Abstract
Background
Frequent stooling immediately after pull-through (PT), fecal soiling, and constipation are chronic complications of Hirschsprung’s disease (HD). This study aimed to investigate the longitudinal outcomes in terms of bowel function of patients below the age of 1 year undergoing PT.
Methods
We retrospectively evaluated 396 patients who underwent PT for HD between September 1979 and March 2014. Stool frequency was analyzed up to 10 years of age, and soiling and constipation were analyzed up to 15 years of age.
Results
After resection of the aganglionic segment (AS), stool frequency decreased over time. Furthermore, stool frequency among the three groups was similar 4 years after PT. Among the patients with aganglionic bowel resection, those who underwent the Soave procedure (SP) had an increase (0.56/day) in stool frequency than those who underwent the Duhamel procedure (DP). The soiling severity according to the AS was similar after 5 years of age. More severe soiling was better associated with patients who underwent the SP than those who underwent the DP. The constipation severity increased gradually until around 5 years and declined thereafter. More severe constipation was better associated with the DP than with the SP.
Conclusion
The result of the analysis of stool frequency and soiling in patients with HD indicated that shorter ASs resulted in fewer bowel movements and less severe soiling. However, with the increase in patient age, the differences became similar. Compared to the DP, the SP was associated with an increased frequency of bowel movements and soiling severity; however, the constipation severity was lower.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hirschsprung’s disease (HD) is a developmental disorder of the intrinsic components of the enteric nervous system. HD is characterized by the absence of ganglionic cells in the myenteric and submucosal plexuses of the distal bowel and has occurred in approximately 1 in 5000 newborns [1]. Although HD is mainly limited to the rectum and distal colon, 2–13% of patients present with total colonic aganglionosis [2, 3]. Surgical intervention for HD involves removal of the aganglionic bowel and subsequent pulling of the normally innervated bowel through the anus to allow for normal bowel movements; this procedure is referred to as pull-through (PT) surgery. However, PT does not always result in satisfactory bowel function, and frequent stooling immediately after the PT, fecal soiling, and constipation are chronic complications associated with HD. Although several studies have reported the long-term outcomes associated with bowel function after PT, they did not elucidate the patterns of stooling, soiling, and constipation [4,5,6,7,8,9,10,11,12,13]. Furthermore, previous studies that examined stooling changes after the Soave procedure (SP) had small sample sizes and short follow-up periods [11, 12].
Many patients with HD undergo PT prior to their first birthday, and the age for definitive surgery for HD is decreasing. According to a nationwide survey in Japan, the mean age for definitive surgery was 564.8 days in 1978–1982 and 324.3 days in 2008–2012 [14]. Moreover, Tang et al. reported that 87.6% of patients with HD underwent definitive surgery aged at <1 year of age [15].
This study aimed to investigate the longitudinal outcomes of patients with HD who underwent successful PT at <1 year of age. We conducted this study on a large number of HD patients in a single center. The measured outcomes included changes in stool frequency, soiling, and constipation from the protocoled outpatient follow-up. In particular, we analyzed the differences in long-term outcomes according to the aganglionic segment (AS) involved and the PT method used.
Methods
We retrospectively evaluated 622 patients who underwent PT for HD between September 1979 and March 2014 at Seoul National University Children’s Hospital. Gestational age, birth weight, sex, age/weight on the day of surgery, surgical method, location of the aganglionic segment, postoperative clinical course, and bowel function parameters (voluntary bowel movement, stool frequency, and the presence and severity of soiling/constipation) after surgery were analyzed. All patients were diagnosed as having HD based on pathological aganglionosis. Patients who underwent PT at <1 year of age and at least 3 years prior to the start of data collection were included in this study. Patients who underwent redo PT for various reasons, the Martin procedure, or enterostomy restoration later as opposed to during the PT were excluded from the study. The Martin procedure was defined as leaving aganglionic distal bowel above the sigmoid colon [16]. Of the 622 patients, 209 who underwent PT at ≥1 year of age, 13 who underwent redo PT, 2 who underwent the Martin procedure, and 2 who underwent delayed enterostomy restoration were excluded. Altogether, 396 patients were enrolled, including 308 who underwent the Duhamel procedure (DP) and 88 who underwent the SP. Length of aganglionosis was confirmed pathologically, and the AS was determined by matching the anatomy of each patient. Patients were classified into three groups according to the aganglionosis in the distal bowel as follows: (1) rectosigmoid colon (RS), (2) intestine from the descending colon to the transverse colon (DT), and (3) intestine above the ascending colon, including the small bowel (total colon).
The DP performed at our institution preserved the rectum and pulled through the ganglionated bowel between the rectum and the sacrum. The rectum is usually preserved to the level of approximately 3 cm above the peritoneal reflection, and side-to-side anastomosis was performed with an automatic stapling device (GIA, 90 or 100 mm). The SP was performed through laparotomy or laparoscopy to mobilize the proximal bowel, followed by transanal endorectal dissection between 0.5 and 1.5 cm above the dentate line. At this time, the anterior and posterior walls of the rectal muscle cuff were split, and the length of the muscle cuff was kept as short as possible. During the study period, five pediatric surgeons performed either the DP or SP according to their preference. In our institution, when PT was performed, a full-thickness biopsy was taken approximately 2–3 cm above the transitional zone, and the presence or absence of ganglion cells was determined using frozen sections. If no ganglion cells were found, another biopsy was performed in the proximal 5 cm of the intestine. The extent of resection of the distal ganglionated bowel remains unknown. In our institution, the intestines were finally resected at least 3 cm above the ganglionated bowels as identified from the frozen sections.
Complications were classified into early complications occurring within 30 days of surgery and late complications occurring 30 days after surgery.
We aimed to record the stool frequency and degree of soiling and constipation in outpatients. The postoperative follow-up protocol was performed at weeks 1 and 2; at months 1, 3, 6, 9, 12, 18, 24, 30, 36, 42, 48, 54, and 60; and every year thereafter. Prior to the patient having a voluntary bowel movement, stooling was defined as the need for a diaper change. Staining of the diaper or underwear was classified as soiling. Constipation was defined as fewer than three defecations per week, the requirement of a dietary adjustment to facilitate defecation, or laxative use [17, 18]. The collection of longitudinal outcome data for each patient was based on the surgeon’s notes, and a single researcher systematically conducted the collection of such data in the second half of 2017. Of the 396 patients, complete data on stool frequency, soiling, and constipation were gathered postoperatively for 391 patients (98.7%) at 6 months, 392 patients (99%) at 1 year, 391 patients (98.7) at 2 years, and 388 patients (98%) at 3 years. Of the 308 patients, 220 (71.4%) had complete data 5 years after surgery. Complete data were also obtained for 108 (51.4%) of 210 patients at 7 years and 26 (27.6%) of 94 patients at 10 years. Soiling and constipation after 10 years of age were analyzed in 16 (20.2%) of 79 patients at 12 years and 11 (17.5%) of 63 patients at 15 years. We analyzed the severity of soiling and constipation using the Krickenbeck continence score [18]. The Krickenbeck score is based on clear definitions of continence parameters and is the most applicable and objective method of bowel control evaluation in pediatric cases [19]. To compare the severity of soiling and constipation, we scored 0 for absence, and 1, 2, and 3 for grades 1, 2, and 3, respectively. The mean stool frequency was measured postoperatively at 1, 3, and 6 months and at 1, 2, 3, 4, 5, 7 and 10 years. Fecal soiling and constipation were evaluated at 1, 2, 3, 4, 5, 7, 10, 12, and 15 years of age.
Non-parametric variance analysis was performed using the Kruskal–Wallis method for the data of <30 cases, and t tests were conducted for the mean comparisons. Correlations between variables were evaluated using a Chi-square test. A linear mixed model was used to analyze the changes in stool frequency, soiling, and constipation with time after PT. The linear model facilitates the analysis of data collected at various time points in the same patient and is useful even in cases with missing data. The results of the linear mixed model analysis are presented as an “Appendix.” p values of <0.05 were considered to be statistically significant. Statistical analysis was performed by the Medical Research Collaborating Center at the Seoul National University Hospital and Seoul National University College of Medicine. Statistical analysis was performed using SPSS software version 20 (SPSS Inc., Chicago, IL, USA) and SAS 9.4 (SAS institute Inc., Cary, NC, USA).
This study was approved by the institutional review board of Seoul National University Hospital (IRB File No. 1702-061-831).
Results
Of the 396 patients, 298 (75.2%) were male. The mean gestational age was 38.52 ± 1.98 weeks, and the mean birth weight was 3.25 ± 0.55 kg. The results showed 348 RS cases (87.9%), 37 DT cases (9.3%), and 11 total colon procedures (2.8%) according to AS. The median age at PT was significantly younger in the RS group (141 days for RS, 184 days for DT, and 189 days for total colon, p = 0.002). The mean body weight at the time of surgery was 7.44 ± 1.51 kg, which was similar between the three groups. The median follow-up duration of all the patients was 6.23 years (range 0–30.58 years) (Table 1).
In terms of the procedure frequency, 308 patients (77.8%) underwent the DP and 88 patients (22.2%) underwent the SP. The median age at PT was significantly younger in the SP group (121.5 vs. 153 days, p < 0.001), at which time the mean body weight was also lower in the SP group (6.34 ± 1.89 vs. 7.74 ± 1.23 kg, p < 0.001). The AS distribution was similar in the two groups (Table 2).
On the basis of the analysis of the linear mixed model for changes in stool frequency according to AS, PT method, and time after PT, only AS and time had an interaction (Fig. 1). Therefore, the final model was constructed excluding factors without interaction, and a significant interaction was found between AS and time for stool frequency change (p < 0.0001). After resection of the RS, DT, or total colon, stool frequency decreased over time. The difference in stool frequency between the three groups was similar 4 years after PT. The difference in stool frequency between PT methods indicated a mean of 4.07/days (range 3.72–4.42 days) in the SP group and 3.51/days (range 3.25–3.77 days) in the DP group. In other words, in patients who underwent aganglionic bowel resection, a greater difference (0.56/day) in stool frequency occurred in the SP group compared with the DP group, regardless of the AS or time (p < 0.0001).
Long-term outcomes of stool frequency. a The final model showed a significant interaction between aganglionic segment and time for stool frequency change. b After resection of the RS, DT, or total colon, the stool frequency decreased over time. The difference in stool frequency between the three groups was similar 4 years after pull-through
A review of fecal soiling suggested that, as with stool frequency changes, there was an interaction between AS and time (Fig. 2). Soiling decreased with time in the RS, DT, and total colon groups. The soiling severity between the three groups was similar after 5 years of age. The difference in fecal soiling between the procedures was more severe in the SP group (mean 1.09, range 0.92–1.25) compared with the DP group (mean 0.71, range 0.59–0.83) regardless of the AS or time (p < 0.0001).
Long-term outcomes of fecal soiling. The Krickenbeck continence score was used to compare the severity of soiling. A score of 0 was given for the absence of soiling, and 1, 2, and 3 for grades 1 (occasionally), 2 (every day, no social problem), and 3 (constant, social problem), respectively. a The final model shows a significant interaction between aganglionic segment and time for fecal soiling change. b The severity of soiling was similar between the three groups after 5 years of age
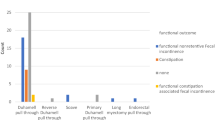
As none of the patients in the total colon group complained of constipation, this group was excluded from further constipation analysis. Further analysis of the remaining groups revealed no significant interactions (Fig. 3). Constipation worsened until approximately 5 years of age but improved thereafter. The difference in constipation score according to AS was 0.33 (range 0.25–0.4) in the RS group and 0.22 (range 0.03–0.41) in the DT group. The RS had a higher overall constipation severity than the DT group, although the difference did not reach statistical significance (p = 0.28). The difference in constipation severity between the procedures was greater in the DP group (mean 0.3, range 0.25–0.45) compared with the SP group (mean 0.2, range 0.05–0.34) regardless of the AS or time (p = 0.02).
Long-term outcomes of constipation. The Krickenbeck continence score was used to compare the severity of constipation. A score 0 was given for the absence of constipation, and 1, 2, and 3 for grades 1 (manageable by change in diet), 2 (required laxative), and 3 (resistant to laxatives and diet), respectively. a None of the interactions was significant. b Constipation worsened until approximately 5 years of age, but improved thereafter
No statistically significant differences were found in early complications according to AS. Late complications occurred more frequently in the DT group than in the other groups; however, detailed analysis revealed no significant differences. With regard to the PT method, no statistically significant difference was observed in terms of early complications, except for enterocolitis. However, late complications were significantly more frequent in the SP group compared with the DP group. No statistically significant differences in mechanical intestinal obstructions were found between the procedures. Rectal prolapse was significantly more frequent in the SP group. Four patients died after PT: 1 patient died of sepsis, 1 of bleeding, 1 from hydrothorax caused by an undetected malpositioned central venous catheter, and in the final patient, the cause of death was unknown. Of the four patients with early mechanical intestinal obstructions, one showed no improvement in ileo-ileal intussusception and three had adhesive ileus. All 13 mechanical intestinal obstructions that occurred as late complications were adhesive ileus (Table 3).
Discussion
In terms of HD, only a few studies have reported on the correlation between altered stool frequency and patient age after PT. Teitelbaum et al. conducted a follow-up study after primary endorectal PT in 24 young infants (mean age at PT 15 ± 17 days) with HD. The results showed a frequency of 5 to 8 stools per day immediately after surgery and a subsequent rapid decline, with a mean of 3.8 ± 1.4 stools per day 6 months after surgery. Thereafter, a gradual decline was noted at the mean follow-up of 1036 ± 614 days [11]. These results were similar to those of our study, in which the RS, DT, and total colon groups showed a drastic decrease in stool frequency until 6 months after surgery, which gradually decreased over the next 10 years. However, Teitelbaum’s study was limited by the small sample size, lack of AS classification, and short follow-up period. Graneli et al. classified stool frequency according to the postoperative period and compared results with those from a healthy group of children [12]. This study reported that stool frequency was higher in patients with HD compared with healthy children, but was similar to that in healthy children 4 years after surgery. However, this study also had limitations including a small sample size, failure to collect data at various time points in the same patient, and a short follow-up duration.
In our study, fecal soiling was more severe after the SP, and constipation was more severe after the DP. The estimated incidence of fecal soiling was reported to range from 6 to 48% after the DP (or mainly DP) [10, 20,21,22] and from 9.4 to 68.4% after the SP [10, 13, 23, 24]. The incidence of constipation ranged from 8.3 to 30% after the DP [10, 25] and from 2.4 to 24% after the SP [10, 23, 26]. In addition to soiling and constipation, the overall bowel function of patients with HD is thought to improve over time. Conway et al. reported a functional outcome score at 8-year intervals in a cohort of patients who underwent the DP. Their results demonstrated improved bowel function with age (1997: 14.9 ± 4.1; 2005: 16.4 ± 2.8; p = 0.02) [27]. However, the reason for this improved bowel function with age was unclear.
The incidence of soiling and constipation has been reported to vary widely. Although the reasons for this variability are unclear, we suspect that it is due to the differences in the definition of fecal soiling and ages of the patients evaluated among the studies. The two aforementioned studies reported the incidence of fecal soiling to be 48% and 68.4% in patients with HD and 22% and 31% in the healthy control group and appeared to have applied overly strict definitions to fecal soiling [13, 22]. We thought that the age at which school begins was the appropriate time to investigate meaningful incidence of fecal soiling and constipation. Thus, we further evaluated 210 patients who were followed up to ≥7 years of age and exhibited a soiling and constipation of grade ≧2 according to the Krickenbeck continence score. The results demonstrated no significant difference in the incidence of soiling between patients in the RS (9.8%), DT (5.5%), and total colon (11.1%) groups (p = 0.833). Constipation occurred in 29 patients (15.8%) in the RS group, 1 patient (5.5%) in the DT group, and 0 patients in the total colon group (p = 0.088). With regard to the PT method, soiling was detected in 13 patients (7.4%) who underwent the DP and in 7 patients (20%) who underwent the SP; however, these results did not reach statistical significance (p = 0.051). The incidence of constipation was similar between the DP and SP groups, with 25 (14.3%) and 5 cases (14.3%), respectively.
Recently, a controlled follow-up study of long-term bowel function and quality of life in patients with HD who underwent transanal endorectal PT showed poor results in almost all areas of fecal control (except constipation) as compared with those in the control group [13]. This study demonstrated that the degree of fecal control impairment differed substantially between the HD and control groups according to age, but this difference decreased with age, and no significant differences were observed at 18 years of age. However, several studies have reported contrasting results; for instance, studies that analyzed bowel function in adults reported that impaired fecal control was still observed into adulthood in patients with HD [22, 27, 28]. However, the DP was the main PT method used in these studies.
Functional outcomes according to the PT method were clearly different in the present study. The advantage of the DP is that it can prevent damage to surrounding structures by restricting dissection of the rectum in the pelvis. The advantage of the SP is its ability to preserve the muscle and serosa layer by transanal submucosal dissection. The cause of fecal incontinence after PT in patients with HD remains unclear. In a recent study that compared the DP and transanal PT, the fecal continence index was not significantly different between the two procedures; however, the DP led to an improvement in the patients’ quality of life [29]. The aganglionic rectal stump is frequently subjected to fecal impactions and can become largely dilated after the DP. Several studies have demonstrated that preserving the mucosa of the dentate line by performing a mucosectomy at the upper level of the dentate line rather than from the dentate line was better for postoperative fecal continence during SP [30,31,32]. This is most likely due to the fact that a mucosectomy from the dentate line is likely to result in damage to the delicate nerve endings on the dentate line that forms the reflex arch, which is responsible for sensation and continence [33]. It is for these reasons we suggest that the incidence rates of constipation and soiling were higher in the DP and SP groups, respectively.
In our institution, we perform PT as soon as possible, if pathological aganglionosis is diagnosed. We previously had a diagnosed outpatient who died of enterocolitis before undergoing PT. Thus, we perform PT without sending the patient home if HD is diagnosed at an outpatient clinic or during the neonatal period in the hospital. During the study period, five pediatric surgeons in our institution performed either the DP or SP according to their preference. The first four senior surgeons primarily performed the DP as an open surgery. Currently, the corresponding author, the fifth surgeon in our institution, primarily performs the SP. The SP was introduced in our institution in 2003, and now, almost all surgeries have been performed with laparoscopy-assisted SP. As many pediatric surgeons know, if the rectal muscular cuff is longer than necessary in the SP, compression can disturb the peristalsis of the pulled-through normal colon [34]. In the early days, we followed literature recommendations regarding the SP while ensuring that the muscular cuff did not exceed 5 cm. Over time, studies have indicated that shorter rectal muscular cuffs have a lower risk of rectal stenosis or stricture [35]. Therefore, we elect to keep the rectal muscular cuff as short as possible.
The term successful PT, which was used to describe the aim of this study, refers to a definitive surgery that has been achieved with only one pull-through surgery. In this study that solely investigated successful PT, we wanted to characterize bowel function changes in patients who underwent successful surgeries without the need for redo PT. The reasons for the redo PT in this study were as follows: anastomosis site leakage/fistula/abscess/stricture in six patients, remnant aganglionosis in two patients, severe constipation in two patients, and severe fecal soiling in two patients. Four patients received Botox injections due to soiling. We started administering Botox injections in 2016 and excluded this from measurement factors, as all patients were operated on by the author. None of the patients underwent an antegrade continence enema such as cecostomy.
The SP resulted in more frequent bowel movements and a greater severity of soiling than the DP, although constipation was found to be less severe in this study. However, regarding the DP and SP, evidence is insufficient to recommend one procedure over the other. We inform the parents of patients with HD of differences between the surgical procedures and our experience of the clinical courses after each procedure. While we respect the parents’ opinion on PT methods, we believe that the surgeon’s experience and skill are more important factors for selecting the appropriate method. We prefer laparoscopy-assisted SP, but we consider the DP for patients with total colonic aganglionosis.
The retrospective design is a limitation of the present study. The lack of an objective and identical method of checking a patient's bowel function in outpatient clinics is a major limitation of this study. Although we aimed to perform a protocoled outpatient follow-up, a considerable amount of data was missing. To compensate for this, we used a linear mixed model. The policy of our institution is to follow up patients until adulthood; however, many patients are inevitably lost to follow-up. Consequently, the study data could be overestimated, as patients with poor bowel function may have had a longer follow-up period. Despite these limitations, our study applied a relatively unified surgical method, was performed within a single institution, and included a considerable number of patients. Descriptions of changes in bowel function over a long follow-up period would also be of great value. A long-term prospective study and comparison with a healthy sample through controlled group matching are required to validate the results of this study further.
Conclusion
In patients with HD who underwent PT prior to their first birthday, bowel movements and soiling became less frequent and less severe as the area of the AS became shorter. However, these differences decreased with age. In the RS and DT groups, constipation severity according to time increased gradually until around 5 years of age and gradually declined afterwards. The SP resulted in more frequent bowel movements and greater severity of soiling than the DP, although constipation was less severe. Therefore, surgeons will need to consider the most appropriate type of surgical procedure based on these factors. The study results can be used as a reference for physicians, parents, and patients when altered stool frequency, fecal soiling, and constipation are observed in relation to age after PT.
References
Rintala RJ, Pakarinen MP (2012) Long-term outcomes of Hirschsprung's disease. Semin Pediatr Surg 21:336–343. https://doi.org/10.1053/j.sempedsurg.2012.07.008
Cass DT, Myers N (1987) Total colonic aganglionosis: 30 years' experience. Pediatr Surg Int 2:68–75
Moore SW, Rode H, Millar AJ et al (1991) Familial aspects of Hirschsprung's disease. Eur J Pediatr Surg 1:97–101. https://doi.org/10.1055/s-2008-1042468
Moore SW, Albertyn R, Cywes S (1996) Clinical outcome and long-term quality of life after surgical correction of Hirschsprung's disease. J Pediatr Surg 31:1496–1502
Reding R, de Goyet JDV, Gosseye S et al (1997) Hirschsprung's disease: a 20-year experience. J Pediatr Surg 32:1221–1225
Catto-Smith AG, Coffey CM, Nolan TM et al (1995) Fecal incontinence after the surgical treatment of Hirschsprung disease. J Pediatr 127:954–957
Heij HA, de Vries X, Bremer I et al (1995) Long-term anorectal function after Duhamel operation for Hirschsprung's disease. J Pediatr Surg 30:430–432
Shankar KR, Losty PD, Lamont GL et al (2000) Transanal endorectal coloanal surgery for Hirschsprung's disease: experience in two centers. J Pediatr Surg 35:1209–1213. https://doi.org/10.1053/jpsu.2000.8728
Marty TL, Seo T, Matlak ME et al (1995) Gastrointestinal function after surgical correction of Hirschsprung's disease: long-term follow-up in 135 patients. J Pediatr Surg 30:655–658
Menezes M, Corbally M, Puri P (2006) Long-term results of bowel function after treatment for Hirschsprung's disease: a 29-year review. Pediatr Surg Int 22:987–990. https://doi.org/10.1007/s00383-006-1783-8
Teitelbaum DH, Drongowski RA, Chamberlain JN et al (1997) Long-term stooling patterns in infants undergoing primary endorectal pull-through for Hirschsprung's disease. J Pediatr Surg 32:1049–1052 (discussion 1052-1043)
Graneli C, Stenström P, Börjesson A et al (2015) Development of frequency of stools over time in children with Hirschsprung disease posttransanal endorectal one-stage pull-through. Eur J Pediatr Surg 25:359–364. https://doi.org/10.1055/s-0034-1376396
Neuvonen MI, Kyrklund K, Rintala RJ et al (2017) Bowel function and quality of life after transanal endorectal pull-through for Hirschsprung disease: controlled outcomes up to adulthood. Ann Surg 265:622–629. https://doi.org/10.1097/sla.0000000000001695
Taguchi T, Obata S, Ieiri S (2017) Current status of Hirschsprung's disease: based on a nationwide survey of Japan. Pediatr Surg Int 33:497–504. https://doi.org/10.1007/s00383-016-4054-3
Tang ST, Wang GB, Cao GQ et al (2012) 10 Years of experience with laparoscopic-assisted endorectal Soave pull-through procedure for Hirschsprung's disease in China. J Laparoendosc Adv Surg Tech A 22:280–284. https://doi.org/10.1089/lap.2011.0081
Martin LW (1972) Surgical management of total colonic aganglionosis. Ann Surg 176:343–346. https://doi.org/10.1097/00000658-197209000-00010
Abi-Hanna A, Lake AM (1998) Constipation and encopresis in childhood. Pediatr Rev 19:23–30 (quiz 31)
Holschneider A, Hutson J, Peña A et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526. https://doi.org/10.1016/j.jpedsurg.2005.08.002
Bischoff A, Bealer J, Peña A (2016) Critical analysis of fecal incontinence scores. Pediatr Surg Int 32:737–741. https://doi.org/10.1007/s00383-016-3909-y
Nah SA, de Coppi P, Kiely EM et al (2012) Duhamel pull-through for Hirschsprung disease: a comparison of open and laparoscopic techniques. J Pediatr Surg 47:308–312. https://doi.org/10.1016/j.jpedsurg.2011.11.025
Bufo AJ, Chen MK, Shah R et al (1999) Analysis of the costs of surgery for Hirschsprung's disease: one-stage laparoscopic pull-through versus two-stage Duhamel procedure. Clin Pediatr (Phila) 38:593–596. https://doi.org/10.1177/000992289903801004
Jarvi K, Laitakari EM, Koivusalo A et al (2010) Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg 252:977–981. https://doi.org/10.1097/SLA.0b013e3182018542
Dahal GR, Wang JX, Guo LH (2011) Long-term outcome of children after single-stage transanal endorectal pull-through for Hirschsprung's disease. World J Pediatr 7:65–69. https://doi.org/10.1007/s12519-011-0247-y
Khalil M (2015) Long-term health-related quality of life for patients with Hirschsprung's disease at 5 years after transanal endorectal pull-through operation. Qual Life Res 24:2733–2738. https://doi.org/10.1007/s11136-015-1012-9
Scholfield DW, Ram AD (2016) Laparoscopic Duhamel procedure for Hirschsprung's disease: systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 26:53–61. https://doi.org/10.1089/lap.2015.0121
Zimmer J, Tomuschat C, Puri P (2016) Long-term results of transanal pull-through for Hirschsprung's disease: a meta-analysis. Pediatr Surg Int 32:743–749. https://doi.org/10.1007/s00383-016-3908-z
Conway SJ, Craigie RJ, Cooper LH et al (2007) Early adult outcome of the Duhamel procedure for left-sided Hirschsprung disease: a prospective serial assessment study. J Pediatr Surg 42:1429–1432. https://doi.org/10.1016/j.jpedsurg.2007.03.046
Ieiri S, Nakatsuji T, Akiyoshi J et al (2010) Long-term outcomes and the quality of life of Hirschsprung disease in adolescents who have reached 18 years or older: a 47-year single-institute experience. J Pediatr Surg 45:2398–2402. https://doi.org/10.1016/j.jpedsurg.2010.08.040
Tannuri AC, Ferreira MA, Mathias AL et al (2017) Long-term results of the Duhamel technique are superior to those of the transanal pullthrough: a study of fecal continence and quality of life. J Pediatr Surg 52:449–453. https://doi.org/10.1016/j.jpedsurg.2016.10.007
Martin LW, Fischer JE, Sayers HJ et al (1986) Anal continence following Soave procedure. analysis of results in 100 patients. Ann Surg 203:525–530. https://doi.org/10.1097/00000658-198605000-00012
Yamataka A, Kaneyama K, Fujiwara N et al (2009) Rectal mucosal dissection during transanal pull-through for Hirschsprung disease: the anorectal or the dentate line? J Pediatr Surg 44:266–269. https://doi.org/10.1016/j.jpedsurg.2008.10.054(discussion 270)
Miyano G, Koga H, Okawada M et al (2015) Rectal mucosal dissection commencing directly on the anorectal line versus commencing above the dentate line in laparoscopy-assisted transanal pull-through for Hirschsprung's disease: prospective medium-term follow-up. J Pediatr Surg 50:2041–2043. https://doi.org/10.1016/j.jpedsurg.2015.08.022
Hollwarth ME, Rivosecchi M, Schleef J et al (2002) The role of transanal endorectal pull-through in the treatment of Hirschsprung's disease: a multicenter experience. Pediatr Surg Int 18:344–348. https://doi.org/10.1007/s00383-002-0747-x
Postuma R, Corkery JJ (1976) Abnormalities of function and faecal water following the modified Soave operation for Hirschsprung's disease. Prog Pediatr Surg 9:141–154
Nasr A, Langer JC (2007) Evolution of the technique in the transanal pull-through for Hirschsprung's disease: effect on outcome. J Pediatr Surg 42:36–39. https://doi.org/10.1016/j.jpedsurg.2006.09.028(discussion 39-40)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
Oh, C., Youn, J.K., Han, JW. et al. The Patients with Hirschsprung’s Disease Who Underwent Pull-Through at Age Less than 1 Year: Longitudinal Bowel Function. World J Surg 44, 2426–2439 (2020). https://doi.org/10.1007/s00268-020-05474-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05474-6