Abstract
Background
The goal of our study was to evaluate the differences in care and clinical outcomes of patients with chest trauma between two hospitals, including one public trauma center (Pu-TC) and one private trauma center (Pri-TC).
Methods
Patients with thoracic trauma admitted from January 2012 to December 2018 at two level I trauma centers (Pu-TC: Hospital Universitario del Valle, Pri-TC: Fundación Valle del Lili) in Cali, Colombia, were included. Multivariable logistic regression was used to assess for differences in in-hospital mortality, adjusting for relevant demographic and clinical characteristics.
Results
A total of 482 patients were identified; 300 (62.2%) at the Pri-TC and 182 (37.8%) at the Pu-TC. Median age was 27 years (IQR 21–36) and median Injury Severity Score was 25 (IQR 16–26). 456 patients (94.6%) were male, and the majority had penetrating trauma [total 465 (96.5%); Pri-TC 287 (95.7%), Pu-TC 179 (98.4%), p 0.08]. All patients arrived at the emergency room with unstable hemodynamics. There were no statistically significant differences in post-operative complications, including retained hemothorax [Pri-TC 19 vs. Pu-TC 18], pneumonia [Pri-TC 14 vs. Pu-TC 14], empyema [Pri-TC 13 vs. Pu-TC 13] and mediastinitis [Pri-TC 6 vs. Pu-TC 2]. Logistic regression did, however, show a higher odds of mortality when patients were treated at the Pu-TC [OR 2.27 (95% CI 1.34–3.87, p < 0.001].
Conclusions
Our study found significant statistical differences in clinical outcomes between patients treated at a Pu-TC and Pri-TC. The results are intended to stimulate discussions to better understand reasons for outcome variability and ways to reduce it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracic trauma accounts for 10–15% of all trauma admissions and 25% of traumatic deaths [1, 2]. A significant number of thoracic trauma patients will develop pulmonary complications or require an extended-care facility [2]. Thoracic injuries are often associated with concomitant cardiac, pulmonary, abdominal, and intracranial injuries, making this a vulnerable population [3]. As a result, poor-quality trauma care or premature hospital discharge could have a significant effect on patient outcomes in this population [1]. In Cali-Colombia, this type of injury ranked in third place after traumatic brain injury (TBI) and polytrauma in the causes of death secondary to murders and in the fourth place in traffic crashes [4], see Table 1. Thanks to this reason, the regional trauma surgeons hold high expertise in this field. However, the financial and organizational crisis in the health system around the country has affected the access to surgical services in certain populations such as trauma patients.
Differences in outcomes between private and public hospitals have been explored in multiple surgical fields, including appendicitis [5, 6], glioblastoma multiforme [7], colorectal cancer [8], pancreatoduodenectomy following pancreatic cancer [9], breast cancer [10, 11] and trauma [12], see Table 2. While in high-income countries (Gross National Income (GNI) > $12,235) [13], outcomes between public and private hospitals are similar [8, 9], difference in outcomes have been reported in upper-middle income countries (GNI per capita $3956–$12,235) [5, 6, 10,11,12]. Previously, one study was done in trauma patients [12], comparing the epidemiology of traumatic injuries and mortality between two tertiary-care trauma centers (one public vs. one private) in Cali-Colombia using the Pan-American Trauma Registry. Significant differences were found between the two centers, including variations in patient employment and insurance status, severity and location of injury, and overall adjusted mortality rates, which were significantly higher in the public versus the private hospital.
Currently, there is no scientific literature that assesses the differences in the clinical outcomes between private and public hospitals for the thoracic trauma subpopulation. In fact, the level of evidence is not sufficient to infer that the differences could be attributable just by their characteristics. However, it is possible that as more studies are conducted, it can be determined if there is a relationship between better or worse clinical outcomes among both types of hospital, as seen before when these variations were evaluated in the context of the American College of Surgeons system [14]. The objective of this study was to assess the differences in care and clinical outcomes of patients with chest trauma between two hospitals, one public Trauma center (Pu-TC) and one private Trauma center (Pri-TC).
Materials and methods
Data source
We retrospectively compiled a database that included data on all patients with thoracic trauma admitted between January 2012 to December 2018 to two level I trauma centers located in Cali, Colombia; one Pri-TC: Fundación Valle del Lili (FVL), a university hospital associated with the Universidad Icesi, and one Pu-TC: Hospital Universitario del Valle (HUV), a university hospital associated with the Universidad del Valle. HUV is an academic, tertiary, and publicly funded teaching hospital with a total of 397 beds (46 adults intensive care unit beds) [15, 16]. FVL, in contrast, is a private, nonprofit academic hospital with 519 total beds for adults (85 adults intensive care unit beds) [16, 17], see Fig. 1a.
a The bar graph shows the number of hospital-beds, UCI-beds and operating rooms registered by 2019 in the Ministerio de Salud y Proteccion Social (National Ministry of Health) in the Private Trauma Center (Private TC) and Public Trauma Center (Public TC). b This bar graph shows the volume of trauma patients admitted during 2018 at the emergency service from both hospitals. Even though there were a higher volume of admissions in the Private TC, of these, just 1319/13,242 = 10% were admitted as an inpatient. On the other hand, a higher proportion were admitted as an inpatient in the Public TC (3021/4944 = 61%)
The annual trauma admission for 2018 was 4944 and 13,242, respectively, for each hospital. [Information extracted from Pan-American Trauma Registry, a joint initiative of the Pan-American Trauma Society and the International Trauma System Development Program at Virginia Commonwealth University]. Although there was a higher volume of admissions at FVL, among them only 1319 out of 13,242 patients (10%) required admission to the hospital. At HUV, in contrast, a higher proportion of patients were admitted as inpatients (3021/4944 = 61%), see Fig. 1b. Both trauma centers reflect the largest regional volumes of trauma patients in southwestern Colombia.
The differences in inpatient admissions could due to the lack of consistent availability of hospital supplies, partial functioning of hospital services, or closing of contracts in the public hospital during that year. Therefore, only severely injured patients who had in-hospital management criteria or surgery requirement were admitted at the public institution. This scenario is different in the private hospital, in which, due to its infrastructure, there are more contracts with health insurance companies who send patients with a greater diversity of traumatic injuries that go from minor to severe; that is, not all patients admitted to the emergency department at the private hospital have injuries that necessarily require admission to the hospital.
Study population
This study included adult trauma patients (aged ≥ 15 years) who were admitted to the emergency department of both trauma centers with diagnoses of chest trauma and who underwent to emergency thoracotomy (ET), resuscitative thoracotomy (RT) or median sternotomy (MS) after initial evaluation. Patients who received thoracotomy or MS after the first 24 h of admission, who were dead on arrival or who were transferred after receiving a previous a surgical intervention in another trauma center were excluded. Operative patients who underwent procedures after the first 24 h of admission were excluded in order to account for the fact that many of them were undergoing thoracotomy for the management of other complications such as retained-hemothorax or empyema, secondary to the management of traumatic hemothorax with thoracostomy (not because they had been life-threatening bleeding in progress).
Statistical analysis
Descriptive statistics were used to summarize demographic, clinical, and care provision characteristics of the study population. We used medians and interquartile ranges for non-normally distributed continuous variables and means and standard deviations for normally distributed continuous variables. Continuous variables were compared using non-parametric tests (Wilcoxon rank sum tests) and parametric tests (t tests), as warranted, depending on their distribution. Categorical variables were summarized as frequencies and percentages and were compared using χ2 tests or Fisher’s exact tests if cell counts were less than five.
In order to determine which clinical variables were associated with higher odds of mortality among patients at the two trauma centers, a multiple logistic regression analysis was performed. The variables considered for inclusion in the initial model were chosen based on the following criteria: 1. Previous reports from the literature that evaluated clinical variables associated with higher mortality in trauma and 2. Clinical criteria set by the researchers. Potential covariates were assessed during bivariate analysis, and only those with resultant p-values was less than 0.05 were included in the final model. The discriminative capacity of the final model was further tested through the use of a receiver-operator characteristic curve (ROC) (i.e. by calculation of the area under the curve).
The following variables were considered for inclusion in the initial model: trauma mechanism, systolic blood pressure (SBP), heart rate (HR), Glasgow Coma Scale (GCS), Injury Severity Score (ISS), red blood cell units transfused in the first 6 h and 24 h, fresh frozen plasma units (FFP) transfused in the first 6 and 24 h, RT, intraoperative hemorrhage and type of trauma center (public or private).
Data management and statistical analyses were performed using Stata Statistical Software: Version 14.0 (StataCorp, College Station, TX, USA). This study was approved by the Institutional Review Boards of Fundación Valle del Lili and Hospital Universitario del Valle.
Results
A total of 482 patients were included: 300 (62.2%) from the Pri-TC and 182 (37.8%) from the Pu-TC. Median age was 27 years (IQR: 21-36). 456 (94.6%) were male, and the majority had penetrating trauma [Pri-TC 287 (95.7%), Pu-TC 179 (98.4%), p 0.08]. With respect to penetrating trauma type, there was a higher proportion of gunshot wounds among patients treated in the private hospital [Pri-TC 198 (68.9%), Pu-TC 89 (50.3%), p < 0.001]. Patients arrived at the emergency room with unstable hemodynamics, slightly more unstable at the Pri-TC. All patients had severe trauma [Pri-TC median ISS 25 (IQR 16–27), Pu-TC median ISS 25 (16–25), p 0.08]; however, a large proportion of patients at the Pri-TC suffered severe trauma (ISS > 25) [Pri-TC 76 (25.3%), Pu-TC 44 (24.2%); p 0.004], see Table 3.
With respect to adjunctive procedures, 166 (34.4%) patients underwent exploratory laparotomy, with similar proportions at both trauma centers [Pri-TC 94 (31.3%), Pu-TC 72 (39.6%); p 0.06]. The following procedures were used: hepatic packing: 64 (13.3%), pelvic packing: 8 (1.7%), splenectomy: 11 (2.28%), bowel resection: 9 (1.87%), craniectomy: 3 (0.6%) and, respectively, hepatic and splenic embolization 4 (0.8%) and 2 (0.4%), without statistically significant differences between groups, see Table 4. Patients from the Pri-TC received more transfusion products in the first 6 and 24 h compared to the Pu-TC patients; respectively: first 6 h, Pri-TC [unit packed RBCs: median 4 (IQR 1–6), unit packed FFP: median 2 (IQR 0–5)], Pu-TC [unit packed RBCs: median 2 (IQR 0–4), unit packed FFP: median 0 (IQR 0–2)]; p < 0.001. First 24 h: Pri-TC [unit packed RBCs: median 4 (IQR 1–6), unit packed FFP: median 3 (IQR 0–6)], Pu-TC [unit packed RBCs: median 2 (IQR 0–4), unit packed FFP: median 0 (IQR 0–2)]; p < 0.001. Nevertheless, the Pu-TC patients received less volume of crystalloids in the first 24 h [Pri-TC median 4500 mL (IQR 3000–6700), Pu-TC 1000 mL (IQR 500–2000); p < 0.01], see Table 5.
Regarding the surgical approach performed for the management of thoracic injuries, the left anterolateral thoracotomy was used more frequently [Pri-TC 203 (75.8%) and Pu-TC 146 (85.4%); p 0.01]. Other surgical approaches were also used: bilateral anterolateral thoracotomies in 24 (5.5%) patients and MS in 43 (8.9%) patients. 189 (39.2%) patients received RT, 104 (34.7%) in the Pri-TC and 85 (46.7%) in the Pu-TC, with a statistically significant difference between groups of p = 0.009. More patients in the Pu-TC required conversion of surgical incision [Pri-TC 38 (12.7%) patients, Pu-TC 37 (20.3%) patients; p 0.02], among these the contralateral thoracotomy and clamshell thoracotomy were the surgical incisions additional used with more frequency in both groups [Pri-TC: contralateral thoracotomy: 22 (57.9%), clamshell thoracotomy: 11 (28.9%), trapdoor thoracotomy: 3 (7.9%), MS: 2 (5.3%) and Pu-TC: contralateral thoracotomy: 10 (27.0%), clamshell thoracotomy: 22 (59.5%), trapdoor thoracotomy: 0 (0%), MS: 4 (13.5%); p 0.004], see Table 6.
In the Pu-TC a higher proportion of patients required resuscitation and hemorrhage control procedures compared to Pri-TC [Pri-TC: cardiac massage: 123 (41.0%), release of cardiac tamponade: 37 (12.3%), aortic occlusion: 115 (38.3%) and Pu-TC: cardiac massage: 93 (51.1%), release of cardiac tamponade: 44 (24.2%), aortic occlusion: 99 (54.4%), p 0.001]. Other characteristics referent to anatomic severity like intraoperative hemorrhage (mL), AAST lung, heart, thoracic vascular scales (Grade III and Grade IV) and damage control surgery in thorax were similar between the groups, see Table 6.
Multiple clinical outcomes were evaluated in both trauma centers, the proportion of patients that presented multiorgan failure on the day 2 measured by SOFA scale was 71 (14.7%) patients, without a statistically significant difference between groups [Pri-TC 52 (17.3%), Pu-TC 19 (10.4%); p 0.27]. Less than 10% of patients presented clinical complications like acute kidney injury, adult respiratory distress syndrome, bacteremia, pneumonia, sepsis, retained hemothorax, empyema and mediastinitis, without statistically significant differences in both groups, see Table 7. However, Intensive Care Unit length of stay [Pri-TC median 2 days (IQR 0–6), Pu-TC median 0 days (0–2); p < 0.001] and, Hospital length of stay [Pri-TC median 6 days (IQR 1–13), Pu-TC median 4 days (IQR 1–12); p 0.02] were higher in the Pri-TC when it was compared with the Pu-TC.
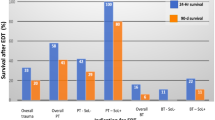
More than a third of patients died [212 (43.9%) patients], a higher proportion of in-hospital mortality was reported in the Pu-TC [Pu-TC 96 (52.7%), Pri-C 116 (38.7%); p 0.003], with differences that were statistically significant. 186 (38.6%) of the patients died in the first twenty-four hours, 106 (35.3%) in the Pri-TC and 96 (52.7%) in the Pu-TC; p value: 0.25. A major proportion of patients died inside the Operating Room (OR) [Pri-TC OR 92 (79.3%), ICU 24 (20.7%), Ward 0 (0%) and Pu-TC OR 78 (82.1%), ICU 11 (11.6%), Ward 6 (6.3%); p 0.004]. At discharge, 210 (43.6%) of the patients were neurologically intact (measured by Glasgow Outcome Scale), with a significative proportion in the Pri-TC [Pri-TC 134 (44.7%), Pu-TC 76 (41.8%); p < 0.001], see Table 7.
Multiple logistic regression analysis adjusted for relevant demographic and clinical characteristics demonstrated that the odds for death was higher when patients were treated at a Pu-TC [OR 2.27 (95% CI 1.34–3.87, p < 0.001]. Logistic regression model had an Area under ROC curve of 87.2%, see Table 8, Fig. 2.
Discussion
In our study, we compared clinical outcomes, surgical complications and mortality in patients with severe thoracic trauma between two trauma centers (one Public TC and one Private TC) in Colombia. We found significant differences in the patients’ characteristics and management strategies including: hemodynamic status on arrival at the emergency room, severity, resuscitation requirements, surgical procedures, and odds of mortality, which were significantly higher at the public versus private trauma center, after adjusting for potential confounders. Although the structural differences between the two trauma centers were not objectively evaluated, this study demonstrated that there was a higher probability of having unfavorable clinical outcomes when chest trauma patients received management in the public institution. However, these findings should not be generalized to other public institutions or different patient populations. As every health system varies depending on the country, more topics must be investigated in this field to strengthen the trauma systems and contribute to decrease or delete these disparities.
There were significant differences in the hemodynamic status on arrival at the emergency room between both hospitals; patients from Pri-TC were more hypotensive, tachycardic and with lower Glasgow scores. These findings contrast with a previous study that compared these centers within the Pan-American Trauma Registry and showed no statistically significant difference in these variables [12]. The reason why patients from the Pri-TC arrived more unstable could be attributed to a higher proportion of patients presenting with severe trauma (ISS ≥ 25). However, due to its location, this center receives more patients from rural areas and other smaller cities in the southern part of the catchment region. This factor implies that those patients who are transferred from these places arrive first at primary care centers (located in the same region where the patient got injured or so close) until they are transferred to a level I trauma center for definitive management. Therefore, there is a delay due to this in interventions such as early transfusion, surgery and an increase in the prehospital transport time (transport usually takes 30 min or more).
Brown et al. [18], evaluated the relationship of fatal motor vehicle collision (MVC) rates and the distance from individual MVC locations to the nearest trauma system resources (TSR) in Pennsylvania-USA. Their analysis demonstrated that fatal MVC rates are higher in geographic areas with fewer TSR nearby. The fatal MVC rate increased 0.141 per 100 million vehicle miles traveled for every 10 miles farther from the nearest TSR (p < 0.01). Another study by Adzemovic et al. [19] showed that trauma patients presenting initially to a Level III/IV trauma setting, subsequent interfacility transfer to a level I/II trauma center was associated with survival benefit for patients with moderate and severe TBI, particularly with CT finding of hemorrhage, pelvic fracture, penetrating thoracic mechanism, complex solid organ injury, great vessel injury, emergency department respiratory distress, and tachycardia at presentation. Almost 60% of patients derived survival benefit from transfer to a Level I/II trauma center. Approximately half of patients admitted to a level III/IV trauma centers potentially would have benefited from transfer. This has special importance when we contrast these findings in our study, especially because many of our patients arrived first to low complexity primary care centers non-verified in trauma management. And even though the transferred status was not reported in our results which is one limitation, in Cali is known that a high proportion of severely injured patients are not transported directly to high complexity trauma centers (HUV/FVL) due to lack of consensus between the prehospital personnel to allocate trauma patients to verified trauma hospitals and because some ambulances are financed to get patients in hospitals (usually, not verified trauma centers) which have contracts with health insurance companies who pays especially for traffic crashes patients.
The discrepancy in mortality is not completely explained by the variables included in the model; however, in the public hospital there was a higher proportion of patients with resuscitative thoracotomy and lower hemostatic resuscitation. Other contributing factors identified by clinicians include delays in patient transfer to public hospital (which typically takes patients not accepted at other institutions), delayed or poorly communicated transfer between pre-hospital, emergency room, ICU and operative settings and political or financial instability as a public hospital. Also, this center has more limited medical supplies and less access to 24-hour specialist services such as interventional radiology.
The limitations of this analysis include its retrospective nature and moreover, this is a single experience limited to two hospitals around the country, which limits the external validity of these findings. Furthermore, all data were entered into the electronic medical record system, often based on available information from existing medical records, which itself is a process prone to omission error. While several key predictors of trauma mortality were included in the database, other contributing features, such as level of provider training, time and distance to hospital, pre-hospital information, time to or cause of death, were not included. Finally, our study focused on two hospitals, one public and one private, in one province of Colombia. The findings seen here, which emblematic of the challenges faced by the trauma system in Cali, might not be generalizable to other hospitals or regions of Colombia or Latin America.
In addition, these patients require a whole organization within the trauma system which guarantees access to the elements that ensure the success of the clinical interventions, based on hemorrhage control and resuscitation strategies, such as: assessment and early diagnosis by a multidisciplinary trauma team (trauma nursing, emergency medicine attendings, trauma and acute care surgeons with endovascular training, anesthesiologists), availability of radiology rooms and permanent equipment of interventional radiology, rapid response of the blood bank, ICU beds accessible, equipment and technology for hemodynamic monitoring and optimal times in surgical reinterventions.
Conclusion
We found significant differences in mortality and clinical outcomes in patients with thoracic trauma between a Pu-TC and a Pri-TC in Cali. This study opens the discussion to identify key factors that could be driving these differences and define targets for potential interventions to reduce this gap.
References
Haines KL, Zens T, Beems M, Rauh R, Jung HS, Agarwal S (2018) Socioeconomic disparities in the thoracic trauma population. J Surg Res [Internet] [cited 2019 Apr 13] 224:160–165. http://www.ncbi.nlm.nih.gov/pubmed/29506834
Ziegler DW, Agarwal NN (1994) The morbidity and mortality of rib fractures. J Trauma [Internet]. [cited 2019 Apr 13]; 37(6):975–979. http://www.ncbi.nlm.nih.gov/pubmed/7996614
Richardson JD, McElvein RB, Trinkle JK (1975) First rib fracture: a hallmark of severe trauma. Ann Surg [Internet]. [cited 2019 Apr 13]; 181(3):251–254. http://www.ncbi.nlm.nih.gov/pubmed/1130843
Instituto Nacional de Medicina Legal y Ciencias Forenses. Forensis. Datos para la vida. [Internet]. http://www.medicinalegal.gov.co/cifras-estadisticas/forensis
Coelho JCU, Fernandes FM, Cortiano LGG, Leme GM de O, Sadowski JA, Artner CL Appendectomy. Comparative study between a public and a private hospital. Rev Assoc Med Bras [Internet]. [cited 2019 Sep 5]; 56(5):522–527. http://www.ncbi.nlm.nih.gov/pubmed/21152822
Yang E, Cook C, Kahn D (2015) Acute appendicitis in the public and private sectors in Cape Town, South Africa. World J Surg 39(7):1700–1707. https://doi.org/10.1007/s00268-015-3002-z
Loureiro LVM, Pontes LDB, Callegaro-Filho D, Koch LDO, Weltman E, Victor EDS et al (2014) Initial care and outcome of glioblastoma multiforme patients in 2 diverse health care scenarios in Brazil: Does public versus private health care matter? Neuro Oncol 16(7):999–1005
Bokey L, Chapuis PH, Keshava A, Rickard MJFX, Stewart P, Dent OF (2015) Complications after resection of colorectal cancer in a public hospital and a private hospital. ANZ J Surg 85(3):128–134
Chua TC, Mittal A, Nahm C, Hugh TJ, Arena J, Gill AJ et al (2018) Pancreatoduodenectomy in a public versus private teaching hospital is comparable with some minor variations. ANZ J Surg 88(6):E526–E531
Coetzee WC, Apffelstaedt JP, Zeeman T, Du Plessis M (2018) Disparities in breast cancer: private patients have better outcomes than public patients. World J Surg 42(3):727–735. https://doi.org/10.1007/s00268-017-4187-0
Kong YC, Bhoo-Pathy N, Subramaniam S, Bhoo-Pathy N, Taib NA, Jamaris S et al (2017) Advanced stage at presentation remains a major factor contributing to breast cancer survival disparity between public and private hospitals in a middle-income country. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph14040427
Ramachandran A, Ranjit A, Zogg CK, Herrera-Escobar JP, Appelson JR, Pino LF et al (2017) Comparison of epidemiology of the injuries and outcomes in two first-level trauma centers in Colombia using the Pan-American trauma registry system. World J Surg [Internet]. [cited 2019 May 9]; 41(9):2224–2230. http://www.ncbi.nlm.nih.gov/pubmed/28417184
The world bank in middle income countries [Internet]. 2018 [cited 2019 Sep 24]. https://www.worldbank.org/en/country/mic/overview#1
Herrera-Escobar JP, Rios-Diaz AJ, Zogg CK, Wolf LL, Harlow A, Schneider EB et al (2018) The “mortality ascent”: hourly risk of death for hemodynamically unstable trauma patients at Level II versus Level i trauma centers. J Trauma Acute Care Surg 84(1):139–145
Torres I (2018) Informe de gestion [Internet]. Cali-Colombia. http://www.huv.gov.co/web/RENDICION CUENTAS HUV 2018/CONSOLIDADO INFORME FINAL 2018.pdf
Capacidad instalada habilitada de los prestadores de servicios de salud del departamento del valle del cauca [Internet]. 2018. https://www.datos.gov.co/Salud-y-Protecci-n-Social/Capacidad-Instalada-Habilitada-De-Los-Prestadores-/btgx-v74p
Informe de sostenibilidad [Internet]. Cali-Colombia; 2018. http://valledellili.org/wp-content/uploads/2019/04/Informe-anual-2018-web.pdf
Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL (2017) Distance matters: effect of geographic trauma system resource organization on fatal motor vehicle collisions. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000001508
Adzemovic T, Murray T, Jenkins P, Ottosen J, Iyegha U, Raghavendran K et al (2019) Should they stay or should they go? Who benefits from interfacility transfer to a higher-level trauma center following initial presentation at a lower-level trauma center. J Trauma Acute Care Surg [Internet]. [cited 2019 Jul 15]; 86(6):952–960. http://insights.ovid.com/crossref?an=01586154-201906000-00003
Acknowledgements
We want to thank for their hard work and dedication building this paper to Dr. Edison Angamarca, Dr. Marisol Badiel, Dr. Adil Haider, Dr. Mario Alain Herrera and our great team of medical students: Angelica Rojas, Tatiana Méndez and Mateo Betancourt. Each contribution during the process, such as designing the research question, write the protocol, collect the data, running the statistical analysis and interpreting our results critically and accurately was supported continuously by each one of them. As well, we thank Dr. Marcela Granados, who has propounded for support and stimulate the collaborative research between these two institutions.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Orlas, C.P., Herrera-Escobar, J.P., Zogg, C.K. et al. Chest Trauma Outcomes: Public Versus Private Level I Trauma Centers. World J Surg 44, 1824–1834 (2020). https://doi.org/10.1007/s00268-020-05400-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05400-w