Abstract
Introduction
New training programs face quality concern by faculty who believe resident involvement in operative management may lead to poorer outcomes. This study aims to understand the impact of resident surgeons on outcomes in a specific common surgical procedure.
Methods
We obtained a retrospective review of 1216 laparoscopic cholecystectomy cases between June 2012 and June 2017 at a community teaching hospital. Data reviewed included patient demographics, operative time, length of stay, 30-day outcomes. An initial analysis comparing outcomes with/without resident participation was undertaken. A subset analysis comparing junior (PGY 1–2) and senior (PGY 3–5) groups was also performed.
Results
We found the resident group participated in higher-risk patient (ASA > 3, 47.5% vs 39.8%, p = 0.04 more acute disease (59.8% vs 37.5%, p < 0.0001) and emergent surgery (59.7% vs 37.5%, p < 0.0001). Resident involvement in severe cases was not a significant factor in the odds of morbidity, mortality, conversion rate or length of stay. Resident participation did increase the odds of having longer OR time (OR 12.54, 95% CI 7.74–17.34, p < 0.0001).
Conclusions
Resident participation is associated with increased operative times but not complications. This study confirms resident participation in the operating room in difficult and challenging cases is safe.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Some might consider that the involvement of a surgeon-in-training is associated with negative impact on procedural outcomes [1, 2]. This is especially true in newer community hospital training programs, whose faculty have not been trained in resident education. The ongoing balance of quality and patient safety and resident education is a challenge for current surgical programs.
This retrospective, single-institution study was designed to evaluate the impact of resident as well as the level of postgraduate medical training on outcomes in laparoscopic cholecystectomy. As a matter of both quality and safety, it is increasingly important to consider resident involvement and competency in surgical case management without compromising the quality of patient care.
Methods
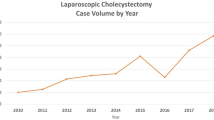
To understand the effects of resident involvement in surgical care, we performed a retrospective review of all patients who underwent laparoscopic cholecystectomy between June 1, 2012, and June 1, 2017, at a community teaching hospital. This hospital’s surgical residency program began in 2012. Cases were identified using Current Procedural Terminology (CPT) codes: 47562 (laparoscopic cholecystectomy without cholangiography), 47563 (laparoscopic cholecystectomy with cholangiography) and 47564 (laparoscopic cholecystectomy with exploration of the common bile duct). Intraoperative cholangiogram was routinely performed in patients whom met any of the following criteria: history of elevated bilirubin, gallstone pancreatitis, cholelithiasis, dilated common bile duct on preoperative imaging, indeterminate intraoperative anatomy of common bile duct. Acute cholecystitis included calculus, acalculous cholecystitis and acute-on-chronic cholecystitis. Patient who presented with right upper quadrant pain and acute cholecystitis confirmed on preoperative imaging (positive Murphy sign, pericholecystic fluid, gallbladder wall thickening) was considered acute cholecystitis. Cases admitted from the emergency room or transferred from another facility and operated 24 h within admission were categorized as emergent surgery. Cases were excluded when cholecystectomy was a part of another procedure, patients were younger than 18 years old, and patients were with inadequate data. The review yielded 1216 cases which were eligible for evaluation. The cases were divided into 2 groups based on if a resident was a part of the procedure or if the case was done by the attending alone. The resident cohort was further subdivided into 2 groups based on postgraduate year (PGY) of clinical training in surgery: junior group (PGY 1, 2) and senior group (PGY 3, 4, 5). The extent of resident involvement in the operation was not available from the operative note, but in general there was a graded increase in intraoperative role of residents as they progressed from PGY 1 through PGY 5.
Patient demographics were also reviewed, and gender, age, American Society of Anesthesia status classification (ASA), body mass index (BMI), previous surgery, the urgency of the case, concomitant pancreatitis, laboratory values (white blood cell count WBC, total bilirubin), imaging findings (ultrasound, CT scan, MRCP, HIDA), pathology, postoperative complications, resident year level, simultaneous procedures (intraoperative cholangiogram, perioperative ERCP) and rate of conversion to an open procedure were recorded. The primary outcome studied was total operative time. Secondary outcomes considered included the length of stay, complications and rate of conversion to open. Complications were categorized as respiratory, cardiology, gastrointestinal, genitourinary tract and infection. Clavien–Dindo classification was utilized to grade the severity of complication. Operative time was calculated as the time from the first incision to the time of skin closure. Length of stay was calculated from the date of operation to date of discharge.
Statistical analysis was performed using IBM SPSS Statistics 23 software (IBM Inc., Armonk, NY, USA). A p value < 0.05 was considered statistically significant. Multiple logistic regression was used to evaluate resident involvement while accounting for patient demographic, urgency of operation. The study was approved by the institutional review board for human studies.
Results
Patient demographics and clinical characteristics (Tables 1 and 2)
A total of 1216 patients were evaluated. We found 1000 patients in resident group and 216 patients in non-resident group. There were no significant differences in patient demographics including age, gender, morbid obesity (BMI > 30) and prior abdominal surgery. However, the resident group was more likely to participate in high-risk patients (ASA > 2, 47.5% vs 39.8%, p = 0.04), patients with acute cholecystitis (59.8% vs 37.5%, p < 0.0001) and patients requiring emergent surgery (59.7% vs 37.5%, p < 0.0001). The resident group was also more likely to operate on more complicated cases, cholelithiasis (77.6% vs 71.3%, p < 0.0001), gallbladder wall thickening more than 4 mm (35.5% vs 26.9%, p = 0.015), pericholecystic fluid (20.8% vs 14.4%, p = 0.03) and dilated CBD (1.89% vs 1.59%, p = 0.003). The patients in the resident group also exhibited higher preoperative white blood cell count (WBC > 12,000) (26.3% vs 19.9%, p = 0.05) and elevated total bilirubin (23.50% vs 13.50%, p = 0.001). Additionally, perioperative ERCP procedure was carried out more frequently in the resident group (18.7% vs 8.3%, p < 0.0001). These findings suggest that residents at this training program are involved in patients with more complicated diseases than patients operated by faculty alone.
Operative details and outcomes (Table 3)
Both the resident and non-resident groups utilized intraoperative cholangiogram equally (48.4% vs 47.2%, p = 0.75). To eliminate the potentially confounding effect on operative time, cases with and without intraoperative cholangiogram were compared separately in each group. The resident group had a longer operative time in both patients who had a cholangiogram (75.09 min vs 58.81 min, p < 0.0001) and without cholangiogram (74.71 min vs 60.40 min, p < 0.0001). The conversion rate to open was also higher in resident group (4.1% vs 0.9%, p = 0.02). The length of stay was longer with the resident group (2.67 days vs 1.69 days, p = 0.02), which may reflect the severity of illness. There does not appear to be a statistical difference in complications (7.9% vs 4.6%, p = 0.09) or mortality (0.1% vs 0%, p = 0.64) between the group of resident involvement and the faculty alone group. There were total 79 (7.9%) major surgical complication in resident group and 10 (4.6%) in non-resident group. All major injuries included in the study required operative intervention, interventional radiology or hospital admission until resolution of symptoms. There were total 36 injuries (3.6%) requiring treatment with ERCP stenting. There was 1 death (0.08%), due to bleeding secondary from undiagnosed coagulopathy.
Additional factors related to outcomes (Table 4)
On multivariable logistic regression analysis, resident participation was strongly associated with increased operative time (OR 12.58; 95% CI 7.86–17.30; p < 0.0001). However, resident involvement was not a significant factor in the odds of morbidity (OR 1.29; 95% CI 0.64–2.58; p = 0.5), conversion rate (OR 3.17; 95% CI 0.75–13.42; p = 0.12) or length of stay (OR 1.07; 95% CI 0.7–1.63; p = 0.74). Only the urgency of surgery and patient comorbidity were predictive factors for increased length of stay. Similarly, acute cholecystitis and patient ASA status were associated with complication, conversion to open.
Postgraduate year
A further subset analysis comparing 535 patients in the senior group (PGY 3–5) and 465 patients in the junior group (PGY 1–2) was performed. No statistical significance in patient demographics was noted between the senior and the junior groups. The senior group was more likely to participate in acute cholecystitis (64.3% vs 54.6%, p = 0.002) and emergent surgery (64.5% vs 54.2%, p = 0.001). Participation of senior residents was also associated with longer operative time (78 min vs 71.7 min, p = 0.003) and was more pronounced in cases needing intraoperative cholangiogram (81.49 min vs 65.43 min, p < 0.0001). Multivariable logistic regression analysis revealed that acute cholecystitis (OR 10.84; 95% CI 4.89–16.78; p < 0.0001), gallbladder wall thickening (GBW > 4) (OR 7.64; 95% CI 2.75–12.52; p = 0.002) and senior participation (OR 5; 95% CI 0.98–9.04; p = 0.015) were predictive factors for longer operative time. The senior group also was associated with a longer length of stay (LOS > 2) (3.09 days vs 2.17 days, p = 0.008). Multivariable logistic regression analysis revealed that the urgency of operation was associated with increased length of stay (LOS > 2) (OR 15.17; 95% CI 8.78–26.21; p < 0.0001). There does not appear to be a difference in the rate of conversion to open (5.2% vs 2.8%, p = 0.06) or complications (8.8% vs 6.9%, p = 0.27) between the senior and the junior groups.
Discussion
Since its implementation in 1987, laparoscopic cholecystectomy has quickly become standard of care for gallbladder diseases in the USA [2]. An estimated number of 500,000 inpatient cholecystectomies are performed every year in the USA [3]. Including inpatient and outpatient cases, the number is likely closer to 1,000,000, making cholecystectomy one of the most common general surgical procedures, not only in the USA but globally as well [4, 5]. We focused on laparoscopic cholecystectomy, as it is an essential component for surgical resident training. A similar retrospective analysis performed by Carson et al. [6] also showed that a higher portion of the total cases performed by US general surgery residents between 1999 and 2008 were minimally invasive procedures (3.7–11.1%, p < 0.0001). Minimally invasive surgery continues to evolve and is quickly becoming the standard of care in surgery. Continued evaluation of the effects of resident involvement is especially true in an era of value-based reimbursement.
This study implies that resident involvement in laparoscopic cholecystectomy does not negatively affect patient outcomes. These findings are in concert with other studies which have shown inclusion of minimally invasive surgery in resident training is safe [7, 8]. Jolley et al. [9] in a review of 37,636 laparoscopic cholecystectomies performed between 2010 and 2011 from American College of Surgeons National Surgical Quality Improvement Program Database (ACS/NSQIP) concluded that resident involvement did not result in significantly higher mortality or morbidity. A small retrospective study by Kauvar et al. [10], however, indicated that patients operated by residents experienced operative complications more frequently. This study, however, was a retrospective study of a small patient population (300 patients) and was not adjusted for confounding factors such as emergent cases, attending experience.
This study indicates that while residents tend to operate on complicated gallstone diseases, there is no statistical difference in morbidity and mortality. Here, analysis is complicated by the fact that it is difficult to determine the scope of both resident and attendings performance of critical parts of the procedure. One of the limitations of this paper is the low number of cases in the faculty group. The low complication rate in this study (7.9%) may result in no significant difference between resident and faculty groups, especially due to the low number of cases in the faculty group.
Despite the fact the rate of conversion to open is significantly higher in the resident group, resident participation does not appear to increase the odds of conversion in multivariate analysis. All of the emergent cases were operated by the resident group, which could explain the increased rate of conversion to open in the resident group.
Similar to other analyses, our study shows that resident participation is associated with longer operative times [11, 12]. In a large study of the NSQIP database, Davis et al. [12] found that laparoscopic cholecystectomy performed by residents lengthened operative time by 47.7% from 44–65 min. Their study also found no difference in operative times between any levels of resident or fellow training.
One might expect a significant decrease in operative time as PGY training level increases. Johnson et al. [13] observed a 2.6-min decrease in operative time for laparoscopic cholecystectomy as postgraduating year of the operating resident increased. A small study by Wang et al. [14] did not find any difference in operative time with increasing postgraduating year level. In addition, Kauvar et al. [10] noted no difference in operative time based on the level of attending seniority. In this study, senior residents had the longest operative times. Senior residents at our institution tend to operate on emergent and cases with higher level of complexity, which most likely contributes to the increased operative time. The previous analysis has found that increased operative time does not appear to be associated with increased complications [15,16,17]. This study confirms these findings. Although the increased operative times are statistically significant, operative time does not appear to be clinically important [18].
Even though increased operative time is not implicated in additional morbidity and mortality for the patients, longer operative times may result in increased cost of care [19]. This study demonstrated longer length of stay with resident participation on univariate analysis. Recognizing that this result is confounded by other important variables, we performed a multivariate analysis which revealed only emergent surgery and patient’s performance status (ASA > 2) were predictive factors for increased length of stay. The resident participation would not appear to increase the cost of care.
This study has several limitations. The retrospective nature of the study allows for selection bias. The presence of confounding variables, both measured and unmeasured, also may contribute to a selection bias. Resident selection for cases was likely based on projected difficulty of the case which may not represent the true difficulty of the case. Residents also tend to participate in complicated cases leading to an inherent selection bias.
Learning in the operating room is important to residents becoming competent to perform surgery. However, the current healthcare environment demands optimization of patient outcomes in addition to maximal cost efficiency. It has already proven that resident participation to surgery increases operating time, therefore increasing the hospital cost. Unfortunately, this is one of the main reasons why many teaching hospitals must struggle between keeping the budget and offering proper training. Recent studies have shown that the key to reducing operating time and efficiency may lie in simulated training and feedback. Fulton et al. [20] found that simulation-based training improves resident skills in ultrasound guided biopsy in terms of overall procedure time, number of skin punctures and needle adjustments and subjective performance. Similarly, study of Egle et al. [21] demonstrated that after simulation-based training, residents performed vascular and bowel anastomoses more adeptly, quickly, and with a higher quality end product. Laboratory training can effectively improve residents’ ability to perform anastomoses, which may result in increased efficiency in the operating room. Panait et al. [22] found that completion of their structured laparoscopic simulation curriculum results in improved advanced laparoscopic skills in senior residents as measured by Fundamental Laparoscopic Skill scores. Interestingly, this skill improvement was independent of laparoscopic case experience. They suggest that continuing to mandate the use of this skills curriculum should improve residents’ performance in advanced laparoscopic surgical procedures. These studies advocate that structured surgical simulation programs can help surgical training by facilitating the residents transitioning from simulated to real-case scenarios.
Conclusions
This study demonstrates that resident involvement in commonly performed minimally invasive surgical procedures is safe and does not adversely affect quality of care. Although resident involvement seems to be associated with longer operative time, the morbidity and mortality were not significantly affected by resident involvement. Increased operative time for more senior residents may be suggestive of the severity of disease and not resident skill of level. Learning in the operating room is essential to the development of surgical competence. This study confirms resident involvement in the operating room is both safe and effective.
References
George BC, Bohnen JD, Williams RG et al (2017) Readiness of US general surgery residents for independent practice. Ann Surg 266(4):582–594
Loiero D, Slankamenac M, Clavien PA, Slankamenac K (2017) Impact o residency training level on the surgical quality following general surgery procedures. World J Surg 41(11):2653–2666. https://doi.org/10.1007/s00268-017-4092-6
Weiss AJ, Elixhauser E (2014) Trends in operating room procedures in US hospitals, 2001–2011. Agency for healthcare research and quality’s healthcare cost and utilization project. Stat Brief 171:1–14
Fogel EL, Sharman S (2015) Diseases of the gallbladder and bile ducts. In: Goldman L, Schafer AI (eds) Goldman cecil medicine. Elsevier, pp 1038–1048. E 1033
Urbach DR, Stukel TA (2005) Rate of elective cholecystectomy and the incidence of severe gallstone disease. CMAJ 172(8):1015–1019
Carson JS, Smith L, Are M (2011) National trends in minimally invasive and open operative experience of graduating general surgery residents: implications for surgical skills curricula development? Am J Surg 202:720–726
Kazaure HS, Roman SA, Sosa JA (2012) The resident as surgeon: an analysis of ACS-NSQUIP. J Surg Res 178:126–132
Ibrahim S, Tay KH, Lim SH et al (2008) Analysis of a structured training program in laparoscopic cholecystectomy. Langenbecks Arch Surg 393:943–948
Jolley J, Lomelin D, Simorow A (2016) Resident involvement in laparoscopic procedures does not worsen clinical outcomes but may increase operative times and length of hospital stay. Surg Endosc 30:3783–3791
Kauvar DS, Braswell A, Brown BD et al (2006) Influence of resident and attending surgeon seniority on operative performance in laparoscopic cholecystectomy. J Surg Res 132:159–163
Maqsood H, Buddensick TJ, Patel K (2016) Effect of residents on operative time and complications: Focus on laparoscopic cholecystectomy in the community. J Surg Educ 73(5):836–843
Davis SS, Husain FA, Lin E et al (2013) Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg 216:96–104
Johnson JJ, Thurman JB, Garwe T et al (2013) Variations in procedure time based on surgery resident postgraduate year level. J Surg Res 185:570–574
Wang WN, Melkonian MG, Marshall R et al (2001) Postgraduate year does not influence operating time in laparoscopic cholecystectomy. J Surg Res 101:1–3
Hardy KL, Davis KE, Constantine RS et al (2014) The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Asthet Surg J 34(4):614–622
Fogarty BJ, Khan K, Ashall G et al (1999) Complications of long operations: a prospective study of morbidity associated with prolonged operative time (>6 h). Br J Plast Surg 52(1):614–622
Tseng WH, Jin L, Canter RJ et al (2011) Surgical resident involvement is safe for common elective general surgery procedure. J Am Coll Surg 213:19–26
Chen W, Sailhammer E, Berger DL et al (2007) Operative time is a poor surrogate for the learning curve in laparoscopic colorectal surgery. Surg Endosc 21:238–243
Hwang CS, Pagano CR, Wichterman KA et al (2008) Resident versus no resident: a single institutional study on operative complications, mortality, and cost. Surgery 144(2):339–344
Fulton N, Buethe J, Gollamudi J et al (2016) Simulation-based training may improve resident skill in ultrasound-guided biopsy. AJR Am J Roentgenol 207(6):1329–1333
Egle JP, Malladi SV, Gopinath N et al (2015) Simulation training improves resident performance in hand-sewn vascular and bowel anastomoses. J Surg Educ 72(2):291–296
Panait L, Hogle NJ, Fowler DL et al (2011) Completion of a novel, virtual-reality-based, advanced laparoscopic curriculum improves advanced laparoscopic skills in senior residents. J Surg Educ 68(2):121–125
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interes
tAll of authors have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nasri, B., Saxe, J. Impact of Residents on Safety Outcomes in Laparoscopic Cholecystectomy. World J Surg 43, 3013–3018 (2019). https://doi.org/10.1007/s00268-019-05141-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05141-5