Abstract
Background
Immune-nutritional status has been recently reported as a prognostic factor in hepatocellular carcinoma (HCC). The controlling nutritional status (CONUT) score has been established as a useful tool to evaluate immune-nutritional status. This study aimed to investigate the efficacy of the CONUT score as a prognostic factor in patients undergoing hepatectomy for HCC.
Methods
A total of 295 patients who underwent curative hepatectomy for HCC between January 2007 and December 2014 were retrospectively analyzed. Patients were divided into two groups according to the CONUT score. The impact of the CONUT score on clinicopathological, surgical, and long-term outcomes was evaluated. Subsequently, the impact of prognostic factors, including the CONUT score, associated with outcomes was assessed using multivariate analyses.
Results
Of 295 patients, 118 (40%) belonged to the high CONUT group (CONUT score ≥ 3). The high CONUT group had a significantly lower 5-year recurrence-free survival rate than the low CONUT group (27.9 vs. 41.4%, p = 0.011) and a significantly lower 5-year overall survival rate (61.9 vs. 74.9%, p = 0.006). In multivariate analyses of prognostic factors, the CONUT score was an independent predictor of recurrence-free survival (hazard ratio = 1.64, p = 0.006) and overall survival (hazard ratio = 2.50, p = 0.001).
Conclusions
The CONUT score is a valuable preoperative predictor of survival in patients undergoing hepatectomy for HCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the third-leading cause of cancer-related deaths worldwide [1]. Although preoperative diagnosis, surgical technique, and radiofrequency ablation procedures for HCC have improved, the clinical outcomes of HCC remain poor, with a 5-year recurrence rate of 70% even in patients undergoing curative treatment [2]. Several studies have evaluated potential prognostic factors for HCC. In contrast to other solid malignancies, the prognosis and treatment options of HCC depend on tumor stage and hepatic functional reserve [3]. The two most commonly used scoring systems are the Cancer of the Liver Italian Program (CLIP) score [4] and Barcelona Clinic Liver Cancer (BCLC) staging classification [5]. However, these scoring systems focus on tumor status, basic liver function, and physical condition. Hypothetically, patients’ immune-nutritional status would be an essential factor for survival in HCC.
Recently, the presence of a systemic inflammatory response and immune-nutritional status, as indicated by the prognostic nutritional index (PNI) [6], have been reported to correlate with poor survival in patients with HCC [7–9]. The PNI, which is calculated from serum albumin level and total lymphocyte count, has conventionally been used to evaluate immune-nutritional status and surgical risk in gastrointestinal surgery [6].
The controlling nutritional status (CONUT) score is another automatic tool to assess nutritional status, taking into account laboratory information, including serum albumin, total cholesterol level, and total lymphocyte count [10]. The prognostic significance of CONUT has been reported in patients undergoing curative surgery for colorectal cancer [11]; however, no previous reports have evaluated the relationship between CONUT and clinical outcomes after hepatectomy for HCC.
This retrospective study evaluated the prognostic significance of the preoperative CONUT score on clinical outcomes and verified whether CONUT could predict survival in patients undergoing hepatectomy for HCC.
Materials and methods
Patients
We retrospectively reviewed the medical records of 295 consecutive patients who underwent curative resection of HCC at Okayama University Hospital (Okayama, Japan) between January 2007 and December 2014. This study was approved by the Ethics Committee of the Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences and Okayama University Hospital and conducted in accordance with the Declaration of Helsinki.
Clinical data
From our database, the following preoperative factors were evaluated: sex, age, height, weight, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status, etiology of liver disease, laboratory values, tumor marker levels, liver function according to the Child–Pugh score and technetium-99 m-galactosyl human serum albumin (99mTc-GSA), and comorbidities.
The CONUT score was calculated using albumin level, total lymphocyte count, and total cholesterol level in each patient, as described in Table 1 [10]. In this study, patients were divided into 2 groups: the low CONUT group (score ≤ 2) and the high CONUT group (score ≥ 3) [11]. Concerning PNI, on the basis of the original report, we used the following formula: 10 × albumin levels (g/dL) + 0.005 × total lymphocyte count (/mm3). Patients were divided into 2 groups based on PNI: the low PNI group (score < 40) and high PNI group (score ≥ 40) [11].
Data regarding surgical procedure, operative time, and blood loss were recorded as operative factors. Details of the surgical techniques have been reported previously [12]. Tumor specimens and the degree of hepatic fibrosis were evaluated by pathologists in accordance with the rules of the Liver Cancer Study Group of Japan [13].
Short-term and long-term outcomes
Postoperative complications were assessed using the Clavien–Dindo classification [14], with major complications defined as Clavien grade ≥3. All patients underwent follow-up examination every 3 or 6 months at our institution or another affiliated hospital to examine their physical condition, liver function, and recurrence. The last data of this cohort were updated in February 2016.
The relationship between the CONUT score and other clinical parameters
To identify the clinical meaning of the CONUT score, patients were also divided into 4 conventional categories of undernutrition status (normal, light, moderate, and severe) (Table 1) [11]. Then, the relationship between the CONUT score and other clinical parameters was examined.
Statistical analysis
Data are presented as mean, median, and standard deviation for continuous variables. Categorical data are presented as proportions. Differences between groups were assessed using the Mann–Whitney U test for continuous variables and Fisher’s exact test or Chi-square test for categorical variables. Overall and recurrence-free survival rates were calculated using the Kaplan–Meier method, and differences between curves were analyzed using the log rank test. To investigate the impact of prognostic factors associated with overall and recurrence-free survival, the Cox proportional hazard model was used for univariate and multivariate analyses, and hazard ratios (HRs) and 95% confidence intervals were calculated. A p value < 0.05 was considered statistically significant. JMP version 10 software (SAS Institute, Cary, NC) was used for statistical analysis.
Results
Demographics
Table 2 shows the clinicopathological characteristics of the 295 patients. The median CONUT score was 2 (interquartile range, 1–3) (Fig. 1). The low CONUT group included 177 patients, and the high CONUT group included 118 patients. Sex ratio, age, BMI, ASA physical status, etiology of liver disease, tumor marker levels, comorbidities, operative factors, pathological factors, and incidence of major complications were not significantly different between the two groups. Patients with Child–Pugh score B were significantly more frequent in the high CONUT group (p = 0.01).
Median PNI was 47.3 (interquartile range, 42.7–51.7). Most patients (n = 263) were in the high PNI group, and 32 patients (10.8%) were in the low PNI group. Table 3 shows the relationship between CONUT score and PNI. Overall, 177 patients (60%) had normal CONUT scores (low CONUT group) and PNI (high PNI group). Eighty-six patients (29.2%) belonged to the normal PNI group and the abnormal CONUT group.
Recurrence after hepatectomy for HCC
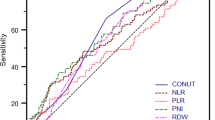
The recurrence-free survival curve in patients with high and low CONUT scores is shown in Fig. 2a. One hundred fifty patients (50.8%) had recurrence at intrahepatic sites (n = 120), extrahepatic sites (n = 13), and both intrahepatic and extrahepatic sites (n = 17). The 2- and 5-year recurrence-free survival rates were 45.8 and 27.9% in the high CONUT group and 57.6 and 41.4% in the low CONUT group, respectively (p = 0.011). Table 4 shows the results of univariate and multivariate analyses to identify prognostic factors for HCC recurrence after hepatectomy. Multivariate analysis revealed that high CONUT score, ASA physical status of 3 or 4, Child–Pugh score B, presence of multiple tumors, and microvascular invasion were significant independent factors for HCC recurrence.
Survival after hepatectomy for HCC
After a mean follow-up of 42.3 months, 74 patients (25.1%) died from the following causes: cancer progression (n = 48); liver failure (n = 15); infection (n = 3); and other reasons (n = 8). Patients with high CONUT scores had a significantly worse prognosis than those with low CONUT scores (p = 0.006) (Fig. 2b). The 2- and 5-year overall survival rates following hepatectomy were 77.7 and 61.9% in the high CONUT group and 89.3 and 74.9% in the low CONUT group, respectively. Table 5 shows the results of univariate and multivariate analyses to identify prognostic factors closely related to overall survival after hepatectomy. In univariate analysis, 9 variables were independent factors associated with poor prognosis; of these, 5 variables were significant poor prognostic factors in multivariate analysis: high CONUT score, ASA physical status of 3 or 4, Child–Pugh score B, presence of multiple tumors, and microvascular invasion.
The influence of the CONUT score on tumor recurrence
In the high CONUT group, HCC recurred at intrahepatic sites (n = 53), extrahepatic sites (n = 3), and both intrahepatic and extrahepatic sites (n = 9). The low CONUT group had HCC recurrence at intrahepatic sites (n = 67), extrahepatic sites (n = 10), and both intrahepatic and extrahepatic sites (n = 8). There was no difference in the HCC recurrence patterns between groups (p = 0.22).
CONUT score and other clinical parameters
The relationship between the CONUT score and other clinical parameters is shown in Table 6. Categories of undernutrition status were: normal (n = 118); light (n = 148); moderate (n = 29); and severe (n = 0). CONUT score was significantly associated with platelet count, prothrombin time, Child–Pugh score, the value of 99mTc-GSA, and the degree of hepatic fibrosis.
Discussion
This retrospective study demonstrates that the preoperative CONUT score was an independent prognostic factor after hepatectomy for HCC in our series. The prognostic significance of the CONUT score in patients with colorectal cancer has been reported [11]; however, this is the first report to identify the prognostic significance of the CONUT score in patients with HCC.
The CONUT score is a screening tool designed to easily and objectively assess patients’ nutritional status [10]. Various methods to evaluate immune-nutritional status have been developed, and recently PNI was reported to correlate with survival in patients with HCC [7–9]. The CONUT score and PNI have common factors (serum albumin and total lymphocyte count); the relationship between the CONUT score and PNI is shown in Table 3. We found that all patients with a low PNI belonged to the high CONUT group. CONUT score additionally identified patients expected to have poor survival who were not detected by PNI.
With regard to CONUT score parameters, serum albumin concentration is a reliable nutritional screening tool, influenced by not only nutritional status but also non-nutritional factors such as hepatic functional reserve, inflammation, and hydration status [15]. A lower albumin level is associated with increased levels of inflammatory cytokines, such as interleukin-6, which are associated with progression of liver fibrosis and HCC [7]. Most patients with HCC have chronic viral hepatitis as well as persistent chronic inflammation. The systemic and chronic inflammatory response to virus or tumor is also associated with decreased serum albumin concentration and poor prognosis in patients with HCC [9].
The total lymphocyte count is a surrogate marker of nutritional and immune status in patients with HCC [16–18]. Total lymphocytes are reportedly associated with the development of HCC [19]. Lymphocytes, such as CD4+ cells and natural killer cells, play a key role in antiviral and cellular immunity [20]. Lower lymphocyte count is associated with poor prognostic factors in patients with HCC because of inadequate immune response to cancer [18, 21].
Serum cholesterol level was reported to be a prognostic factor for outcomes of for HCC [22]. A decrease in cholesterol level implies not only a calorie deficiency but also that cells are being deprived of an essential nutrient required to maintain metabolic and hormonal equilibrium and membrane integrity [23]. Therefore, inadequate immunocompetent cells would be unable to exert their immunological function against cancer cells because of membrane structure changes [24]. This might explain why cholesterol level is associated with prognosis in patients with HCC.
In the present study, we found a strong correlation between the CONUT score and survival. Patients with HCC with a high CONUT score had significantly lower recurrence-free and overall survival rates (Fig. 2), similar to results among colorectal cancer patients [11]. Our multivariate analysis revealed that the CONUT score was an independent preoperative predictor related to recurrence-free and overall survival after hepatectomy (Tables 4, 5).
Among preoperative factors, ASA physical status and Child–Pugh score were also significant factors associated with survival. The ASA physical status is evaluated by anesthesiologists to assess surgical risk; it is also useful to assess patients’ general condition, but it can be subjective. The Child–Pugh score is reportedly associated with hepatic functional reserve and prognosis in HCC. Similar to previous reports, tumor-specific factors, such as multiple tumors and microvascular invasion, were strong independent factors associated with survival [25, 26], but tumor size and differentiation were not significantly associated with survival. Although PNI has been reported to correlate with survival in patients with HCC [7–9], PNI was not an independent predictor in this study. Therefore, the CONUT score might be a more accurate prognostic factor than the PNI.
Interestingly, a significant relationship was seen between the CONUT score and some clinical parameters (Table 6). These results might indicate that the CONUT score reflected hepatic functional reserve. Furthermore, the CONUT score had a significant relationship with hepatic fibrosis. Indeed, 19 patients (65.5%) with moderate undernutrition status had stage 3 or 4 fibrosis. The CONUT score could predict not only hepatic functional reserve but also the stage of fibrosis.
Despite our important findings, there are a few limitations to the current study. First, this was a retrospective, single-center study; therefore, there may be potential selection bias in the enrollment of patients for hepatectomy. Second, the number of patients is small. Third, although the CONUT score conventionally described four classes of undernutrition (Table 1), we used other cutoff values according to a previous report [11]. In the present study, the cutoff value for the CONUT score associated with survival using the receiver operating characteristic was also 3 (area under the curve = 0.59). Further studies are needed to determine more adequate cutoff values of the CONUT score to predict worse outcomes. Finally, we did not compare the efficiency of the CONUT score with that of other screening systems, such as nutrition risk index (NRI), malnutrition universal screening tool (MUST), and nutritional risk screening (NRS-2002) [27], because this study was conducted retrospectively and such screening systems were not assessed. However, a comparison of the four systems indicated that CONUT was clearly superior at predicting the statistical outcome [23, 28]. Future studies are required to assess the efficiency of screening systems to evaluate patients’ status.
Conclusion
Our study indicates that the CONUT score is a reliable and independent preoperative predictor of survival after hepatectomy for HCC. Assessment of the CONUT score is an easy and feasible method and could help clinicians develop comprehensive approaches for decision-making regarding surgical indication.
References
Bray F, Ren JS, Masuyer E et al (2013) Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer 132:1133–1145
Forner A, Llovet JM, Bruix J (2012) Hepatocellular carcinoma. Lancet 379:1245–1255
Huitzil-Melendez FD, Capanu M, O’Reilly EM et al (2010) Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol 28:2889–2895
(1998) A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology 28:751–755
Llovet JM, Brú C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–338
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005 Article in Japanese
Pinato DJ, North BV, Sharma R (2012) A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer 106:1439–1445
Chan AW, Chan SL, Wong GL et al (2015) Prognostic nutritional index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol 22:4138–4148
Okamura Y, Ashida R, Ito T et al (2015) Preoperative neutrophil to lymphocyte ratio and prognostic nutritional index predict overall survival after hepatectomy for hepatocellular carcinoma. World J Surg 39:1501–1509. doi:10.1007/s00268-015-2982-z
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG et al (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
Iseki Y, Shibutani M, Maeda K et al (2015) Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS ONE 10:e0132488
Sadamori H, Yagi T, Shinoura S et al (2013) Risk factors for organ/space surgical site infection after hepatectomy for hepatocellular carcinoma in 359 recent cases. J Hepatobiliary Pancreat Sci 20:186–196
Japan LCSGo (2010) General rules for the clinical and pathological study of primary liver cancer, 3rd English edn. Tokyo
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Tanriverdi O (2014) A discussion of serum albumin level in advanced-stage hepatocellular carcinoma: a medical oncologist’s perspective. Med Oncol 31:282
Xiao WK, Chen D, Li SQ et al (2014) Prognostic significance of neutrophil-lymphocyte ratio in hepatocellular carcinoma: a meta-analysis. BMC Cancer 14:117
Sun XD, Shi XJ, Chen YG et al (2016) Elevated preoperative neutrophil-lymphocyte ratio is associated with poor prognosis in hepatocellular carcinoma patients treated with liver transplantation: a meta-analysis. Gastroenterol Res Pract 2016:4743808
Hu B, Yang XR, Xu Y et al (2014) Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res 20:6212–6222
Jia Y, Zeng Z, Li Y et al (2015) Impaired function of CD4 + T follicular helper (Tfh) cells associated with hepatocellular carcinoma progression. PLoS ONE 10:e0117458
Nagai S, Abouljoud MS, Kazimi M et al (2014) Peritransplant lymphopenia is a novel prognostic factor in recurrence of hepatocellular carcinoma after liver transplantation. Transplantation 97:694–701
Wang M, Li C, Wen TF et al (2016) Postoperative low absolute lymphocyte counts may predict poor outcomes of hepatocellular carcinoma after liver resection. Chin Med J (Engl) 129:536–541
Lee YL, Li WC, Tsai TH et al (2016) Body mass index and cholesterol level predict surgical outcome in patients with hepatocellular carcinoma in Taiwan—a cohort study. Oncotarget 7:22948–22959
de Ulíbarri Pérez JI, Fernández G, Rodríguez Salvanés F et al (2014) Nutritional screening; control of clinical undernutrition with analytical parameters. Nutr Hosp 29:797–811
Kritchevsky SB, Kritchevsky D (1992) Serum cholesterol and cancer risk: an epidemiologic perspective. Annu Rev Nutr 12:391–416
Colecchia A, Schiumerini R, Cucchetti A et al (2014) Prognostic factors for hepatocellular carcinoma recurrence. World J Gastroenterol 20:5935–5950
Shah SA, Cleary SP, Wei AC et al (2007) Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 141:330–339
Kondrup J, Rasmussen HH, Hamberg O et al (2003) Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 22:321–336
Kyle UG, Kossovsky MP, Karsegard VL et al (2006) Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr 25:409–417
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Takagi, K., Yagi, T., Umeda, Y. et al. Preoperative Controlling Nutritional Status (CONUT) Score for Assessment of Prognosis Following Hepatectomy for Hepatocellular Carcinoma. World J Surg 41, 2353–2360 (2017). https://doi.org/10.1007/s00268-017-3985-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3985-8