Abstract
Background
The objectives of this study were to emphasize the importance of preoperative laryngeal examination before thyroidectomy by investigating the incidence of coincident abnormal laryngeal conditions that impair the quality of voice, and evaluate the usefulness of the “thyroidectomy-related voice questionnaire” as a screening tool.
Methods
Five hundred consecutive patients scheduled to undergo thyroidectomy underwent preoperative laryngeal examination and voice analysis and completed the questionnaire. According to the laryngeal examination results, patients were classified into normal and abnormal groups. Acoustic-analysis results and questionnaire scores were compared between the two groups, and correlations between acoustic parameters and questionnaire scores were evaluated. The cutoff score of the questionnaire that can effectively discriminate between the two groups was also determined.
Results
The incidence of abnormal laryngeal conditions was 35.8%. The most common finding was laryngopharyngeal reflux (27.2%) followed by vocal nodule (4.8%), vocal polyp (1.8%), vocal cord palsy (1.2%), Reinke’s edema (0.4%), vocal cyst (0.2%), and vocal sulcus (0.2%). The perceptual grade of voice quality (0.33 ± 0.49 for normal group vs. 0.65 ± 0.62 for abnormal group, P = 0.000) and the questionnaire scores (3.21 ± 5.47 for normal group vs. 13.41 ± 11.67 for abnormal group, P = 0.000) of the two groups were significantly different, and there was a significant correlation between objective voice parameters and questionnaire scores. A questionnaire score of 5 showed the best sensitivity (74%) and specificity (71%) in discriminating between the two groups.
Conclusions
The incidence of coincident abnormal laryngeal conditions is relatively high; therefore, voice screening before thyroidectomy is important. The “thyroidectomy-related voice questionnaire” is a simple and effective screening tool to detect preexisting laryngeal disorders that can affect the quality of voice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroidectomy is a frequently used surgical procedure for the treatment of thyroid diseases. According to one study, an estimated 75,000–80,000 thyroid operations are performed yearly in the United States, making it one of the most commonly performed procedures [1]. One of the most prominent and feared complications of thyroid surgery is vocal dysfunction. Recurrent laryngeal nerve (RLN) injuries are traditionally considered to be the main cause of postoperative voice alterations, and their prevalence is reportedly 0.77% [2] to 13.3% [3]. However, besides RLN injuries, many other causes of postoperative voice alterations, such as operative injury of the external branch of the superior laryngeal nerve (EBSLN), or pitch control alterations caused by dysfunction of the prethyroid strap muscles, have been described [4, 5].
However, all of these studies focused on voice alterations after thyroidectomy. Preoperative voice assessment has recently been emphasized, and several authors insisted that laryngeal examination should be routinely performed before thyroidectomy [6]. Many studies document a low but significant number of patients undergoing surgery (even with benign disease) with preoperative vocal cord palsy [7]. Other than voice impairment caused by vocal cord palsy, many other abnormal laryngeal conditions unrelated to thyroid pathology can cause voice impairments, and such voice impairments not detected preoperatively will likely be considered to result from the ensuing thyroidectomy on postoperative review. Additionally, these preoperatively detected laryngeal disorders can be treated by their respective surgeries simultaneously with thyroidectomy thus avoiding another general anesthesia. In this sense, routine preoperative laryngeal examinations are important for screening for abnormal laryngeal conditions that can affect the quality of voice before thyroidectomy. Laryngoscopy or videostroboscopy is a relatively easy and effective procedure for the examination of the larynx. However, considering its discomfort and cost, it is difficult to perform this procedure routinely on all patients.
In the present study, we performed laryngeal examinations and voice analysis in all patients scheduled to undergo thyroidectomy and evaluated the prevalence and types of coincident abnormal laryngeal conditions. We also invented a simple questionnaire, the “thyroidectomy-related voice questionnaire,” and evaluated its usefulness as a prethyroidectomy screening tool. Based on the results of this study, we conclude that whenever a routine laryngeal examination is not available, thyroid surgeons will be able to effectively screen patients who require closer laryngeal examinations and voice analysis.
Materials and methods
Study design
The study group consisted of 500 patients scheduled to undergo thyroidectomy at the Department of Surgery and who were referred to the Department of Otolaryngology-Head and Neck Surgery for preoperative laryngeal and voice examinations between March 2010 and January 2011. Subjects were excluded if they had a history of head and neck surgery (including prior thyroid surgery) and if they had a greater than 1 month history of other disorders or conditions that may have affected their voice quality at the time of the examination, such as sinusitis, allergic rhinitis, or recent upper respiratory infection. Patients included 88 males and 412 females. Ages ranged from 16 to 76 years (mean = 45.52 ± 11.97 years). All subjects underwent fiber-optic laryngoscopy, videostroboscopy, perceptual voice analysis, and computerized acoustic analysis, and all were asked to complete the thyroidectomy-related voice questionnaire. The types and prevalence of abnormal laryngeal conditions were evaluated according to the flexible laryngoscopic and stroboscopic findings, and patients were classified into “normal” and “abnormal” groups. The questionnaire scores and parameters of perceptual and acoustic analyses were compared between the two groups. To evaluate whether there was any correlation between objective voice analysis results and subjective questionnaire scores, we investigated the relationships between voice parameters and questionnaire scores. Additionally, to determine the cutoff score that can effectively distinguish between normal and abnormal groups, sensitivity and specificity were analyzed according to the questionnaire score. The institutional review board of our institution approved the present study.
Fiber-optic laryngoscopic and videostroboscopic examinations
Using fiber-optic laryngoscopy (Machida Instruments, Tokyo, Japan) and videolaryngostroboscopy (model 9200C, KayPENTAX, Lincoln Park, NJ), we examined the entire larynx, including the mucosal status and the presence of vocal-fold diseases. The presence of laryngopharyngeal reflux (LPR) was examined using the reflux finding score (RFS). The RFS is an eight-item clinical severity scale based on findings during fiber-optic laryngoscopy. The eight items are subglottic edema, ventricular obliteration, erythema/hyperemia, vocal-fold edema, diffuse laryngeal edema, posterior commissure hypertrophy, granuloma/granulation tissue, and thick endolaryngeal mucus. The scale ranges from 0 (no abnormality) to a maximum of 26 (worst score possible). The RFS score was determined by two otolaryngologists by consensus, and patients with RFS scores of >7 were considered to have LPR [8].
Thyroidectomy-related voice questionnaire
This questionnaire was developed at our institution and is a self-assessment tool that measures quality of voice (Table 1). It consists of 20 questions; responses to each are scored from a minimum of 0 (no voice alterations or symptoms) to a maximum of 80 (highest voice impairment and multiple vocal symptoms). This questionnaire was developed based on the voice handicap index (VHI) and other studies on subjective symptoms related to thyroidectomy [9, 10]. The questions concern general voice complaints, representative symptoms related to LPR and vocal cord palsy, and swallowing-related symptoms associated with thyroidectomy.
Perceptual voice analysis
Voice samples were recorded for all patients. They were instructed to read “Sanchaek (a walk)” at a comfortable volume and rate. Each patient’s voice was also evaluated perceptually during a conversation. The patients provided information on their voice history and social history. A GRBAS (grade, roughness, breathiness, asthenia, strain) score was given at the end of the evaluation session. The recorded audiotapes of “Sanchaek (a walk)” were then replayed after the evaluation session to reconsider the GRBAS scores. Any variation in the GRBAS scores between reading and conversation were considered, and preference was given to the scores obtained during conversation. The voice was scored using the five GRBAS parameters: grade = overall degree of deviance of voice, roughness = irregular fluctuation of the fundamental frequency, breathiness = turbulent noise produced by air leakage, asthenia = overall weakness of the voice, and strain = impression of tenseness or excess effort. Each parameter was scored on a scale of 0 to 3 (0, normal; 1, slight disturbance; 2, moderate disturbance; and 3, severe disturbance). The voices were judged by two speech therapists and one otolaryngologist by consensus.
Acoustic analysis
Patients were instructed to produce the vowel “a” at a comfortable volume and constant pitch. Each vowel pronunciation was recorded with a constant mouth-to-microphone distance of 5 cm using Computerized Speech Lab (CSL model 4150, KayPENTAX, Lincoln Park, NJ). All digital recordings were made in a quiet room. Each patient sustained an “a” for at least 3 s at a comfortable pitch level. The task was repeated four times or more, and the fourth trial was often the recorded sample. Each analysis was made by a multidimensional voice program (MDVP model 5105, ver. 3.1.7; KayPENTAX). The parameters considered in the analysis were fundamental frequency (F o), perturbations of fundamental frequency (jitter), amplitude (shimmer), glottal noise (i.e., the noise-to-harmonic ratio), and speaking fundamental frequency (SFF).
Statistical analysis
Statistical analyses were performed using SPSS software ver. 15.0 for Windows (SPSS, Inc., Chicago, IL). Data from the two patient groups were statistically compared using Student’s t-test, and the relationship between the voice parameters and questionnaire score was tested using Spearman’s correlation coefficient (rho). A P value of <0.05 was considered statistically significant. The questionnaire cutoff score for detecting abnormal laryngeal conditions was determined by calculating the sensitivity and specificity of each score; the score with the best sensitivity and specificity was considered the cutoff score.
Results
On videostroboscopic examination, 321 patients (64.2%) showed normal findings and 179 patients (35.8%) showed abnormal findings. Abnormal findings were as follows: LPR in 136 patients (27.2%), vocal nodule in 24 patients (4.8%), vocal polyp in 9 patients (1.8%), vocal cord palsy in 6 patients (1.2%), Reinke’s edema in 2 patients (0.4%), vocal cyst in 1 patient (0.2%), and vocal sulcus in 1 patient (0.2%) (Table 2).
The perceptual and acoustic analyses results and the questionnaire scores were compared between normal and abnormal groups. Among the parameters of acoustic analysis, F o and SFF were analyzed according to the patients’ sex because the normal values of these parameters differ between male and female patients. The questionnaire scores were statistically significantly different between the two groups (0.33 ± 0.49 for normal group vs. 0.65 ± 0.62 for abnormal group, P = 0.000). G (grade) of perceptual analysis also showed statistically significant differences between the two groups (3.21 ± 5.47 for normal group vs. 13.41 ± 11.67 for abnormal group, P = 0.000). Among the acoustic parameters, only F o of female patients was significantly different between groups (204.87 ± 20.58 for normal group vs. 199.31 ± 27.67 for abnormal group, P = 0.029) (Table 3).
The analysis of the relationship between questionnaire scores and voice analysis parameters revealed that the perceptual parameter G and acoustic parameters were closely related. Moreover, the subjective questionnaire score showed a correlation with shimmer and G, with G showing a statistically significant correlation with the questionnaire score (r = 0.260, P < 0.05) (Table 4).
To determine the questionnaire cutoff score that could effectively distinguish between normal and abnormal groups, the sensitivity and specificity of each score in detecting abnormal laryngeal conditions were evaluated. The score with the best simultaneous sensitivity and specificity would be the score that distinguished between normal and abnormal groups; a score of 5 was found to be the best score that could effectively screen for the presence of abnormal laryngeal conditions (sensitivity of 73% and specificity of 71%) (Table 5).
Six patients had vocal cord palsy before the surgery. Retrospective chart review showed that all six patients underwent total thyroidectomy for the treatment of papillary thyroid cancer. Of these six patients, five had vocal cord palsy on the same side as the thyroid cancer, and operative findings showed that their RLNs were directly invaded by the cancerous mass; therefore, the RLNs were sacrificed during thyroidectomy. One patient had vocal cord palsy on the side opposite the thyroid cancer and was finally diagnosed with idiopathic vocal cord palsy. The questionnaire scores of the former five patients ranged from 15 to 50 (mean = 29.2), which is much higher than the score of 5 designated as the cutoff score for detecting abnormal laryngeal conditions in preoperative screening. The patient with idiopathic vocal cord palsy had a questionnaire score of 6, which was also higher than the cutoff score. Therefore, every patient with vocal cord palsy was effectively detected preoperatively with the questionnaire.
The coincident laryngeal disorders of the patients in the abnormal group were treated during or just after thyroidectomy. The disorders requiring surgical treatment, such as vocal polyp, vocal cysts, and Reinke’s edema, were cured with simultaneous microlaryngeal surgery and thyroidectomy. Microlaryngeal surgery was performed prior to thyroidectomy by the otolaryngologist and took an average of 10 min, with no complications and it did not interfere with the thyroidectomy. Other disorders that required medical treatment were managed just after thyroidectomy. Vocal nodules were treated with voice therapy, and LPR was treated with the standard protocol, including proton pump inhibitors. The five patients who had vocal cord palsy resulting from cancer invasion of the RLN underwent injection laryngoplasty under local anesthesia 2 weeks after thyroidectomy to improve the voice. The patient with idiopathic vocal cord palsy was asymptomatic before thyroidectomy and the RLN of the contralateral side was not injured during thyroidectomy so no treatment was performed.
Discussion
Vocal disability has always been considered an uncomfortable complication of thyroidectomy [9]. These problems are usually attributed to RLN trauma, although some reports have shown that voice alterations are present even in patients with normal nerve function [11]. The proposed mechanisms for voice alteration despite grossly normal RLN function include partial or subclinical RLN dysfunction and unrecognized, partial, or subclinical EBSLN dysfunction. Other possible etiological factors include endotracheal tube-associated vocal cord or laryngeal injury, direct cricothyroid muscle injury, regional surgical effects such as strap-muscle denervation and regional scarring or laryngeal tethering, and coincident voice change from nonthyroid pathology [12]. Many studies have examined these etiologies of voice change after thyroidectomy. Of these etiologies, coincident voice change from nonthyroid pathology has not been recognized. However, considering the high incidence of voice disorders resulting from many pathologic laryngeal conditions such as LPR and vocal cord mucosal diseases, the possibility of coincident voice disorders among thyroidectomy patients may be high. In these cases, undetected underlying voice disorders will likely be considered to result from the ensuing thyroid surgery, proper diagnosis and treatment may be delayed, and legal problems may result. Previous studies have reported the importance of performing a videolaryngoscopic examination prior to thyroidectomy to detect laryngeal abnormalities [6, 13]. In these studies, a routine videolaryngoscopic examination prior to surgery was considered important, especially in professional voice users, because it could diagnose the presence of an asymptomatic laryngeal alteration that could be exacerbated by surgery. However, all of these studies focused on vocal cord palsy resulting from thyroid diseases or thyroidectomy. No studies have been performed on preexisting pathologic laryngeal conditions unrelated to thyroid pathologies or on screening of voice-impairing diseases before thyroidectomy. To the best of our knowledge, the present study is the first trial that investigated the incidence of coincident voice disorders in a cohort of patients scheduled to undergo thyroidectomy.
In the present study, the incidence of pathologic laryngeal conditions was surprisingly high at 35.8%. Among these patients, LPR was diagnosed in 76.0%. Because we used only laryngoscopic and stroboscopic findings to diagnose LPR, we cannot be certain that all of these patients definitively had laryngopharyngeal reflux disease (LPRD). However, the aim of the present study was to screen for pathologic laryngeal conditions, and stroboscopic findings that suggest the presence of LPRD are a useful screening tool. Other than LPR, benign vocal cord diseases were observed in 8.6% (43/500) of all patients. These high incidences of LPR and benign vocal cord diseases justify routine laryngeal and voice examinations before thyroidectomy. In addition to detecting preexisting voice disorders, there is another reason for and advantage of laryngeal and voice screening. Many voice disorders, such as vocal polyp, vocal cyst, and Reinke’s edema, require surgical treatment for voice improvement. Surgical treatment of these disorders takes a very short time (approximately 10 min) and can be easily performed by the otolaryngologist. Through simultaneous surgeries, patients can avoid additional general anesthesia and can have a rather improved voice after thyroidectomy. In the present study, nine patients with vocal polyp, two with Reinke’s edema, and one with vocal cyst underwent simultaneous microlaryngeal surgery and thyroidectomy; improved voice quality was shown both subjectively and objectively. In addition to disorders that require surgical treatment, other disorders that require medical treatment can be managed properly after thyroidectomy, and voice improvement can be achieved. LPR is a very common disorder [14] and is reported to affect voice quality [15]. All patients diagnosed with LPR were treated with a proton pump inhibitor, which is reportedly the most effective treatment for LPRD [16]. The second most common laryngeal pathology in this study was vocal nodule (24 patients). These patients were successfully managed with voice therapy, which is recognized as the standard therapy for this disorder. In summary, through preoperative laryngeal examination and voice analysis, we detected many voice-affecting disorders, and after proper counseling, we effectively managed these disorders during and just after thyroidectomy, eventually improving patients’ voice quality.
Several other factors argue in favor of routine laryngeal and voice examinations prior to thyroidectomy. First, it is reported that one third or more of patients with unilateral vocal cord palsies are asymptomatic [17]. In the later period of vocal cord palsy, patients can be asymptomatic because of variability in remaining cordal function, paralytic cord position, and contralateral cord compensation [18, 19]. Preoperative recognition of vocal cord palsy is essential in planning the procedure because surgical management of an invaded RLN is based in part on knowledge of its preoperative function. Preoperative knowledge of vocal cord function is also essential for intraoperative decision-making. Many authors have recommended that if preoperative vocal cord function is normal, every attempt should be made to resect all invasive disease, leaving, at most, microscopic disease on the functioning RLN; the nerve should not be resected [20, 21]. In the present study, six patients had vocal cord palsy before thyroidectomy, and all of their diagnoses were thyroid cancers. Among them, five patients showed vocal cord palsy on the same side as the thyroid cancer. For these patients, the surgeon expected that the RLN would be involved with the cancer before the surgery and did not hesitate to sacrifice the RLN after finding cancer invasion of the nerve. For these five patients, injection laryngoplasty, which is reportedly one of the most useful treatment modalities for unilateral vocal cord palsy [22], was performed 2 weeks after thyroidectomy to improve the patients’ voice quality. In one patient, preexisting vocal cord palsy was not a result of the patient’s thyroid pathology; the patient’s thyroid cancer was in the right lobe, but the patient showed left vocal cord palsy. The patient had never been diagnosed with vocal cord palsy. Diagnostic tests failed to identify the cause of the vocal cord palsy so the patient was diagnosed with idiopathic vocal cord palsy. During this patient’s surgery, care was taken to avoid injuring the right RLN to prevent bilateral vocal cord palsy, and the patient showed intact right vocal cord movement on postoperative evaluation. The surgeon obtained information on the importance of preserving the right RLN in this patient through proper preoperative screening, preventing serious complications of bilateral vocal cord palsy.
Another reason for routine laryngeal and voice examinations is the important and growing trend toward evidence-based outcome analysis of operative practice. If we are to accurately determine the true rates of RLN palsy resulting from thyroid operations, we must preoperatively examine the larynx of all patients. For these reasons, many investigators have made similar recommendations regarding the importance of preoperative laryngeal and voice examinations in patients undergoing thyroid operations [18]. Grillo et al. [23] stated, “preoperative assessment of vocal cord function is, of course, routine.”
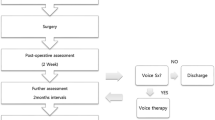
However, because of various logistic difficulties, laryngeal examination and voice analysis are not common practices; these examinations are time-consuming, require specific instruments, add extra costs, and are unpleasant for patients. For these reasons, performing routine laryngeal examination and voice analysis before thyroidectomy is nearly impossible. Therefore, a quick examination tool that is noninvasive and easy to use and that provides a summary of vocal parameters useful in discriminating different voice disturbances may make effective screening possible. With this in mind, we invented the simple “thyroidectomy-related voice questionnaire” and evaluated its usefulness in screening before thyroidectomy. The main basis of this questionnaire is the VHI, which is the most widely used questionnaire for evaluating subjective voice quality in various studies, including those on thyroidectomy-related voice symptoms. However, the VHI does not contain questions specific for LPR. Considering that the incidence of LPR is high and LPR frequently impairs voice quality, we added questions concerning LPR-related symptoms. When we evaluated the usefulness of the questionnaire, the scores were significantly different between the normal and abnormal groups (P = 0.000). To validate its usefulness, we investigated its correlation with objective voice parameters, and the questionnaire showed a statistically significant correlation with shimmer and G (correlation coefficients of 0.091 and 0.260, respectively). Therefore, the questionnaire effectively distinguished between normal and abnormal groups and showed correlations with objective parameters. Furthermore, a cutoff score of 5 showed the best sensitivity and specificity in detecting abnormal laryngeal conditions. From these results, we recommend that the questionnaire be completed by patients before thyroidectomy, and if a patient’s score is higher than 5, further laryngeal examination and voice analysis should be performed to detect preexisting abnormal laryngeal conditions.
In conclusion, the frequency of coincident abnormal laryngeal conditions that can impair the voice quality of patients scheduled to undergo thyroidectomy is high. Therefore, proper screening before thyroidectomy is important. The thyroidectomy-related voice questionnaire is a simple, easy, noninvasive, and effective tool for screening before thyroidectomy. We recommend administering this questionnaire as a screening tool before thyroidectomy. If a patient shows a questionnaire score of more than 5, surgeons can perform laryngoscopy or stroboscopy and voice analysis to detect underlying voice disorders. Through this process, surgeons can tailor their surgical plans and may minimize medicolegal problems; they can also manage voice problems during or just after thyroidectomy.
References
Harness JK, Organ CH Jr, Thompson NW (1995) Operative experience of U.S. general surgery residents in thyroid and parathyroid disease. Surgery 118:1063–1069
Bhattacharyya N, Fried MP (2002) Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg 128:389–392
Roy AD, Gardiner RH, Niblock WM (1956) Thyroidectomy and the recurrent laryngeal nerves. Lancet 270:988–990
Hong KH, Kim YK (1997) Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg 117:399–404
Debruyne F, Ostyn F, Delaere P et al (1997) Acoustic analysis of the speaking voice after thyroidectomy. J Voice 11:479–482
Farrag TY, Samlan RA, Lin FR et al (2006) The utility of evaluating true vocal fold motion before thyroid surgery. Laryngoscope 116:235–238
Fenton JE, Timon CI, McShane DP (1994) Recurrent laryngeal nerve palsy secondary to benign thyroid disease. J Laryngol Otol 108:878–880
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111:1313–1317
de Pedro Netto I, Fae A, Vartanian JG et al (2006) Voice and vocal self-assessment after thyroidectomy. Head Neck 28:1106–1114
Van Lierde K, D’Haeseleer E, Wuyts FL et al (2010) Impact of thyroidectomy without laryngeal nerve injury on vocal quality characteristics: an objective multiparameter approach. Laryngoscope 120:338–345
Stojadinovic A, Shaha AR, Orlikoff RF et al (2002) Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 236:823–832
Pereira JA, Girvent M, Sancho JJ et al (2003) Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery 133:318–322
Yeung P, Erskine C, Mathews P et al (1999) Voice changes and thyroid surgery: is pre-operative indirect laryngoscopy necessary? Aust N Z J Surg 69:632–634
Koufman JA (1991) The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101:1–78
Ross JA, Noordzji JP, Woo P (1998) Voice disorders in patients with suspected laryngo-pharyngeal reflux disease. J Voice 12:84–88
Berardi RR (2000) A critical evaluation of proton pump inhibitors in the treatment of gastroesophageal reflux disease. Am J Manag Care 6:S491–S505
Sittel C, Stennert E, Thumfart WF et al (2001) Prognostic value of laryngeal electromyography in vocal fold paralysis. Arch Otolaryngol Head Neck Surg 127:155–160
Steurer M, Passler C, Denk DM et al (2002) Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope 112:124–133
Randolph GW, Kamani D (2006) The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery 139:357–362
Falk SA, McCaffrey TV (1995) Management of the recurrent laryngeal nerve in suspected and proven thyroid cancer. Otolaryngol Head Neck Surg 113:42–48
Nishida T, Nakao K, Hamaji M et al (1997) Preservation of recurrent laryngeal nerve invaded by differentiated thyroid cancer. Ann Surg 226:85–91
Lee SW, Kim JW, Chung CH et al (2010) Utility of injection laryngoplasty in the management of post-thyroidectomy vocal cord paralysis. Thyroid 20:513–517
Grillo HC, Suen HC, Mathisen DJ et al (1992) Resectional management of thyroid carcinoma invading the airway. Ann Thorac Surg 54:3–9
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nam, IC., Bae, JS., Shim, MR. et al. The Importance of Preoperative Laryngeal Examination Before Thyroidectomy and the Usefulness of a Voice Questionnaire in Screening. World J Surg 36, 303–309 (2012). https://doi.org/10.1007/s00268-011-1347-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1347-5