Abstract
Background
Postoperative pancreatic fistula (POPF) causes significant morbidity and mortality after distal pancreatectomy. Patch coverage of the pancreatic stump is often used with the intention to prevent POPF. Despite numerous investigations, the effects of patch coverage remain unclear. The present meta-analysis aims to clarify the effects of patch coverage in distal pancreatectomy on the incidence of POPF.
Methods
A systematic search of MEDLINE/PubMed and the Cochrane Database according to the PRISMA Statement was performed. Subsequently a meta-analysis on rates and overall incidence of POPF and length of hospital stay was carried out. By applying the inverse variance weighting method, the combined effect size and 95 % confidence interval were calculated. Heterogeneity was assessed using I 2 statistics.
Results
Five randomized controlled trials and six observational clinical studies were included for final analysis. A cumulative incidence of 43 % of POPF grades A–C was identified. Patch coverage in distal pancreatectomy is significantly associated with a decreased rate of POPF grade C (p = 0.006). Patches of autologous vascularized tissue significantly reduce the overall incidence of POPF (p = 0.04) and clinically relevant POPF grade B and C (p = 0.002). Fibrin sealant patches do not influence rates of POPF after distal pancreatectomy. None of the outcomes evaluated showed adverse results for the patch group.
Conclusions
Patch coverage after distal pancreatectomy can reduce the rate of POPF. Patch coverage with autologous vascularized tissue but not fibrin sealant patches may be used to reduce clinically relevant POPF and postoperative morbidity in distal pancreatectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative pancreatic fistula (POPF) and intraabdominal fluid collection critically contribute to postoperative morbidity after distal pancreatectomy. Despite multiple efforts, the incidence of POPF still may exceed 50 % [1]. Up until now, various approaches for closure of the pancreatic remnant exist; however, none of them have been shown to reduce the rate of POPF [2]. Additionally, guidelines or general recommendations are lacking. Pasireotide, a somatostatin analogue that has a long half-life, has recently been shown to decrease the rate of pancreatic fistula in pancreaticoduodenectomy as well as in distal pancreatectomy [3]. Focusing on operative techniques, stapling of the pancreatic remnant does not reduce the incidence of POPF in comparison with regular hand sutures [4], but growing attention is now drawn to patch coverage of the pancreatic stump. In this respect, randomized controlled trials and observational clinical studies have been carried out evaluating different types of sealants for the pancreatic stump [5–7]. As such, fibrin sealant [1, 7–10], seromuscular [6, 11, 12], omental [13], gastric [13], and falciform/teres hepatis [5, 11, 14] patches have been investigated. In particular, patches of autologous vascularized tissue are thought to support local wound healing. However, results do not clearly support the use of a patch in distal pancreatectomy. We thus aimed to gather the existing evidence on patch coverage in distal pancreatectomy and performed a systematic review of the literature and a meta-analysis on selected outcomes. By analysis of randomized and nonrandomized studies, we seek to clarify the influence of patch coverage in distal pancreatectomy on the incidence of POPF. In particular, this study aims to compare the effect of autologous and fibrin sealant patches on the rates of POPF.
Methods
Search strategy
A systematic search of MEDLINE/PubMed and the Cochrane Database according to the PRISMA Statement [15] was performed by two independent researchers (MW and JGD) to identify suitable studies. Subsequently, reference lists were hand-searched for the relevant literature. The search terms used were “distal pancreatectomy” combined with “pancreatic fistula” and/or “patch” and/or “coverage” and/or “fibrin sealant”. “Distal pancreatectomy” does not exist as a “Medical Subject Heading” (MeSH), which is why controlled vocabulary terms could not be used.
Inclusion criteria
All articles published from 01/01/1990 to 12/31/2015 were included for abstract screening. Study selection was performed independently by two investigators (MW and JGD). Subsequently, randomized controlled trials (RCTs) and nonrandomized observational clinical studies (OCS) comparing distal pancreatectomy with patch coverage to distal pancreatectomy without patch coverage were included for detailed analysis. Only studies using the International Study Group on Pancreatic Fistula criteria for pancreatic fistula were included [16].
Exclusion criteria
Publications were excluded from further analysis if they were published in any language other than English, or focused on pediatric patients, transplant surgery, trauma surgery, or animal models. Furthermore, OCS other than case–control and cohort studies (case reports and case series), reviews of the literature, and publications not containing original data on patch coverage in distal pancreatectomy were also excluded.
Data xtraction and management
Data extraction was performed by two independent researchers (MW and JGD). After data extraction, a consensus meeting including all authors was held to select outcomes of interest for which meta-analyses should be performed. In case data were not reported completely for outcomes of interest, the corresponding authors were contacted and asked to provide the missing data. The following outcomes were defined as outcomes of interest: overall pancreatic fistula rate (grades A, B, and C), rate of POPF grade A, B, or C, combined rate of clinically relevant POPF grade B and C, mortality, and length of postoperative stay (LOS). First, the groups “patch” and “no patch” were compared, irrespective of the nature of the used patch. Subsequently, the groups “fibrin sealant patch” and “autologous patch” were compared.
Data synthesis
Effect sizes were calculated as a risk ratio (for dichotomous outcomes) or a mean difference. A fixed and random effect model was applied for all outcomes. For each study, the effect size with its 95 % confidence interval (CI) was calculated. This was followed by calculation of the combined effect size with its 95 % CI applying the inverse variance weighting method. For analysis of heterogeneity between the studies, the variance of the true effect size between the studies (Tau2) and a test for heterogeneity (I 2) were calculated. An I 2 greater than 50 % was considered as substantial heterogeneity. For meta-analyses, where substantial heterogeneity was detected, results of the random effects model are displayed. Otherwise, results of the fixed effects model are shown. For statistical analysis and figure generation, Review Manager Software (RevMan, version 5.3., Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used.
Results
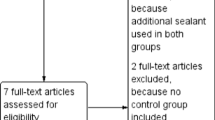
The systematic search of the literature retrieved 48 articles. Of these, 32 articles remained after removal of duplicates. Subsequently, 21 articles were excluded from further analysis. Figure 1 displays details on the number of excluded studies and the respective reasons for exclusion. Finally, a total of five RCTs [1, 5–7, 9] and six OCS [8, 10–14] remained. A total of 1359 patients were included, of which 721 were operated with patch coverage and 638 without patch coverage. Table 1 shows an overview on the characteristics of the studies included. Table 2 provides details on indications for surgery, pancreatic texture, blood loss, and operative time. Further details on age, gender distribution, patient body mass index (BMI), and pancreatic duct size are displayed in supplemental Table 1.
Study characteristics
All studies indicated whether the pancreatic stump was closed by stapler or by regular hand suture. Stapler closure was used in 312 patients in the patch group and in 267 cases in the no patch group. Statistically significant differences were not detected (p = 0.82). Drainages were routinely placed in all studies except the RCT by Sa Cunha et al. [9]. Intraabdominal drainages were not placed in five cases in the patch group and in seven cases in the no patch group (p = 0.42). Additionally, no statistically significant differences were detected with respect to operative time (p = 0.74), patient age (p = 0.20), and gender distribution (p = 0.25). Furthermore, no statistically significant differences between the patch and no patch group were detected with respect to indications for surgery (pancreatic cancer, p = 0.33; neuroendocrine tumors, p = 0.88; intraductal papillary mucinous neoplasms and cystic lesions, p = 0.37; others, p = 0.82). Meta-analyses on potential differences in blood loss, laparoscopic surgery, use of somatostatin analogues, patient BMI, pancreatic duct size, and pancreatic texture were not performed due to missing or incomplete data in a substantial amount of studies.
Incidence of POPF
The overall incidence of POPF grades A–C is 43 % when RCTs and OCS are subjected to joint analysis. Furthermore, the analysis of both RCTs and OCS revealed an overall incidence of 26 % for POPF grade A, 11 % for POPF grade B, and 3 % for POPF grade C. Detailed incidence figures are displayed in Table 3.
Overall POPF rate (grades A, B, and C)
For the overall POPF rate, data from five RCTs [1, 5–7, 9] and five OCS [8, 10, 12–14] were available. The meta-analysis of the RCTs (Supplemental Fig. 1) did not show a significant reduction in overall POPF rate for the patch group (risk ratio: 0.97; 95 % CI 0.86, 1.10; p = 0.66, I 2 = 29 %). Likewise, no significant difference between the patch and no patch group was evident in the meta-analysis of the five OCS (risk ratio: 0.79; 95 % CI 0.59, 1.05; p = 0.10, I 2 = 0 %) (Supplemental Fig. 2). The combined effect of both RCTs and OCS (Fig. 2) did not show an effect favoring either the patch or no patch group (risk ratio: 0.94; 95 % CI 0.84, 1.05; p = 0.30, I 2 = 11 %).
When studies investigating autologous patches only were analyzed (Fig. 3), an effect favoring the patch group was evident (risk ratio: 0.72; 95 % CI 0.53, 0.98; p = 0.04, I 2 = 0 %). The meta-analysis of studies investigating fibrin sealant patches (Supplemental Fig. 3) did not reveal a statistically significant difference between the patch and no patch group (risk ratio: 0.98; 95 % CI 0.87, 1.11; p = 0.76, I 2 = 9 %).
Rates of POPF grade A and B
For the meta-analysis on POPF grade A and B, data from four RCTs [1, 5–7] and six OCS [8, 10–14] were available. Neither the meta-analysis on POPF grade A (risk ratio: 1.05; 95 % CI 0.88, 1.26; p = 0.59, I 2 = 9 %) nor on POPF grade B (risk ratio: 0.78; 95 % CI 0.55, 1.09; p = 0.15, I 2 = 0 %) showed a statistically significant difference when RCTs and OCS were subjected to joint analysis (Fig. 2). Additionally, none of the subanalyses on RCTs only (Supplemental Fig. 1), OCS only (Supplemental Fig. 2), autologous patches, and fibrin sealant patches (Supplemental Fig. 3) displayed a statistically significant difference between the patch and no patch group.
Rate of POPF grade C
Also for the analysis on POPF grade C, data from four RCTs [1, 5–7] and six OCS [8, 10–14] were included. The meta-analysis of RCTs only (Supplemental Fig. 1) revealed a tendency favoring the use of a patch (risk ratio: 0.31; 95 % CI 0.08, 1.19; p = 0.09, I 2 = 0 %). The results of the meta-analysis of OCS only (Supplemental Fig. 2) displayed a statistically significant effect favoring the patch group (risk ratio: 0.40; 95 % CI 0.18, 0.91; p = 0.03, I 2 = 22 %). Furthermore, the combined meta-analysis of both OCS and RCTs (Fig. 2) showed a statistically significant effect favoring the patch group (risk ratio: 0.38; 95 % CI 0.19, 0.76; p = 0.006, I 2 = 0 %).
As shown in Fig. 3, a statistically significant effect favoring the patch group was evident in the meta-analysis on autologous patches (risk ratio: 0.39; 95 % CI 0.17, 0.87; p = 0.02, I 2 = 0 %). The meta-analysis on studies using fibrin sealant patches (Supplemental Fig. 3) did not reveal a statistically significant difference between the patch and no patch group (risk ratio: 0.35; 95 % CI 0.09, 1.34; p = 0.12, I 2 = 16 %).
Rate of clinically relevant POPF (grade B and C)
Data from five RCTs [1, 5–7, 9] and six OCS [8, 10–14] were included. The meta-analysis of RCTs only (Supplemental Fig. 4) did not show a statistically significant difference between the patch and no patch group (risk ratio: 0.98; 95 % CI 0.74, 1.30; p = 0.90, I 2 = 16 %). When OCS only (Supplemental Fig. 4) were analyzed, a significant effect favoring the patch group was evident (risk ratio: 0.54; 95 % CI 0.35, 0.82; p = 0.004, I 2 = 8 %). The combined analysis of both OCS and RCTs (Fig. 4) revealed a tendency favoring the patch group (risk ratio: 0.82; 95 % CI 0.64, 1.03; p = 0.09, I 2 = 36 %).
As shown in Fig. 4, a statistically significant effect favoring the patch group was evident in the meta-analysis on studies using autologous patches (risk ratio: 0.50; 95 % CI 0.32, 0.78; p = 0.002, I 2 = 0 %). The meta-analysis on fibrin sealant patches could not demonstrate a statistically significant difference between the patch and no patch group (risk ratio: 0.99; 95 % CI 0.75, 1.30; p = 0.92; I 2 = 7 %).
Mortality
All of the five RCTs [1, 5–7, 9] and six OCS [8, 10–14] provided data on mortality. Out of the 721 patients included in the patch group, one patient died in the study by Sa Cunha et al. [9]. In the no patch group, five out of 637 patients that were included died. Overall, no significant differences were detected between the patch and no patch group (risk ratio: 0.34; 95 % CI 0.08, 1.47; p = 0.15; I 2 = 0 %).
Length of postoperative stay
Data from five RCTs [1, 5–7, 9] were available for the meta-analysis on LOS. Two of the four studies that were included showed a statistically significant difference favoring the patch group [5, 7]. Upon analysis for heterogeneity, substantial heterogeneity was revealed, which is why a random effects model was applied. The combined effect showed a trend toward a reduction in LOS in the patch group (mean difference: −3.36; 95 % CI −7.40, 0.68; p = 0.10; I 2 = 92 %).
Discussion
Despite constant improvements in operative techniques, POPF still remains common after distal pancreatectomy and causes relevant morbidity and mortality, and increased health-care costs [11]. Recently, intensive efforts have been made to overcome this issue; however, none of the operative techniques that were evaluated have been shown to reduce postoperative complication rates. In this respect, the DISPACT trial [4], which compared regular hand suture to stapler closure in distal pancreatectomy, failed to show a reduction in POPF for stapled closure of the pancreatic remnant. The value of patch coverage of the pancreatic stump in distal pancreatectomy still remained to be clarified. Therefore, the present meta-analysis was performed to evaluate outcomes after distal pancreatectomy with and without patch coverage. Our data on the overall incidence of POPF illustrate the tremendous need for improvement of the operative technique. In this respect, the overall incidence of POPF grades A–C was 43 % in the analysis of both RCTs and OCS, and even as high as 52 % when RCTs only were analyzed.
Based on the results of the meta-analysis of both RCTs and OCS on overall POPF rate, patch coverage of the pancreatic stump may exert beneficial effects. Joint analysis of both studies investigating the effect of fibrin sealant and autologous patches revealed that patch coverage of the pancreatic stump may reduce POPF C after distal pancreatectomy. The fact that significant differences were limited to the rates of POPF C might be explained by the point that five [1, 7–10] out of the eleven included studies had been conducted with fibrin sealant patches and accounted for more than half of the 1359 patients that were included in this meta-analysis. Subsequently, subanalyses accounting for different types of patches were conducted showing that fibrin sealant patches do not influence the rate of any grade of POPF while autologous patches reduce the overall incidence of POPF, POPF C, and clinically relevant POPF. One may hypothesize that vascularized tissue is required to effectively support wound healing after distal pancreatectomy. Thus, as collagen sponges coated with fibrinogen and thrombin, fibrin sealant patches are unlikely to reduce rates of POPF. This comparison between fibrin sealant and autologous patches is limited by the fact that out of the six studies on autologous patches, four were OCS, whereas three out of the five studies on fibrin sealant patches were RCTs. Additionally, a heterogeneous group of patches was combined in the analysis on autologous patches.
Mortality was not reduced by usage of a patch. Nevertheless, our analysis shows that the overall mortality is low in distal pancreatectomy. For LOS, a trend toward reduced hospital stay was seen. However, each of the included RCTs in this analysis was conducted in a different country which is why this analysis is likely to be biased by internationally differing discharge criteria.
The present meta-analysis has several limitations. First, the majority of studies on autologous patches were OCS. Second, the overall incidence of POPF was high, which might have overpowered the meta-analyses on POPF. Vice versa, the mortality was low, and therefore, a potential difference might not have been detected.
However, despite its limitations this analysis indicates that fibrin sealant patches are unlikely to be beneficial in preventing POPF after distal pancreatectomy. Moreover, autologous patches represent a promising intervention worth further randomized controlled trials on patch coverage in distal pancreatectomy. However, high rates of POPF after distal pancreatectomy require intensified efforts on improving operative technique, and autologous patches probably represent the most promising option for future randomized controlled trials. Whether somatostatin analogues with a long half-life may be beneficial in this situation to further decrease clinically relevant pancreatic fistula remains unclear [3].
Conclusion
Patch coverage of the pancreatic remnant after distal pancreatectomy by autologous vascularized tissue can reduce the overall incidence of POPF and clinically relevant POPF. Fibrin sealant patches do not reduce the incidence of POPF after distal pancreatectomy and are not advisable for patch coverage of the pancreatic stump. Whether patch coverage in combination with application of long-acting somatostatin analogues shows additional effects deserves further investigation.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- IPMN:
-
Intraductal papillary mucinous neoplasm
- LOS:
-
Length of postoperative hospital stay
- NET:
-
Neuroendocrine tumor
- OCS:
-
Observational clinical studies
- PCa:
-
Pancreatic cancer
- POPF:
-
Postoperative pancreatic fistula
- RCT:
-
Randomized controlled trial
References
Park JS, Lee DH, Jang JY et al (2016) Use of TachoSil((R)) patches to prevent pancreatic leaks after distal pancreatectomy: a prospective, multicenter, randomized controlled study. J Hepatobiliary Pancreat Sci 23:110–117
Hartwig W, Werner J, Jager D et al (2013) Improvement of surgical results for pancreatic cancer. Lancet Oncol 14:e476–e485
Allen PJ, Gonen M, Brennan MF et al (2014) Pasireotide for postoperative pancreatic fistula. N Engl J Med 370:2014–2022
Diener MK, Seiler CM, Rossion I et al (2011) Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial. Lancet 377:1514–1522
Carter TI, Fong ZV, Hyslop T et al (2013) A dual-institution randomized controlled trial of remnant closure after distal pancreatectomy: does the addition of a falciform patch and fibrin glue improve outcomes? J Gastrointest Surg Off J Soc Surg Aliment Tract 17:102–109
Olah A, Issekutz A, Belagyi T et al (2009) Randomized clinical trial of techniques for closure of the pancreatic remnant following distal pancreatectomy. Br J Surg 96:602–607
Montorsi M, Zerbi A, Bassi C et al (2012) Efficacy of an absorbable fibrin sealant patch (TachoSil) after distal pancreatectomy: a multicenter, randomized, controlled trial. Ann Surg 256:853–859 discussion 859–860
Pavlik Marangos I, Rosok BI, Kazaryan AM et al (2011) Effect of TachoSil patch in prevention of postoperative pancreatic fistula. J Gastrointest Surg Off J Soc Surg Aliment Tract 15:1625–1629
Sa Cunha A, Carrere N, Meunier B et al (2015) Stump closure reinforcement with absorbable fibrin collagen sealant sponge (TachoSil) does not prevent pancreatic fistula after distal pancreatectomy: the FIABLE multicenter controlled randomized study. Am J Surg 210:739–748
Silvestri S, Franchello A, Gonella F et al (2015) Role of TachoSil(R) in distal pancreatectomy: a single center experience. Minerva Chir 70:175–180
Hassenpflug M, Hartwig W, Strobel O et al (2012) Decrease in clinically relevant pancreatic fistula by coverage of the pancreatic remnant after distal pancreatectomy. Surgery 152:S164–s171
Fujii T, Yamada S, Murotani K et al (2016) Modified blumgart suturing technique for remnant closure after distal pancreatectomy: a propensity score-matched analysis. J Gastrointest Surg: Off J Soc Surg Aliment Tract 20:374–384
Akca A, Goretzki PE, Wirowski D et al (2013) Is the covering of the resection margin after distal pancreatectomy advantageous? Eur J Med Res 18:33
Wu CT, Xu WY, Liu L et al (2013) Ligamentum teres hepatis patch enhances the healing of pancreatic fistula after distal pancreatectomy. Hepatobiliary Pancreat Dis Int 12:651–655
Preferred Reporting Items for Systematic Reviews and Meta-Analyses, 2015
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Maximilian Weniger and Jan Goesta D’Haese have contributed equally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Weniger, M., D’Haese, J.G., Crispin, A. et al. Autologous but not Fibrin Sealant Patches for Stump Coverage Reduce Clinically Relevant Pancreatic Fistula in Distal Pancreatectomy: A Systematic Review and Meta-analysis. World J Surg 40, 2771–2781 (2016). https://doi.org/10.1007/s00268-016-3612-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3612-0