata K, Watanabe S et al (2018) Clinical characteristics and risk factors for stent-stone complex formation following biliary plastic stent placement in patients with common bile duct stones. J Hepatobiliary Pancreat Sci 25:448–454
Hao WL, Lee YK (2004) Microflora of the gastrointestinal tract: a review. Methods Mol Biol 268:491–502
Dimidi E, Christodoulides S, Scott SM et al (2017) Mechanisms of action of probiotics and the gastrointestinal microbiota on gut motility and constipation. Adv Nutr 8:484–494
Bassotti G, Stanghellini V, Chiarioni G et al (1996) Upper gastrointestinal motor activity in patients with slow-transit constipation. Further evidence for an enteric neuropathy. Dig Dis Sci 41:1999–2005
Ueda H, Ban D, Kudo A et al (2017) Refractory long-term cholangitis after pancreaticoduodenectomy: a retrospective study. World J Surg 41:1882–1889
Yamaki S, Satoi S, Yamamoto T et al (2022) Risk factors and treatment strategy for clinical hepaticojejunostomy stenosis defined with intrahepatic bile duct dilatation after pancreaticoduodenectomy: a retrospective study. J hepatobiliary Pancreat Sci 29:1204–1213
Funding
This research did not receive any specific funding from any agencies in the public, commercial, or not-for-profit areas.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fukuoka, H., Toyama, H., Mizumoto, T. et al. Risk Factors for Recurrence of Cholangitis After Pancreaticoduodenectomy and Comparison of Stents in Hepaticojejunostomy. World J Surg 47, 2499–2506 (2023). https://doi.org/10.1007/s00268-023-07104-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07104-3