Abstract
Background
Indocyanine green (ICG) is a near-infrared fluorescent contrast agent, which preferentially accumulates in cancer tissue. The aim of our study was to investigate the role of fluorescence imaging (FI) with ICG (ICG-FI) for detecting peritoneal carcinomatosis (PC) from colorectal cancer (CRC).
Methods
Four CRC patients with PC scheduled for cytoreductive surgery + hyperthermic intraperitoneal chemotherapy were enrolled in this prospective study. At a median time of 50 min after 0.25 mg/kg ICG injected intravenously, intraoperative ICG-FI using Fluobeam® was performed in vivo and ex vivo on all specimens. The Peritoneal Cancer Index was used to estimate the likelihood of complete cytoreduction.
Results
No severe complications were recorded. ICG-FI took a median of 20 min (range 10–30, IQR 15–25). Sixty-nine nodules were harvested. Fifty-two nodules had been diagnosed preoperatively by conventional imaging (n = 30; 43%) or intraoperatively by visual inspection/palpation (n = 22; 32%). With ICG-FI, 47 (90%) nodules were hyperfluorescent, and five hypofluorescent. Intraoperative ICG-FI identified 17 additional hyperfluorescent nodules. On histopathology, 16 were metastatic nodules. Sensitivity increased from 76.9%, with the conventional diagnostic procedures, to 96.9% with ICG-FI. The positive predictive value of ICG-FI was 98.4%, and test accuracy was 95.6%. Diagnostic performance of ICG-FI was significantly better than preoperative (p = 0.027) and intraoperative conventional procedures (p = 0.042). The median PCI score increased from 7 to 10 after ICG-FI (p < 0.001).
Conclusions
Our results suggest that intraoperative ICG-FI can improve outcomes in patients undergoing CS for PC from CRC. Further studies are needed to determine the role of ICG-FI in this patient population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with peritoneal carcinomatosis (PC) from gastrointestinal cancer generally have a dismal prognosis [1]. Peritoneal metastases occur in 30–40% of patients with colorectal cancer (CRC) and are the only metastases in 25% of patients [2, 3]. Peritoneal involvement is judged as the most serious event in tumor progression [4]. If untreated, patients have a median survival of ≤ 6 months after diagnosis [5]. The only potentially curative treatment in these cases is cytoreductive surgery (CS) with hyperthermic intraperitoneal chemotherapy (HIPEC) with a 5-year survival rate ranging from 30 to 48%, in selected cases [6,7,8,9,10]. Since PC is considered a kind of regional metastasis, and it is impossible to remove all microscopic residues, the concept of radicality is relative, so that not only complete cytoreduction, CC-0, but also CC-1 (residual tumor < 2.5 mm) is acceptable [11].
The diagnosis of PC is challenging, both pre- and intraoperatively. Computed tomography (CT) and positron emission tomography (PET) scans give the best results preoperatively, but underestimation of the disease stage is frequent [12]. During laparotomy, surgeons depend on visual inspection and palpation, to determine the extent of PC and the extent of the resection. However, some subclinical peritoneal lesions may escape intraoperative detection.
The Peritoneal Cancer Index (PCI) is of key importance in planning treatment and closely related with prognosis after CS + HIPEC [13]. In patients with PC from CRC, a PCI of 10–20 means extensive carcinomatosis and therefore a worse prognosis and patients with a PCI > 20 should be treated only palliatively [14,15,16,17].
In recent years, new technology has made it possible for surgeons to detect smaller lesions [18, 19]. Intraoperative fluorescence imaging (FI) is a recently introduced imaging modality that may improve detection of PC [20]. Indocyanine green (ICG), a near-infrared contrast agent becoming fluorescent if excited by light with a wavelength of 800–900 nm, has been recently proposed for FI because of its special affinity for cancer tissue [21, 22]. Bound to serum proteins, ICG works as a macromolecule permeating endothelial fissures and is retained in cancer tissue because of impaired lymphatic drainage [enhanced permeability and retention (EPR)] from the lesion [23, 24]. Intravenously injected ICG is removed from the circulation and remains in the lesion, allowing a high signal-to-background ratio, at a depth of few millimeters within the tissue itself [25]. FI-guided surgery with ICG (ICG-FI), both in vivo (intraoperative ICG-IF) and ex vivo (on the table ICG-FI) seems to be particularly suitable for detecting PC where superficial lesions are present. However, data about ICG-guided surgery in the treatment of PC from CRC is still scarce and the technique has not yet been standardized for this use.
The aim of the present study was to evaluate the role of ICG-FI in improving outcome in patients undergoing CS + HIPEC.
Materials and methods
Patient cohort
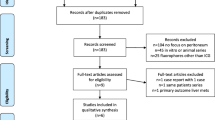
From October 1, to December 31, 2016, at the Division of Surgical Oncology of the University of Campania “Luigi Vanvitelli”, Naples, Italy, seven consecutive patients with PC from CRC were admitted. Inclusion criteria for CS + HIPEC were age 18–70 years, PCI ≤ 20 at preoperative diagnosis, tumor limited to the peritoneal cavity without other distant metastases, absence of severe comorbidities with performance status ≤1. Three patients were excluded from surgical treatment because of high PCI (29 and 31, respectively), or poor general conditions (one patient). Ultimately, four patients underwent surgical exploration. All patients had previously undergone a potentially curative resection for stage III colorectal adenocarcinoma. After resection of the primary tumor, all patients had received 5-fluorouracil plus oxaliplatin-based adjuvant chemotherapy and had been followed at 3-monthly intervals until tumor recurrence. This prospective study was approved by the Ethics Committee of the University of Campania “Luigi Vanvitelli,” and all patients gave written informed consent.
ICG-FI-guided surgery
All operations were performed through open median relaparotomy. After clinical exploration of the entire peritoneal cavity, with the assessment of the feasibility of CC-0 or CC-1 cytoreduction and localization of metastatic nodules, a dose of 0.25 mg/kg ICG (PULSION Medical Systems SE, FeldKirchen, Germany) was injected intravenously. IF-guided imaging was performed in vivo on the entire peritoneal cavity by using the Fluobeam® (Fluoptics Imaging Inc, Cambridge, MA, USA), an open system for in vivo infrared fluorescence imaging. At Fluobeam® examination, the peritoneum appeared as a large gray area striped with very thin bright lines corresponding to vascular structures. With black and white vision, a hyperfluorescent peritoneal nodule appeared as a well-defined area of intense bright light with clear margins (Fig. 1a). This area, with color vision allowed by Fluobeam®, appeared as a red zone with ultraviolet margins (Fig. 1b). Visible and/or palpable nodules showing no clear dissimilarity from the gray peritoneal serosa (with black and white vision) or colors shifting from green to ultraviolet were defined as hypofluorescent nodules.
After surgical resection, all peritoneal sites were checked again to evaluate residual fluorescence. Finally, all specimens were observed ex vivo with Fluobeam® to confirm their previous appearance and investigate the margins of resected tissue.
HIPEC was performed through a closed technique by using oxaliplatin (400 mg/m2) in 5 L of 5% glucose solution for 30 min at 42 °C.
Statistical analysis
Data are expressed as range, median value and interquartile range (IQR). Sensitivity (probability that the test identifies all peritoneal nodules), specificity (probability that the test does not identify all non-cancerous nodules), positive predictive value (probability that the identified nodule is metastatic), negative predictive value (probability that the unidentified nodules are non-cancerous tissue), and test accuracy (correct diagnosis from the test) with their 95% confidence intervals (CI) were calculated by using the receiver operating characteristic (ROC) curve analysis. For each diagnostic method (pre-, intraoperative, and ICG-FI) was calculated the area under the curve (AUC), and a comparison among the curves was performed. Differences between continuous variables were calculated by using the paired sample t test assuming as significant a p value <0.05. Statistical analyses were carried out using the Medcalc® software version 9.4.2.0 (Mariakerke, Belgium).
Results
The patient characteristics are shown in Table 1. In all patients, a CC-0 cytoreduction was performed followed by HIPEC. No patient experienced severe postoperative complications and all were discharged on postoperative days 9–11. The peritoneal exploration was performed at a median time of 50 min after the ICG injection (range 30–60; IQR 35–60 min). The time for ICG-FI took a median of 20 min (range 10–30; IQR 15–25 min), and all images collected by Fluobeam® were converted into pictures and videos. The operation time ranged from 240 to 360 min (median 280 min; IQR 250–330 min).
Overall, a total of 69 nodules were harvested (median diameter 2.7 cm; range 0.2–5.0 cm; IQR 1.2–3.8 cm). With conventional techniques, such as CT and PET scans, 30 nodules had been diagnosed preoperatively (median diameter 3.8 cm; range: 1.5–5.0 cm; IQR 3.5–4.4 cm). Intraoperative exploration added further 22 peritoneal nodules (median diameter 2.3 cm; range: 1.3–3.1 cm; IQR 1.8–2.8 cm). Out of these 52 nodules, 47 (90%) were hyperfluorescent at examination with Fluobeam®. ICG-FI identified 17 additional hyperfluorescent nodules with a median diameter of 0.5 mm (range 0.2–0.7 cm; IQR 0.3–0.6 cm) (Fig. 2).
All specimens were also examined with Fluobeam® ex vivo, namely on the table in the operating room. There was a complete correspondence between in vivo and ex vivo observations (Fig. 3a, b). Furthermore, a boundary of hypofluorescent tissue was identified around each lesion. Postoperative histopathology showed that two preoperatively diagnosed, and other two intraoperatively detected nodules were non-metastatic. Out of 64 hyperfluorescent nodules, one (false positive) resulted non-cancerous; out of five hypofluorescent nodules, two (false negatives) resulted to be metastatic tissue. In all cases, the hypofluorescent tissue around each lesion was negative for metastatic tissue.
Out of 65 metastatic peritoneal nodules, the ICG-FI allowed to identify 16 nodules undiagnosed from conventional procedures, adding a 25% diagnostic improvement. Overall, the sensitivity of current diagnostic procedures (CT and PET scans) was 43.1% preoperatively and 76.9% intraoperatively (visual examination and palpation). With ICG-FI sensitivity increased to 96.9%. ICG-FI showed the highest specificity, and positive and negative predictive values. The test accuracy, i.e., the global prognostic performance of the procedure, was 43.4, 75.3 and 95.6% for preoperative, intraoperative and ICG-FI, respectively (Table 2). The comparison of ROC curves showed that the diagnostic performance between pre- and intraoperative conventional methods was not different (p = 0.35); on the contrary, ICG-FI did significantly better than preoperative (p = 0.027), and intraoperative diagnostic tools (p = 0.042) (supplemental Fig. 1).
Before ICG-FI, the median PCI was 7 (range 2–12, IQR 4–10) but after ICG-FI, the PCI significantly increased to a median of 10 (range 3–15, IQR 5–13; p < 0.001). However, the worsening of the PCI did not prevent to perform a complete cytoreduction in all patients.
Cytological examination of the peritoneal washing liquid was positive for malignant cells in three out four cases before HIPEC and negative in all cases after HIPEC.
Discussion
CC-0 or at least CC-1 cytoreduction is the goal of the surgical therapy of PC from CRC. A technique that improves intraoperative detection of PC nodules would help to obtain complete cytoreduction and avoid resection of non-cancerous lesions.
In spite of the small number of patients and of PC nodules that are limitations of our study, our results with intraoperative ICG-FI appear promising. Using this imaging technique, it was possible to correctly map metastatic areas with a sensitivity of 97%, a test accuracy of 95.6%, and improvement of almost 25% in identifying the disease. The 16 malignant lesions identified intraoperatively with Fluobeam® had been missed at conventional abdominal exploration.
To the best of our knowledge, this study represents the third ever published experience on the use of ICG in peritoneal carcinomatosis from colorectal cancer. Last year, Liberale et al. and Barabino et al. both from Europe reported their results in 17 and 10 patients, respectively [14, 22]. Our results differ from those reported by Barabino [22]. In contrast with our results showing that the PCI score improved significantly from 7 (with conventional methods) to 10 (with PCI-FI), Barabino et al. reported a not significant difference between conventional and ICG-FI-guided surgery [22]. They also reported false positive and negative rates of 40 and 27%, respectively, whereas our rates were 25 and 3%, respectively. The authors’ explanation of these high rates includes preoperative chemotherapy, and limitations of the EPR effect of ICG. However, Barabino and colleagues administered ICG 24 h preoperatively, and it could have impaired their results. In our experience, 50 min after intravenous injection of ICG, the intraoperative view with Fluobeam® of fluorescent areas in the abdomen was optimal. Our decision to perform intraoperative injection of the fluorescent probe was influenced by our previous experience with ICG-FI-guided surgery of liver cancer in which the injection was performed 24 h before surgery, in order to consistently reduce physiological hepatic uptake and allow the drug to concentrate in the tumor [26, 27]. In these cases, there was no peritoneal fluorescence at the time of the operation. As in our observations, Liberale et al. did not detect fluorescence in the metastatic nodules in the first two patients who received ICG 24 h before surgery. In contrast, in the remaining patients who received intraoperative injection of ICG, all peritoneal nodules were hyperfluorescent [14].
Establishing the optimal dosage of ICG and timing of injection are important for standardization of the technique. Some authors [24] propose a dose of 0.5 mg/kg 12–24 h before surgery, others [14] an overall dose of 5 mg administered intraoperatively. In the case of PC, in which numerous, small, hypervascularized nodules have to be detected, an intraoperative ICG injection is suitable since ICG disappears from plasma at a rate of 18 to 25% per minute [28].
A new interesting tool is represented by the prophylactic HIPEC in CRCs at high risk of developing metachronous peritoneal carcinomatosis, such as tumors invading the serosa (pT4a), or with positive peritoneal washing liquid [29]. In these patients, current clinical and imaging techniques sill lack sufficient diagnostic sensitivity [30], and ICG-FI-guided surgery could identify undiagnosed small peritoneal metastatic nodules. In addition, this technique would be a great tool to enhance sensitivity for second-look laparoscopy in high-risk patients and it could be practice-changing.
This study has some limitations. The number of patients was too small to drawn definitive conclusions and conflicting results with previous studies require caution. However, ICG-FI-guided surgery seems a promising tool to improve the radicality of CS in PC originating from CRC. Further studies are needed to standardize the technique and determine its role in this patient population.
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:359–386
Chu DZ, Lung NP, Thompson C et al (1989) Peritoneal carcinomatosis in non-gynecologic malignancies: a prospective study of prognostic factors. Cancer 63:364–367
Sadeghi B, Arvieux C, Glehen O et al (2000) Peritoneal carcinomatosis in non-gynecologic malignancies: results of EVOCAPE 1 multicentric prospective study. Cancer 88:358–363
Jessup MJ, Goldberg RM, Asara EA et al (2017) Colon and rectum. In: American joint committee on cancer. AJCC Cancer Staging Manual, 8 edn. Springer, Berlin, pp 251–274
Elias D, Faron M, Juga BS et al (2015) Prognostic similarities and differences in optimally resected liver metastases and peritoneal metastases from colorectal cancers. Ann Surg 261:157–163
Glehen O, Kwiatkowski F, Sugarbaker PH et al (2004) Cytoreductive surgery combined with preoperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol 22:3284–3292
Da Silva RG, Sugarbaker PH (2006) Analysis of prognostic factors in seventy patients having complete cytoreduction plus perioperative intraperitoneal chemotherapy for carcinomatosis from colorectal cancer. J Am Coll Surg 203:878–886
Elias D, Raynard B, Farkhondeh F et al (2006) Long-term survival of peritoneal carcinomatosis of colorectal origin. Gastroenterol Clin Biol 30:1200–1204
Quere P, Facy O, Manfredi S et al (2015) Epidemiology, management, and survival of peritoneal carcinomatosis from colorectal cancer: a population-based study. Dis Colon Rectum 58:743–752
Blackham AU, Russell GB, Stewert JH 4th et al (2014) Metastatic colorectal cancer: survival comparison of hepatic resection versus cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol 21:2667–2674
Begossi G, Gonzales-Moreno S, Ortega Perez G et al (2002) Cytoreduction and intraperitoneal chemotherapy for the management of peritoneal carcinomatosis, sarcomatosis and mesothelioma. Eur J Surg Oncol 28:80–87
Dromain C, Leboulleux S, Auperin A et al (2008) Staging of peritoneal carcinomatosis: enhanced CT vs. PET/CT. Abdom Imaging 33:87–89
Sugarbaker PH (1998) Intraperitoneal chemotherapy and cytoreductive surgery for the prevention and treatment of peritoneal carcinomatosis and sarcomatosis. Semin Surg Oncol 14:254–261
Liberale G, Vankerckhove S, Caldon MG et al (2016) Fluorescence imaging after indocyanine green injection for detection of peritoneal metastases in patients undergoing cytoreductive surgery for peritoneal carcinomatosis from colorectal cancer: a pilot study. Ann Surg 264:1110–1115
Sugarbaker PH (1999) Successful management of microscopic residual disease in large bowel cancer. Cancer Chemother Pharmacol 43:15–25
Gomez Portilla A, Sugarbaker PH, Chang D (1999) Second look surgery after cytoreductive and intraperitoneal chemotherapy for peritoneal carcinomatosis from colorectal cancer: analysis of prognostic features. World J Surg 23:23–29
Berthet B, Sugarbaker TA, Chang D et al (1999) Quantitative methodologies for selection of patients with recurrent abdominopelvic sarcoma for treatment. Eur J Cancer 3:413–419
Kim S, Lim YT, Soltesz EG et al (2004) Near-infrared fluorescent type II quantum dots for sentinel lymph node mapping. Nat Biotechnol 22:93–97
Schaafsma BE, Mieog JSD, Hutteman M et al (2011) The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. J Surg Oncol 104:323–332
Polom K, Murawa D, Rho Y et al (2011) Current trends and emerging future of indocyanine green usage in surgery and oncology: a literature review. Cancer 117:4817–4822
Fox IJ, Wood EH (1960) Indocyanine green: physical and physiologic properties. Proc Staff Meet Mayo Clin 35:732–744
Barabino G, Klein JP, Porcheron J et al (2016) Intraoperative near-infrared fluorescence imaging using indocyanine green in colorectal carcinomatosis surgery: proof of concept. Eur J Oncol Surg 42:1931–1937
Maeda H, Wu J, Sawa T et al (2000) Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 65:271–284
Bekheit M, Vibert E (2015) Fluorescent-guided liver surgery: Paul Brousse experience and perspectives. In: Dip FD (ed) Fluorescence imaging for surgeons: concepts and applications, vol 11. Springer, Switzerland, pp 117–126
Frangioni J (2003) In vivo near-infrared fluorescence imaging. Curr Opin Chem Biol 7:626–634
Miyashiro I, Miyoshi N, Hiratsuka M et al (2008) Detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging: comparison with infrared imaging. Ann Surg Oncol 15:1640–1643
Takahashi H, Zaidi N, Berber E (2016) An initial report on the intraoperative use of indocyanine green fluorescence imaging in the surgical management of liver tumors. J Surg Oncol 114:625–629
Faybik P, Hetz H (2006) Plasma disappearance rate of indocyanine green in liver dysfunction. Transplant Proc 38:801–802
Honoré C, Goéré D, Souadka A et al (2013) Definition of patients presenting a high risk of developing peritoneal carcinomatosis after curative surgery for colorectal cancer: a systematic review. Ann Surg Oncol 20:183–192
Cortes-Guiral D, Elias D, Cascales-Campos PA et al (2017) Second-look surgery plus hyperthermic intraperitoneal chemotherapy for patients with colorectal cancer at high risk of peritoneal carcinomatosis: does it really save lives? World J Gastroenterol 23:377–381
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure 1.
Receiver operating characteristic curves of ICG-FI guided surgery, and pre- and intraoperative conventional technology (AUC= area under the curve) (TIFF 252 kb)
Rights and permissions
About this article
Cite this article
Lieto, E., Auricchio, A., Cardella, F. et al. Fluorescence-Guided Surgery in the Combined Treatment of Peritoneal Carcinomatosis from Colorectal Cancer: Preliminary Results and Considerations. World J Surg 42, 1154–1160 (2018). https://doi.org/10.1007/s00268-017-4237-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4237-7