Abstract
Purpose
Laparoscopic proximal gastrectomy (LPG) is a function-preserving surgery performed on patients with cancer of the upper third of the stomach. However, if much of the ingested food passes through the jejunum, LPG might function broadly like a total gastrectomy. We devised a jejunogastrostomy with double-tract reconstruction (DTR) to ensure that most food flows easily to the remnant stomach.
Methods
A side-to-side jejunogastrostomy was created between the remnant stomach's posterior wall and the jejunum 10 cm below the esophagojejunostomy, and the common stab incision was also closed with a linear stapler. The jejunogastrostomy was created as a delta-shaped anastomosis by using only linear staplers. The 15 patients who underwent delta-shaped anastomosis from 2017 to 2018 were retrospectively reviewed to collect and analyze their surgical and postoperative outcomes, including nutritive conditions, in comparison to the reconstruction that was performed before then.
Results
Operative times and postoperative complications were not significantly different compared to the previous reconstruction. We confirmed significant differences in operative bleeding and passage of food through the remnant stomach. The level of nutritional indicators at the end of postoperative year one did not tend to be lower, but total weight loss (TWL) and %TWL were significantly lower. As expected, there was a correlation between differences in jejunogastrostomy type and postoperative malnutrition.
Conclusions
This method devised for intracorporeal DTR provided patients with improved postoperative nutritional status by directing more food through the remnant stomach after LPG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current studies have reported that upper-third gastric cancer, including early-stage cancer, is on the rise in East Asia [1]. Previously, total gastrectomy (TG) with extensive dissection of lymph node was performed even for relatively early disease, but recent reports have shown that proximal gastrectomy (PG) with lymph node dissection achieves an oncological outcome similar to that of TG, at least in patients with cancer of the upper third of the stomach [2, 3], and an equivalent procedure can be performed with a laparoscope. Takiguchi et al. [4] indicated that PG excelled in the prevention of disorders after surgery like dumping syndrome, diarrhea, and weight loss compared with TG. As a result, PG would likely be conducted more frequently to preserve function with oncological safety in patients with cancer of the upper third of the stomach.
When using PG as a surgery to preserve gastric function, the reconstructions performed after PG are important in offsetting lost gastric function. Several reconstructions can be performed after PG: esophagogastrostomy, jejunal pouch interposition, jejunal interposition, and double-tract reconstruction (DTR). The benefits of every procedure have been shown, but there is no consensus on the appropriate reconstruction after PG [5]. After PG with DTR, the influx of physiological food that can pass through the remnant stomach to the duodenum is reported to be very important for the prevention of postoperative malnutrition in the patient [6].
Various factors cause weight loss following gastrectomy for gastric cancer [7, 8]. Weight loss is an important factor related to nutritional status and quality of life (QOL) of patients following gastrectomy for gastric cancer and has been reported to be a prognostic factor after gastrectomy [8, 9]. The above findings indicate that it is important to reduce the amount of weight loss after this procedure. From 2014 to 2016, we performed DTR according to the method of Ahn et al. [10] after laparoscopic proximal gastrectomy (LPG) previously, but we experienced cases in which the flow of contrast agent into the remnant stomach was not good on postoperative fluoroscopy. Therefore, we made a minor modification to the jejunogastrostomy to allow food to flow to the remnant stomach to reduce weight loss after LPG and assessed postoperative malnutrition compared with that of the previous method.
Methods and patients
Procedures
Laparoscopic proximal gastrectomy
The patient was placed in a reverse Trendelenburg position with legs spread apart under general anesthesia. The surgeon stood on the right side of the patient, the assistant stood on the other side, and the endoscopist stood between the patient’s legs. The endoscope was inserted via the umbilical port, and PG was performed using four working ports that were placed in the upper abdominal area. Then, LPG with D1+ lymph node dissection, as determined in the Japanese gastric cancer treatment guidelines [2], was done for every patient. No. 4d and 6 lymph nodes with the right gastroepiploic vessels and No. 5 lymph nodes with the right gastric vessels were preserved for the distal remnant stomach. The abdominal esophagus and the distal half of the stomach were then individually divided with a linear stapler to ensure a surgical margin from the tumor.
Reconstructions
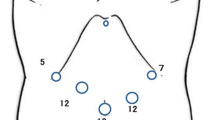
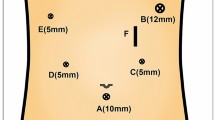
In the first half of the study period, from January 2014 to December 2016 (defined as the first group), we performed DTR after LPG as reported by Ahn et al. [10]. The jejunum was transected by a linear stapler at a location 20 cm from the Treitz ligament. The distal length of the jejunum (approximately 20 cm) was removed to avoid excessive tension at the esophagojejunostomy. An end-to-side esophagojejunostomy was created by intracorporeal anastomosis with 21-mm OrVil™ so that the mesentery of the jejunal limb was on the patient’s right side. A side-to-side jejunogastrostomy of 6 cm in diameter was created 10 cm below the esophagojejunostomy using extracorporeal hand-sewn suture, and then an end-to-side jejunojejunostomy was created about 20 cm below the jejunogastrostomy, also with extracorporeal hand-sewn suture. From January 2017 to December 2018, (defined as the second group), DTR was performed under totally laparoscopic surgery. The jejunum was transected by a linear stapler at a location 20 cm from the Treitz ligament. Esophagojejunostomy was created in the same manner as in the first group. A side-to-side jejunogastrostomy was created between the remnant stomach's posterior wall and the antimesenteric side of the jejunum 10 cm below the esophagojejunostomy. The common stab incision was also closed with a linear stapler. The jejunogastrostomy was created as a delta-shaped anastomosis by a linear stapler (Fig. 1a, b). The jejunal limb was pulled downward due to the weight of the remnant stomach and was twisted in the ventral direction with respect to its long axis (Figs. 2d and 3). Then, a side-to-side jejunojejunostomy was created approximately 20 cm below the jejunogastrostomy with a linear stapler.
Schematic illustration of jejunogastrostomy. a The remnant stomach is twisted, then a side-to-side jejunogastrostomy is created between the jejunal limb and the posterior wall of the remnant stomach. b After the linear stapler is fired, a V-shaped anastomosis is made between the jejunal limb and the remnant stomach. c Closure of the common stab incision. d The jejunal limb rides on the remnant stomach because of the twisting jejunum to the ventral side. And, the exit route of the jejunum is a narrow and slight bend (black arrow)
Patients
In this retrospective study, LPG with DTR was performed in 32 patients at Teikyo University Hospital, Mizonokuchi. We excluded the following patients: patients with liver cirrhosis of Child grade B or C, diabetic patients with HbA1C of 7% or more, patients with chronic kidney disease and eGFR <40 ml/min/1.73 m2, patients with COPD and predicted FEV1 <80%, and patients with heart failure with symptoms appearing during light work. The 32 patients were divided into two groups according to the difference in the jejunogastrostomy mentioned above. In the first group, 17 patients underwent LPG with DTR that performed with a side-to-side jejunogastrostomy created with extracorporeal hand-sewn suture. In the second group, 15 patients underwent LPG with DTR in which a similar type of jejunogastrostomy with delta-shaped anastomosis was created under totally laparoscopic surgery. The preoperative diagnosis was made with the aid of endoscopy, ultrasonography, and contrast-enhanced CT. The indications for surgery were gastric cancer in a clinically early stage and esophageal–gastric junction cancer, including additional resections performed after the endoscopic submucosal dissection, and the ability to preserve more than half of the distal stomach. This study procedures were approved by the institutional review board of Teikyo University (No 18-207). Characteristics, surgical conditions, and postoperative outcomes were acquired from the patients’ medical records. Preoperative clinical data were acquired within 2 weeks before gastrectomy, and postoperative data were acquired at 1 year after surgery. The pathological diagnosis of the tumor was made in accordance with the Japanese Classification of Gastric Carcinoma. The Clavien–Dindo classification was used to judge postoperative complications. Postoperative malnutrition was classified according to the following diagnostic criteria for malnutrition option 2 in the ESPEN guideline: weight loss > 10% and reduced body mass index (BMI) of < 20 kg/m2 in patients younger than 70 years or < 22 kg/m2 in those older than 70 [11].
Postoperative fluoroscopic examination
The postoperative fluoroscopic examination was performed on postoperative day (POD) 4 or 5 to determine whether anastomotic leakage or stenosis was absent. The patients were divided into two groups based on whether contrast medium passed through the remnant stomach (PRS group; Fig. 4a, b) or did not pass through the remnant stomach (non-PRS group; Fig. 4c).
Postoperative fluoroscopic images. In a, the contrast agent passed only through the remnant stomach, whereas in b it passed through both the remnant stomach and the jejunum. These images were classified as “passing through the remnant stomach (PRS)”. In c, the contrast agent passed only through the jejunum. This image was classified as “non-PRS”
Statistical analysis
Clinicopathological findings and clinical outcomes in the two groups were compared with t tests, Fisher’s exact test, and the Mann–Whitney test. A value of p < 0.05 was considered to indicate statistical significance. All statistical analyses were performed with SPSS® version 26 software (IBM, Chicago IL).
Results
Patient characteristics and clinicopathological features are given in Table 1. The study cohort included 17 patients in the first-half group and 15 patients in the second-half group. Between these two groups, only age was higher in the second group, but no significant differences were found for sex, weight, BMI, the final-stage cancer, and hematological nutritional indicators.
The results of the differences in jejunogastrostomy are given in Table 2. Operative time and postoperative complications were not significantly different, but we did confirm significant differences in operative bleeding and PRS. At 1 year postoperatively, nutritional indicators like hemoglobin and serum albumin level were not lower in the first group than the second group. But, TWL and %TWL were significantly greater in the first group than the second group. As expected, there was a correlation between differences in jejunogastrostomy technique and postoperative malnutrition.
The univariate analysis of factors related to postoperative malnutrition is given in Table 3. No significant differences in age, sex, operative time, operative bleeding, postoperative complication, and the final-stage cancer were observed between the two groups. However, the PRS group was less likely to experience postoperative malnutrition than the non-PRS group. Serum albumin and hemoglobin level at postoperative year 1 in the postoperative malnutrition group were not lower than the postoperative non-malnutrition group. However, TWL and %TWL in the postoperative malnutrition group were significantly greater than the postoperative non-malnutrition group.
Discussion
In this cohort study, we showed that the jejunogastrostomy we devised to allow increased food flow into the remnant stomach after LPG with DTR was effective in preventing postoperative malnutrition. The %TWL 1 year after LPG was 15.4% in the first group and 9.4% in the second group. Bodyweight change was related to postoperative malnutrition, and postoperative malnutrition was related to food flow as indicated by the passage of contrast agent through the remnant stomach on postoperative fluoroscopy.
As the detection rate of early gastric cancer has increased, so has the number of long-term survivors after gastrectomy [12, 13]. Thus, it has become necessary to devise a gastrectomy method to reduce post-gastrectomy functional disorder and provide patients with better QOL. A variety of options are available when performing gastrectomy for gastric cancer, such as function-preserving surgery that leaves the pylorus, functional reconstruction that creates a substitute stomach, and the reconstruction route, depending on the location, size, and progression of the cancer. The basic concepts in the choice of options are not to impair the curability that should be secured by a standard gastrectomy and to minimize problems in postsurgical life including postoperative nutritional status. LPG is one of the limited surgeries that preserves function and offers several benefits by maintaining gastric hormones and gastric acid production that results from preserving the gastric antrum [14].
Several reconstructions can be created after LPG: esophagogastrostomy, jejunal interposition, jejunal pouch interposition, and DTR [15]. The benefits of each reconstruction have been shown, and in any reconstruction, the most important thing is to prevent reflux esophagitis, which can significantly decrease the postoperative QOL [16]. Although only studies with small sample sizes show these results, DTR, as a simpler reconstruction procedure, results in comparatively low reflux symptoms [17]. Furthermore, DTR may be advantageous in terms of digestion and absorption, because it preserves the passage of food through the remnant stomach and duodenum. In fact, passage of a stable isotope 13C-labeled lipid compound through the duodenum in patients who underwent gastrectomy showed better absorption ability and physiological state in these patients [18]. Further, even in DTR after PG, a large inflow of food into the remnant stomach will prevent malnutrition after gastrectomy [6]. In contrast, if most of the ingested food passes via the escape route of the jejunum, the functional benefits offered by PG might resemble those experienced after total gastrectomy. Thus, we devised an anastomosis between the jejunal limb and the remnant stomach so that more food flows through the remnant stomach into the duodenum. As a result, intraabdominal jejunogastrostomy-like delta-shape allowed more food inflow into the remnant stomach and less postoperative malnutrition than a hand-sewn jejunogastrostomy.
We consider that the following two reasons for the increased flow to the remnant stomach. First, the jejunal limb was directed to the patient’s left side, because the esophagojejunostomy was performed such that the mesentery of the jejunal limb was on the patient’s right side, which allowed the remnant stomach to be relatively free to move with lymph node dissection. The jejunogastrostomy was performed by lateral anastomosis between the jejunal limb and the remnant stomach’s posterior wall. The remnant stomach pulls the jejunogastrostomy in a downward vector by its own weight with the patient in a sitting or standing position. However, a leftward force is always applied to the jejunal limb. Due to the resulting balance between the jejunal limb vector and the remnant stomach vector, the meal flows linearly from the jejunal limb into the remnant stomach (Fig. 5a). Second, as a result of forming the jejunogastrostomy into delta-like shape, the exit route of the jejunum became narrow and the outflow towards the exit route was less flexible after closing the entry hole with a linear stapler. We think this method of closing the entry hole was the cause of the slight bend in the jejunum that allows more flow into the remnant stomach (Fig. 5b). We thus considered that the flow from the jejunal limb in the direction of the remnant stomach and not in that of the exit route of the jejunum was linearized so that the meal would flow easily to the remnant stomach. Moreover, even if the linear flow to the remnant stomach is not sufficient, it is easy for food to flow to the remnant stomach due to the narrow and slight bend in the exit route of the jejunum (Figs. 2d and 5b).
Right anterior oblique images showing a, contrast agent passing only through the remnant stomach (arrow shows the vector from the jejunal limb to the remnant stomach), and b, contrast agent passing through both the remnant stomach and distant jejunum (arrowheads indicate the slight bend in the exit route of the jejunum)
DTR is one of the jejunal interpositions for PG and is thought to be a better method that contributes to the prevention of body weight loss after gastrectomy. Jejunal interposition for proximal gastrectomy (PG-JI), which reduces postoperative body weight loss compared to the Roux-en-Y reconstruction for TG, contributes to better patient QOL and thus has been well embraced [17]. Esophageal reflux is reported to be significantly less frequent after PG-JI [19, 20]. In addition, mesentery division is not necessary with DTR and continuity of the jejunum is maintained. Further, there is no issue with delayed gastric emptying, because even if it does occur, an alternative route exists for the passage of food, contrary to other types of jejunal interposition [10]. These characteristics of DTR help to ensure a certain amount of oral intake after gastrectomy, thus preventing weight loss in patients who undergo DTR.
This study has limitations. First, it is a retrospective, single-center study with a comparatively small sample size. On the basis of the present results, we are planning a multicenter study with an adequate sample size and will conduct multivariate logistic regression analysis to examine independent factors. Second, the route of food passage was evaluated with fluoroscopy, which is performed in the first week after the gastrectomy, but it is not known whether this reflects the evaluation of the route long term after the gastrectomy. In addition to evaluating liquid flow, it is also necessary to evaluate solid flow, such as by cine magnetic resonance imaging [21]. Only five patients in the second group underwent fluoroscopy 1 year later, and all five had meal flow to the remnant stomach similar to that found on fluoroscopic examination 1 week after the operation (Fig. 6a, b). There is still room for improvement, and further research is needed to prevent postoperative malnutrition after LPG. In particular, changing the esophagojejunostomy from a circular stapler method to a linear method as a means of increasing oral intake may provide better results in the prevention of postoperative malnutrition [22].
Fluoroscopic images 1 year later. In a, frontal and right anterior oblique images show contrast agent passing through only the remnant stomach. In b, frontal and right anterior oblique images show contrast agent passing through both the remnant stomach and exit route. Inflow into the remnant stomach is as good as that shown in the fluoroscopic images obtained immediately postoperatively
Conclusion
We have developed a jejunogastrostomy that stabilizes the flow of food to the remnant stomach to help prevent the postoperative malnutrition that can occur after DTR in LPG.
References
Ahn HS, Lee HJ, Yoo MW et al (2011) Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg 98:255–260
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–9
Giacopuzzi S, Bencivenga M, Weidelmayer J et al (2017) Western strategy for EGJ carcinoma. Gastric Cancer 20:60–68
Takiguchi N, Takahashi M, Ikeda M et al (2015) Long-term quality-of-life comparison of total gastrectomy and proximal gastrectomy by postgastrectomy syndrome assessment scale (PGSAS-45): a nationwide multi-institutional study. Gastric Cancer 18:407–416
Nakamura M, Yamaue H (2016) Reconstruction after proximal gastrectomy for gastric cancer in upper third of the stomach: a review of the literature published from 2000 to 2014. Surg Today 46:517–527
Yamashita K, Iwatsuki M, Koga Y et al (2019) Preservation of physiological passage through the remnant stomach prevents postoperative malnutrition after proximal gastrectomy with double tract reconstruction. Surg Today 49:748–754
Abdiev S, Kodera Y, Fujiwara M et al (2011) Nutritional recovery after open and laparoscopic gastrectomies. Gastric Cancer 14:144–149
Climent M, Munarriz M, Blazeby JM et al (2017) Weight loss and quality of life in patients surviving 2 years after gastric cancer resection. Eur J Surg Oncol 43:1337–1343
Yu W, Seo BY, Chung HY (2002) Postoperative body-weight loss and survival after curative resection for gastric cancer. Br J Surg 89:467–470
Ahn SH, Jung DH, Son SY et al (2014) Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer 17:562–570
Weimann A, Braga M, Carli F et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36:623–650
Adachi Y, Kitano S, Sugimachi K (2001) Surgery for gastric cancer: 10-year experience worldwide. Gastric Cancer 4:166–174
Takiguchi S, Masuzawa T, Hirao M et al (2011) Pattern of surgical treatment for early gastric cancers in upper third of stomach. Hepatogastroenterology 58:1823–1827
Nunobe S, Hiki N (2017) Function-preserving surgery for gastric cancer: current status and future perspectives. Transl Gastroenterol Hepatol 2:77
Kojima M, Hosoda H, Date Y et al (1999) Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 402:656–660
Wang S, Lin S, Wang H et al (2018) Reconstruction methods after radical proximal gastrectomy: a systemic review. Medicine 97:11
Nomura E, Lee SW, Kawai M et al (2014) Functional outcomes by reconstruction technique following laparoscopic proximal gastrectomy for gastric cancer: double tract versus jejunal interposition. World J Surg Oncol 12:20
Takase M, Sumiyama Y, Nagano J (2003) Quantitative evaluation of reconstruction methods after gastrectomy using a new type of examination: digestion and absorption test with stable isotope 13C-labeled lipid compound. Gastric Cancer 6:134–141
Masuzawa T, Takiguchi S, Hirao M et al (2014) Comparison of perioperative and long-term outcomes of total and proximal gastrectomy for early gastric cancer: a multi-institutional retrospective study. World J Surg 38:1100–1106. https://doi.org/10.1007/s00268-013-2370-5
Tokunaga M, Ohyama S, Hiki N et al (2008) Endoscopic evaluation of reflux esophagitis after proximal gastrectomy: comparison between esophagogastric anastomosis and jejunal interposition. World J Surg 32:1473–1477. https://doi.org/10.1007/s00268-007-9459-7
Baba S, Sasaki A, Nakajima J et al (2009) Assessment of gastric motor function by cine magnetic resonance imaging. Gastroenterol Hepatol 24:1401–1406
Hong J, Qian L, Wang YP et al (2016) A novel method of delta-shaped intracorporeal double-tract reconstruction in totally laparoscopic proximal gastrectomy. Surg Endosc 30:2396–2403
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
DF and KT were responsible for the study design and for the acquisition, analysis and interpretation of the data. HK critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from the institutional review board of the Teikyo University (No 18-207).
Informed consent
Informed consent was obtained prior to recruitment from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujimoto, D., Taniguchi, K. & Kobayashi, H. Double-Tract Reconstruction Designed to Allow More Food Flow to the Remnant Stomach After Laparoscopic Proximal Gastrectomy. World J Surg 44, 2728–2735 (2020). https://doi.org/10.1007/s00268-020-05496-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05496-0