Abstract
Background
Parathyroid glands (PGs) can be particularly hard to distinguish from surrounding tissue and thus can be damaged or removed during thyroidectomy. Postoperative hypoparathyroidism is the most common complication after thyroidectomy. Very recently, it has been found that the parathyroid tissue shows near-infrared (NIR) auto-fluorescence which could be used for intraoperative detection, without any use of contrast agents. The work described here presents a histological validation ex vivo of the NIR imaging procedure and evaluates intraoperative PG detection by NIR auto-fluorescence using for the first time to our knowledge a commercially available clinical NIR imaging device.
Methods
Ex vivo study on resected operative specimens combined with a prospective in vivo study of consecutive patients who underwent total or partial thyroid, or parathyroid surgery at a comprehensive cancer center. During surgery, any tissue suspected to be a potential PG by the surgeon was imaged with the Fluobeam 800 ® system. NIR imaging was compared to conventional histology (ex vivo) and/or visual identification by the surgeon (in vivo).
Results
We have validated NIR auto-fluorescence with an ex vivo study including 28 specimens. Sensitivity and specificity were 94.1 and 80 %, respectively. Intraoperative NIR imaging was performed in 35 patients and 81 parathyroids were identified. In 80/81 cases, the fluorescence signal was subjectively obvious on real-time visualization. We determined that PG fluorescence is 2.93 ± 1.59 times greater than thyroid fluorescence in vivo.
Conclusions
Real-time NIR imaging based on parathyroid auto-fluorescence is fast, safe, and non-invasive and shows very encouraging results, for intraoperative parathyroid identification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is the most common endocrine malignancy, and in recent decades, its incidence has shown a steady increase [1]. Thyroid cancer generally carries a very good prognosis [2]. In most cases, treatment is based on surgery [1, 3, 4]. Because of their small size and variable anatomic position adjacent to the thyroid gland, parathyroid glands (PGs) can be particularly hard to distinguish from surrounding tissue and thus can be damaged or removed during thyroidectomy. Temporary postoperative hypoparathyroidism is the most common complication after thyroidectomy, with an incidence ranging from 20 to 35 % [5]. Parathyroid preservation is critical in preventing hypoparathyroidism after thyroidectomy [6]. Today, there is no reliable intraoperative method to identify PG: the current solution is based on visual inspection from surgeon, which is a method by default and the results depend greatly on the operator’s experience [7].
The past several years have witnessed a growing interest for new optical imaging methods, especially in the near-infrared (NIR), in order to guide the surgeon and improve the outcomes of cancer surgery [8, 9]. NIR fluorescence takes advantage of the fact that NIR light (700–900 nm) penetrates blood and tissue to a depth of several millimeters, whereas visible light is limited to several micrometers. Moreover, auto-fluorescence of tissue in the NIR spectral range is very rare and most of the clinical uses of NIR fluorescence are based on the administration of contrast agents [8, 9]. But very recently it has been found that the parathyroid tissue shows NIR auto-fluorescence, independently of their pathological status [10, 11]. Interestingly, this optical property differentiates PG from surrounding tissue and could be used for intraoperative detection, without any labeling or any challenges associated with the use of contrast agents. The first studies of in vivo auto-fluorescence of PG have been reported by McWade et al. [12] at Vanderbilt University, using an experimental NIR camera (n = 6, human and dogs). Since their publication, several NIR cameras have been made commercially available, but the usefulness of commercialized NIR imaging systems has not been investigated to the extent of our knowledge. The feasibility of this technique in clinical practice remains unclear.
Here we report a histological validation of the auto-fluorescence using NIR imaging on healthy human parathyroid tissue ex vivo and an evaluation of intraoperative in vivo PG detection by NIR auto-fluorescence using a commercially available clinical NIR imaging device.
Methods
NIR imaging device and image acquisition
The system used in this study, Fluobeam® 800 Clinical System (Fluoptics, Grenoble, France), is a European Community-certified Class I medical device. It excites tissues with a wavelength of 750 nm (5 mW/cm2 at 20 cm) and collects the optical signal for wavelengths over 800 nm providing a global picture of the light signals emitted above 800 nm in real time. Auto-fluorescence requires operating lights to be turned off. The probe has an integrated NIR-less white light [LEDs (RG-1, 5000 lx at 20 cm)] to illuminate the surgical site. Real-time, two-dimensional video images are obtained using the Fluosoft (Fluoptics, Grenoble, France), which can save the video data and still images (in TIFF format). For our study, exposure time was set as 333 ms and the optical probe (diameter: 75 mm, length: 24 cm) was placed in a sterile sleeve intraoperatively. The imaging system illuminated the operating field, without touching the patient, with a working distance of about 20 cm.
Ex vivo NIR imaging
The visualization of the NIR fluorescence signal in parathyroid tissue was assessed ex vivo on resected specimens (see Table 1). The evaluation of the presence of PG on the specimen, due to iatrogenic resection, was performed blindly by a scientist using NIR imaging (i.e., without knowledge of the anatomy or histopathology) under the supervision of a pathologist. Samples were chosen based on the NIR fluorescence signal. The imaging procedure was performed between 5 min and 1 h after resection or after formalin fixation. The resected auto-fluorescent samples and entire specimens were examined by a pathologist and analyzed by conventional histology (HES staining).
In vivo study: patient population
Prospective study of consecutive patients (>18 years old) who underwent total or partial thyroid, or parathyroid surgery at Gustave Roussy were included between December 2014 and March 2015. All optical procedures were performed in a way that did not interfere with the quality of the patient care.
Intraoperative in vivo NIR imaging
During surgery, any tissue suspected to be a potential PG by the surgeon was non-invasively imaged with the Fluobeam 800®. In cases where no potential PG was found by visual examination, anatomical sites where PG could theoretically be located were also checked by NIR imaging. All the signals were compared to visual examination. The operating and ambient lights in the operating room were turned off during the NIR imaging procedure in order to minimize infrared interference in the room, the surgical site being illuminated by the Fluobeam®’s white light. No preoperative preparation was needed for intraoperative imaging. The imaging procedure did not interfere with the continuum of the surgical procedure. Absorbable sutures used during the procedure were coated Vicryl Polyglactin® 910 (Ethicon, Johnson&Johnson, New Brunswick, USA). Because of the limitations of histological analysis on healthy (and thus non-resected) parathyroid tissue, NIR imaging could only be compared to visual identification of the PG by the surgeon. The real-time infrared video and NIR auto-fluorescence images were compared directly with the intraoperative view of the surgical field. Although NIR imaging was considered as helpful to identify PG (see results section), the visual identification remained the gold standard (associated with histologic evidence where described) to guide surgery, as this is a feasibility study.
NIR signal quantification
Image acquisition was performed under the supervision of a surgeon in vivo or a pathologist for ex vivo specimens. Images were annotated directly during acquisition and quantification was measured post acquisition. Auto-fluorescence was quantified for tissue identified with a high confidence level (classified definitively PG) by the operator and/or by histological validation. The mean intensity of the signal was measured using ImageJ. In order to avoid environmental variations, each measured parathyroid signal was divided by the corresponding thyroid signal. We collected our measurements with a double condition: the parathyroid and the thyroid glands were in the same field of view and in the same plane; otherwise, they were excluded from the study. To determine the effect of formalin treatment, the ex vivo imaged tissues were treated for 24 h in formalin and then re-imaged. The ratios of the normalized signals, before and after formalin fixation, were calculated.
Results
Ex vivo near-infrared imaging for parathyroid gland identification
In order to validate the NIR auto-fluorescence signal coming from healthy human parathyroid gland (PG), we performed an ex vivo assessment of NIR imaging on resected specimens coming from different kinds of surgeries (listed in Table 1) where parathyroid tissue could be potentially found. The resected specimens were analyzed with the NIR camera under the supervision of pathologists to find any parathyroid tissue resected. NIR fluorescence-positive tissues were sampled and analyzed by conventional histology. With dimmed room lights, we were able to clearly see NIR auto-fluorescence coming from tissues that were confirmed later as PG (Fig. 1a, b). Our study included specimens coming from 28 patients. Based on the NIR images, we were able to identify 16 parathyroids (out of 17 parathyroids found histopathologically). It is worth noting that parathyroid tissue coming from thyroidectomy did not correspond to a complete PG but to small fragments remaining on the resected specimens (Fig. 1b). The parathyroid tissue that we were not able to observe with NIR imaging corresponded to an intrathyroid PG. Fluorescence signals were quantified on NIR images for 10 healthy PGs. These measures were normalized with the corresponding thyroid signal. The normalized PG fluorescence signal intensity varied from 1.7 to 5.4 times greater than that of thyroid fluorescence (average: 2.91 ± 0.89, Table 1).
Ex Vivo validation of NIR signal; tissues in geometric figures were sample and analyzed by conventional histology. NIR imaging of resected specimen of a laryngectomy with thyroidectomy (a); PGs are in the circles. NIR imaging of resected thyroidectomy (b) fragment of PG is in the circle. NIR imaging of fresh (c) or formalin-fixed (d) parathyroid tissue (circle) and thyroid tissue (broken line square). NIR imaging of a resected specimen from parathyroidectomy (parathyroid adenoma is in the circle) (e). NIR imaging of a resected specimen coming from a thyroidectomy (f); nodule is indicated by the dotted square. NIR imaging of the resected lymph nodes from neck dissection (g); signal from brown adipose tissue is indicated by the broken line circle
We also observed that PG auto-fluorescence remained stable over time (at least 1 h after resection for small PG fragments). Moreover, PG auto-fluorescence remains stable after tissue formalin fixation (Fig. 1c, d). We measured the normalized PG fluorescence signal intensity before and after formalin fixation and calculated the ratio between these two measures, which is 1.08 ± 0.14, showing that formalin fixation does not affect PG auto-fluorescence (Table 1). In a similar way, we also verified parathyroid adenoma (n = 4) auto-fluorescence (Fig. 1e), suggesting that NIR auto-fluorescence occurs in PGs, independently of their pathological status.
The NIR imaging procedure revealed other signals also. These positive tissues were also sampled and analyzed by conventional histology. These were identified as thyroid and brown adipose tissue (Fig. 1f, g). We have shown that thyroid fluorescence is less intense than PG fluorescence (Table 1). However, we noticed three cases where a bright spot was observed in thyroid tissue. These were identified as colloid nodule by histology and reported as false positive. The normalized nodule fluorescence signal intensity was 2.88 ± 1.14 times greater than that of the normal thyroid tissue. This value is similar to PG fluorescence, but visually the aspect of the nodule fluorescence is a more diffuse signal (Fig. 1f). Brown adipose tissue is quite rare in adults. Nevertheless, during the imaging procedure we observed bright spots (Fig. 1g) corresponding to brown adipose tissue (confirmed by conventional histology). Surprisingly, these bright spots were also observed when only using white light of the camera for illumination (with the NIR laser switched off). This shows that the signal is not NIR specific and thus does not correspond to PG auto-fluorescence. Therefore, brown adipose tissue can be easily discriminated by checking the signal specificity and this avoids any confusion with PG. Muscle, white adipose tissue, lymph nodes, thymus, and trachea do not show NIR auto-fluorescence. We were able to identify PG ex vivo using NIR imaging with a sensitivity of 94.1 % and a specificity of 80 % (Table 1).
In vivo near-infrared imaging for parathyroid gland identification
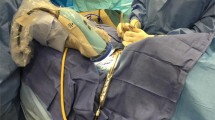
Intraoperative NIR imaging was performed on 35 patients (Table 2). As we could not ethically perform frozen section analysis on normal parathyroid during thyroid surgery (because a biopsy of such small organs may cause definitive harm and put the patient at risk of permanent hypoparathyroidism), we thus employed the only method currently a standard in thyroid surgery: visual identification. A total of 81 PGs were identified by the surgeons with a high level of confidence and/or histologic validation (Table 2). In all but one case (in which the identification of the parathyroid was verified by frozen section analysis), the fluorescence signal of the parathyroid glands was clearly obvious subjectively upon visualization of the real-time video (Fig. 2). Thus, in 80/81 cases, the intraoperative NIR imaging identification of PG was validated, for a sensitivity of 98.8 %.
Intraoperative NIR imaging for PG identification. Intraoperative NIR imaging and the corresponding bright light view of the PG of the same patient. URPG upper right parathyroid gland, ULPG upper left parathyroid gland, LRPG lower right parathyroid gland, LLPG lower left parathyroid gland, arrowhead: parathyroid gland, arrow: suture
To support our subjective interpretation of the obvious fluorescent signal observed in real time, we quantified the NIR fluorescence. Fluorescence signals were measured on NIR images for 53 healthy PGs. These measures were normalized with the corresponding thyroid signal. The normalized PG fluorescence signal intensity varied from 0.48 to 7.71 times (average: 2.93 ± 1.41; Table 2; Fig. 3) greater than that of thyroid fluorescence. PG NIR auto-fluorescence was consistently greater than thyroid fluorescence in 98.1 % (52 out of 53). The only PG fluorescence with lower value than its corresponding thyroid fluorescence was the PG considered as non-sufficiently fluorescent in our real-time intraoperative observation. These results are consistent with our intraoperative interpretation and our ex vivo study.
As mentioned above, ex vivo NIR imaging procedure revealed other signals. This was confirmed in our intraoperative study. Indeed, we observed auto-fluorescence coming from thyroid colloid nodules and unspecific signal from brown adipose tissue. We also observed that the brown adipose signal declined rapidly after resection of the adipose tissue, whereas the PGs that were removed for surgical reasons (devascularization) were still auto-fluorescent after 30 min in ice-cold saline serum (where they were held before re-implantation). All these results were confirmed on the final histopathologic analysis. It is also worth noting that the sutures used during this study (see methods) had NIR auto-fluorescent properties (Fig. 2, arrows). Muscle, white adipose tissue, lymph nodes, and trachea did not show NIR signal.
During surgery, the operator needs to clearly identify PGs in order to preserve them from iatrogenic lesions. In our study, we encountered three cases (Table 3): (1) the surgeon was sure that he had found a PG definitively; (2) the surgeon thought that it was possibly a PG; and (3) the surgeon did not find PG. Therefore, any tissues suspected of being a parathyroid were imaged using NIR camera and when the surgeon did not identify PG, potential locations were investigated with NIR imaging. As the surgeons who participated in this study are experimented in thyroid and parathyroid surgery, the surgeon was confident most of the time. In this case, the imaging procedure strengthened the surgeon’s opinion. Nevertheless, there were two cases where the tissue did not “light up.” The first case was the poorly auto-fluorescent parathyroid mentioned above. This PG was confirmed by frozen section analysis. It was the only reported false negative. On the contrary, in the second case, frozen section analysis indicated that the tissue was actually adipose. Thus, in this case NIR imaging was right against the surgeon’s first opinion. Moreover, in case the surgeon had any doubts, the NIR imaging procedure was a true guide for surgery. We noticed 14 cases of potential PG, where the operator’s first opinion was unsure. In those cases, the NIR imaging procedure results could clear up ambiguities concerning the presence or not of a PG. The NIR results were supported by further tissue examination (sinking test, visual examination, etc.). Finally, we also observed 5 cases where the surgeon did not find the PG before the NIR imaging procedure was performed. Those 5 PGs were found by investigating the bright spot of NIR auto-fluorescence during the imaging procedure. After examination, in all the cases, the surgeon was truly confident of the identity of the PG as indicated by the NIR imaging procedure.
Discussion
Parathyroid insufficiency is still the most common complication after total thyroidectomy [13]. Inadvertent PG resection may occur because of a lack of intraoperative PG identification. Several previous studies on image-guided surgery to address the issue of PG preservation during thyroidectomy required the administration of contrast agents, parathyroid specific or not [14–19]. These methods have limited clinical impact or currently have insufficient data for clinical use. The procedure presented here is based on the intrinsic optical properties of PG [12], thereby avoiding challenges associated with the use of contrast agents. We have validated PG auto-fluorescence ex vivo, but also in vivo and intraoperatively. Moreover, this is the first study to our knowledge using a commercial clinical device and our results suggest that this procedure could be adopted easily in thyroid surgery.
Very recently, McWade et al. [20] described a very interesting clinical evaluation of auto-fluorescence for PG detection based on spectroscopy instead of an NIR imaging system. A benefit of this method is to be able to quantify the fluorescence during surgery which is not possible using the Fluobeam© device, as it does not have a quantification module. Thus, we quantified PG fluorescence with pixel intensity on NIR images. Our measures showed a quite wide variety in PG auto-fluorescence intensity. Nevertheless, interestingly, the results of our ex vivo and in vivo studies showed that in both cases the PG intensities are in the same range and about 2.9 times greater than those of thyroid fluorescence. An advantage of NIR imaging is that this technology is contactless and provides real-time information with a large field of view, while spectroscopy needs to be in contact with the tissue to make measurement, point by point. NIR imaging provides a global view of the tissue illuminated in the operative field. This way, the procedure can highlight PGs even before the surgeon’s eyes, as it happened 5 times (out of a total of 35 patients and 81 PGs) during our study.
Due to the limitation of the depth of penetration of light in biological tissue, auto-fluorescence NIR imaging can identify PG to a limited extent. This technology cannot find parathyroid located deeper than a few millimeters in neck tissue. This is illustrated by the PG with an intrathyroid localization that we missed with NIR system during our ex vivo study. Therefore, the imaging procedure can only assess tissue exposed by the surgeon to the NIR light. However, beyond this limitation, the NIR imaging procedure seems to have a very good sensitivity both ex vivo and in vivo. This sensitivity is important because a tool that could mistake a PG for another tissue type could obviously not be useful for parathyroid preservation. Although we have noticed some variations in signal with NIR imaging, parathyroid auto-fluorescence is a clear interpretable signal.
The identity of the endogenous NIR fluorophore is currently unknown but potential candidates have been reported [10–12, 20]. McWade et al. indicate that these fluorescent compounds could also be found in thyroid tissue but in lower concentration than in PG. Our results support this possibility, especially our observation about colloid fluorescence. Endogenous fluorophores might also be used for detection of cancer cells. However, we did not observe any obvious auto-fluorescence in tissues surrounding thyroid cancer, in metastatic lymph nodes or surrounding the PG (normal or abnormal). Interestingly, NIR auto-fluorescence seems sustainable and can be observed on small parathyroid fragments, 1 h after en bloc resection, and after formalin fixation. This shows that NIR signal is not dependent on the parathyroid gland activity, vascularization, and/or viability. Further studies are needed to determine the source of the parathyroid auto-fluorescence.
The complication rate in thyroid surgery depends to a large extent on the operator’s experience [21]. Thus, a tool for intraoperative parathyroid detection would have more impact for less experienced surgeons. However, even highly experienced surgeons cannot completely avoid incidental PG resection. Interestingly, our study has shown that the NIR imaging procedure can clear up doubts that even experienced surgeons can have in anatomical identifications, leading to an increased precision in thyroid surgery. NIR fluorescence imaging is an expanding technology to guide the surgeon in real time, and the list of clinical application is growing fast, especially in cancer surgery [8, 22–24]. PG identification by NIR auto-fluorescence is fast, safe, non-invasive, and easy to use; here, we have shown that it is feasible intraoperatively with a commercially available NIR imaging clinical device.
References
Binder-Foucard F, Bossard N, Delafosse P et al (2014) Cancer incidence and mortality in France over the 1980–2012 period: solid tumors. Rev Epidemiol Sante Publique 62:95–108. doi:10.1016/j.respe.2013.11.073
Shaha AR (2004) Implications of prognostic factors and risk groups in the management of differentiated thyroid cancer. Laryngoscope 114:393–402. doi:10.1097/00005537-200403000-00001
Kim TY, Kim WG, Kim WB, Shong YK (2014) Current status and future perspectives in differentiated thyroid cancer. Endocrinol Metab (Seoul) 29:217–225. doi:10.3803/EnM.2014.29.3.217
Hartl DM, Brasnu DF, Shah JP et al (2013) Is open surgery for head and neck cancers truly declining? Eur Arch Otorhinolaryngol 270:2793–2802. doi:10.1007/s00405-012-2322-y
Christou N, Mathonnet M (2013) Complications after total thyroidectomy. J Visc Surg 150:249–256. doi:10.1016/j.jviscsurg.2013.04.003
Lorente-Poch L, Sancho JJ, Ruiz S, Sitges-Serra A (2015) Importance of in situ preservation of parathyroid glands during total thyroidectomy. Br J Surg 102:359–367. doi:10.1002/bjs.9676
Mittendorf EA, McHenry CR (2004) Complications and sequelae of thyroidectomy and an analysis of surgeon experience and outcome. Surg Technol Int 12:152–157
Vahrmeijer AL, Hutteman M, van der Vorst JR et al (2013) Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol 10:507–518
Hadjipanayis CG, Jiang H, Roberts DW, Yang L (2011) Current and future clinical applications for optical imaging of cancer: from intraoperative surgical guidance to cancer screening. Semin Oncol 38:109–118. doi:10.1053/j.seminoncol.2010.11.008
Paras C, Keller M, White L et al (2011) Near-infrared autofluorescence for the detection of parathyroid glands. J Biomed Opt 16:67012–67014
McWade MA, Paras C, White LM et al (2013) A novel optical approach to intraoperative detection of parathyroid glands. Surgery 154:1371–1377. doi:10.1016/j.surg.2013.06.046
McWade M, Paras C, White LM et al (2014) Label-free intraoperative parathyroid localization with near-infrared autofluorescence imaging. J Clin Endocrinol Metab 99:4574–4580. doi:10.1210/jc.2014-2503
Lorente-Poch L, Sancho JJ, Munoz-Nova JL et al (2015) Defining the syndromes of parathyroid failure after total thyroidectomy. Gland Surg 4:82–90. doi:10.3978/j.issn.2227-684X.2014.12.04
Guimaraes AV, Brandao LG, Dedivitis RA (2010) Contact endoscopy for identifying the parathyroid glands during thyroidectomy. Acta Otorhinolaryngol Ital 30:20–26
Suh YJ, Choi JY, Chai YJ et al (2014) Indocyanine green as a near-infrared fluorescent agent for identifying parathyroid glands during thyroid surgery in dogs. Surg Endosc. doi:10.1007/s00464-014-3971-2
Takeuchi S, Shimizu K, Shimizu K Jr et al (2014) Identification of pathological and normal parathyroid tissue by fluorescent labeling with 5-aminolevulinic acid during endocrine neck surgery. J Nippon Med Sch 81:84–93
Antakia R, Gayet P, Guillermet S et al (2014) Near infrared fluorescence imaging of rabbit thyroid and parathyroid glands. J Surg Res 192:480–486. doi:10.1016/j.jss.2014.05.061
Hyun H, Park MH, Owens EA et al (2015) Structure-inherent targeting of near-infrared fluorophores for parathyroid and thyroid gland imaging. Nat Med 21:192–197. doi:10.1038/nm.3728
Chakedis JM, Maser C, Brumund KT, Bouvet M (2015) Indocyanine green fluorescence-guided redo parathyroidectomy. BMJ Case Rep. doi:10.1136/bcr-2015-211778
McWade MA, Sanders ME, Broome JT et al (2015) Establishing the clinical utility of autofluorescence spectroscopy for parathyroid detection. Surgery. doi:10.1016/j.surg.2015.06.047
Stavrakis AI, Ituarte PH, Ko CY, Yeh MW (2007) Surgeon volume as a predictor of outcomes in inpatient and outpatient endocrine surgery. Surgery 142:887–899. doi:10.1016/j.surg.2007.09.003
Mondal SB, Gao S, Zhu N et al (2014) Real-time fluorescence image-guided oncologic surgery. Adv Cancer Res 124:171–211. doi:10.1016/B978-0-12-411638-2.00005-7
Zhu B, Sevick-Muraca EM (2015) A review of performance of near-infrared fluorescence imaging devices used in clinical studies. Br J Radiol 88:20140547. doi:10.1259/bjr.20140547
de Boer E, Harlaar NJ, Taruttis A et al (2015) Optical innovations in surgery. Br J Surg 102:e56–e72. doi:10.1002/bjs.9713
Acknowledgments
The authors wish to thank the technicians of the Biopathology Department and the operating room staff of Head and Neck Surgery Department of Gustave Roussy for their precious help. This work was supported by the French National Cancer League (Ligue National Contre le Cancer: 1FI11687PIAE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or competing financial interests in the subject matter or materials discussed in the manuscript.
Rights and permissions
About this article
Cite this article
De Leeuw, F., Breuskin, I., Abbaci, M. et al. Intraoperative Near-infrared Imaging for Parathyroid Gland Identification by Auto-fluorescence: A Feasibility Study. World J Surg 40, 2131–2138 (2016). https://doi.org/10.1007/s00268-016-3571-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3571-5