Abstract
Objective
The purpose of this article is to systematically analyse the randomized, controlled trials (RCTs) comparing Ferguson or closed haemorrhoidectomy (CH) versus open haemorrhoidectomy (OH) or Milligan–Morgan haemorrhoidectomy in the management of haemorrhoidal disease (HD).
Methods
RCTs on the effectiveness of CH and OH in the management of HD were analysed systematically using RevMan®, and combined outcome was expressed as odds ratio (OR) and standardized mean difference.
Results
Eleven CRTs encompassing 1326 patients were analysed systematically. There was significant heterogeneity among included trials. Therefore, in the random effects model, CH was associated with a reduced post-operative pain (SMD, −0.36; 95 % CI, −0.64, −0.07; z = 2.45; p = 0.01), faster wound healing (OR, 0.08; 95 % CI, 0.02, 0.24; z = 4.33; p < 0.0001), lesser risk of post-operative bleeding (OR, 0.50; 95 % CI, 0.27, 0.91; z = 2.27; p < 0.02) and prolonged duration of operation (SMD, 6.10; 95 % CI, 3.21, 8.98; z = 4.13; p < 0.0001). But the variables such as pain on defecation (SMD, −0.33; 95 % CI, −0.68, 0.03; z = 1.82; p = 0.07), length of hospital stay, post-operative complications, HD recurrence and risk of surgical site infection were similar in both groups.
Conclusion
CH has clinically measurable advantages over OH in terms of reduced post-operative pain, lower risk of post-operative bleeding and faster wound healing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of haemorrhoidal disease (HD) ranges, according to different studies, from 4.4 to 86 % [1–4]. Surgical excision of advanced haemorrhoids in the form of haemorrhoidectomy has been reported with numerous complications. The major complications include sphincter dysfunction (up to 25 %), in 75 % cases pain, severe enough to eliminate patients from professional life for up to 3 weeks, bleeding in 5–15 % patients, and a 30 % risk of recurrent disease [4]. Despite these complications, haemorrhoidectomy is still considered an effective treatment of third-degree and fourth-degree haemorrhoids [5]. It can be performed by the open or closed technique [6, 7]. In Europe, the Milligan–Morgan procedure or open haemorrhoidectomy (OH) [6] is more frequently practised, whereas in the United States of America the closed haemorrhoidectomy (CH) procedure, as described by Ferguson and Heaton [7], is the most popular [8]. CH is purported to be a less painful procedure and associated with faster wound healing due to primary wound closure [6, 9–11]. However, the conflicting outcomes following both procedures have been debated in the published literature and several controversies with regards to post-operative pain still need clarification. The purpose of this article is to systematically analyse the randomized, controlled trials (RCTs) comparing CH versus OH in the management of HD.
Methods
Relevant prospective randomized, controlled trials (irrespective of type, language, gender, blinding, sample size or publication status) on CH versus OH for the management of HD until May 2014 were included in this review. The Cochrane Colorectal Cancer Group (CCCG) Controlled Trial Register, the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library, Medline, EMBASE and Science Citation Index Expanded were searched until May 2014 using the medical subject headings (MeSH) terms “third-degree haemorrhoids”, “fourth-degree haemorrhoids”, “prolapsing haemorrhoids” and “haemorrhoidal disease” in combination with “open haemorrhoidectomy”, “Ferguson haemorrhoidectomy”, “closed haemorrhoidectomy”, “Milligan–Morgan haemorrhoidectomy” and “surgical haemorrhoidectomy” were searched. Boolean operators (AND, OR, NOT) were appropriately utilized to narrow and widen the search results. The published titles from the resultant search were scrutinized closely, and their suitability was determined for potential inclusion into this study. The references from selected published articles were also checked as a further search tool to find additional studies. For inclusion in the meta-analysis, a study had to meet the following criteria: (I) randomized, controlled trial; (II) comparison between CH and OH; (III) evaluation of post-operative pain; (IV) main outcome measures reported preferably as an intention-to-treat (ITT) analysis; and (V) trials in surgical patients who had undergone procedure for third-degree and fourth-degree haemorrhoids. Two reviewers using a predefined meta-analysis form extracted data from each study which resulted in satisfactory inter-observer agreement. The extracted data contained information regarding the name of the authors, title of the study, journal in which the study was published, country and year of the study, treatment regimen, length of the therapy, testing sample size (with sex differentiation if applicable), the number of patients receiving each regimen and within the group the number of patients who succeeded and the number of patients who failed the allocated treatment, the patient compliance rate in each group, the number of patients reporting complications and the number of patients with absence of complications in each arm.
The software package RevMan 5.2.12 [12, 13], provided by the Cochrane Collaboration, was used for the statistical analysis. The odds ratio (OR) with a 95 % confidence interval (CI) was calculated for binary data, and the standardized mean difference (SMD) with a 95 % CI was calculated for continuous variables. The random effects model [14, 15] was used to calculate the combined outcomes of both binary and continuous variables. Heterogeneity was explored using the chi2 test, with significance set at p < 0.05, and was quantified [16] using I 2 test, with a maximum value of 30 % identifying low heterogeneity [16]. The Mantel–Haenszel method was used for the calculation of OR under the random effect models [17]. In a sensitivity analysis, 0.5 was added to each cell frequency for trials in which no event occurred in either the treatment or control group, according to the method recommended by Deeks et al. [18]. If the standard deviation was not available, then it was calculated according to the guidelines of the Cochrane Collaboration [12]. This process involved assumptions that both groups had the same variance, which may not have been true, and variance was either estimated from the range or from the p value. The estimate of the difference between both techniques was pooled, depending upon the effect weights in results determined by each trial estimate variance. A forest plot was used for the graphical display of the results. The square around the estimate stood for the accuracy of the estimation (sample size), and the horizontal line represented the 95 % CI. The methodological quality of the included trials was initially assessed using the published guidelines of Jadad et al. and Chalmers et al. [19, 20]. Based on the quality of the included randomized, controlled trials, the strength and summary of the evidence were further evaluated by GradePro® [21], a tool provided by the Cochrane Collaboration.
Results
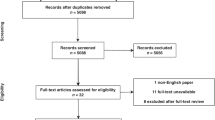
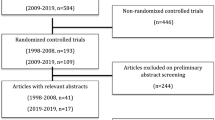
The PRISMA flow chart explaining the outcome of electronic database search and methodology of included studies selection is given in Fig. 1. Eleven randomized, controlled trials [22–32] encompassing 1326 patients undergoing CH or OH for third-degree and fourth-degree haemorrhoids were retrieved from the electronic databases. Six hundred and sixty-three patients underwent CH and 663 patients underwent OH. The characteristics and treatment protocol adopted in included studies are given in Tables 1 and 2, respectively.
Methodological quality of included studies
The methodological quality of included trials (Table 3) was assessed by the published guideline of Jadad et al. and Chalmers et al. [19, 20]. Five trials [25, 26, 29–31] were of poor quality due to lack of adequate randomization technique, absence of blinding, lack of power calculations and in-adequate methods of concealment. Remaining six trials [22–24, 27, 28, 32] were considered of good quality due to adequate methodology following analysis of reported quality variables. Based on the quality of included randomized controlled trials, the strength and summary of evidence was further evaluated by GradePro® [21], a statistical tool provided by the Cochrane Collaboration [Fig. 2].
Post-operative pain score
Six included trials contributed to the combined calculation of this variable as shown in Fig. 3. There was significant heterogeneity [Tau2 = 0.14, chi2 = 18.97, df = 5, (p = 0.002); I 2 = 74 %] among trials. In the random effects model (SMD, −0.36; 95 % CI, −0.64, −0.07; z = 2.45; p = 0.01), the CH was associated with lower pain score post-operatively.
Duration of operation
Seven included trials contributed to the combined calculation of this variable as shown in Fig. 4. There was significant heterogeneity [Tau2 = 14.99, chi2 = 873.05, df = 6, (p = 0.00001); I 2 = 99 %] among trials. In the random effects model (SMD, 6.10; 95 % CI, 3.21, 8.98; z = 4.13; p < 0.0001), the CH was associated with longer duration of operation.
Pain on defecation
Four included trials contributed to the combined calculation of this variable as shown in Fig. 5. There was significant heterogeneity [Tau2 = 0.09, chi2 = 10.90, df = 3, (p = 0.01); I 2 = 72 %] among trials. In the random effects model (SMD, −0.33; 95 % CI, −0.68, 0.03; z = 1.82; p < 0.07), the pain scores were statistically similar following both CH and OH.
Length of hospital stay
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 6. There was significant heterogeneity [Tau2 = 0.35, chi2 = 105.88, df = 10, (p = 0.00001); I 2 = 91 %] among trials. In the random effects model (SMD, −0.36; 95 % CI, −0.73, 0.01; z = 1.89; p < 0.06), the length of hospital stay was statistically similar following both CH and OH.
Post-operative complications
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 7. There was significant heterogeneity [Tau2 = 0.57, chi2 = 24.97, df = 9, (p = 0.003); I 2 = 64 %] among trials. In the random effects model (OR, 0.81; 95 % CI, 0.44, 1.48; z = 0.69; p = 0.49), the risk of post-operative complications was similar in both groups.
Post-operative bleeding
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 8. There was no heterogeneity [Tau2 = 0.12, chi2 = 7.17, df = 6, (p = 0.31); I 2 = 16 %] among trials. In the random effects model (OR, 0.50; 95 % CI, 0.27, 0.91; z = 2.27; p = 0.02), the risk of post-operative bleeding was higher following OH.
Surgical site infection
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 9. There was no heterogeneity [Tau2 = 0.0, chi2 = 3.76, df = 4, (p = 0.44); I 2 = 0 %] among trials. In the random effects model (OR, 2.21; 95 % CI, 0.66, 7.39; z = 1.28; p = 0.20), the risk of post-operative surgical site infection was similar in both groups.
Delayed wound healing
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 10. There was significant heterogeneity [Tau2 = 1.90, chi2 = 34.02, df = 7, (p = 0.0001); I 2 = 79 %] among trials. In the random effects model (OR, 0.08; 95 % CI, 0.02, 0.24; z = 4.33; p < 0.0001), the risk of delayed wound healing was higher following OH.
Recurrence
Eleven included trials contributed to the combined calculation of this variable as shown in Fig. 11. There was no heterogeneity [Tau2 = 0.00, chi2 = 1.22, df = 3, (p = 0.75); I 2 = 0 %] among trials. In the random effects model (OR, 0.91; 95 % CI, 0.56, 1.48; z = 0.38; p = 0.70), the risk of HD recurrence was similar in both groups.
Discussion
Based upon the findings of this review CH was associated with a reduced post-operative pain, faster wound healing, lesser risk of post-operative bleeding but prolonged duration of operation. The variables such as pain on defecation, length of hospital stay, post-operative complications, HD recurrence and the risk of surgical site infection were similar in both groups. Therefore, it is fair to conclude that CH has shown clinically measurable advantages over OH for reduced post-operative pain, lower risk of post-operative bleeding and faster wound healing. Findings of this review are contradictory to previously published meta-analysis of six randomized, controlled trials [33]. Study published by Ho et al. in 2007 advocated the faster wound healing and failed to demonstrate other potential advantages of CH. However, current review of eleven randomized, controlled trials on 1326 patients validated the previously reported variable of faster wound healing in addition to the lower post-operative pain, reduced risk of post-operative bleeding with slightly longer duration of operation.
The included randomized, controlled trials evaluated post-operative pain as primary or secondary outcomes according to the pre-trial analysis strategy. The use of post-operative pain as primary or secondary endpoints following CH or OH was well targeted because the post-operative pain is a major burden of morbidity in patients undergoing HD surgery. This outcome was thoroughly investigated and adequately reported in included randomized, controlled trials. However, present review still has some limitations. Studies included in this review that recruited a small number of patients may not have had sufficient power to reveal small differences in outcomes. Due to fewer numbers of patients and fewer trials on this subject, it is still unwise to generalize the results of this study to all groups of patients undergoing HD surgery. Six included studies were of poor methodological quality. The major methodological flaws in included trials were the lack of a uniformed and standardized pain measuring tool. The surgeons performing procedure were of variable experience and operator dependent pain score differences were not reported adequately. Therefore, a major multicentre, high powered, randomized, controlled trial is mandatory to validate the findings of this review and until then current study may assist colorectal surgeons in decision making about which technique should be adopted to perform haemorrhoidectomy for third-degree and fourth-degree haemorrhoids.
References
Dal Monte PP, Tagariello C, Sarago M et al (2007) Transanal haemorrhoidal dearterialisation: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol 11:333–338
Jayaraman S, Colquhoun PH, Malthaner RA (2007) Stapled hemorrhoidopexy is associated with a higher long-term recurrence rate of internal hemorrhoids compared with conventional excisional hemorrhoid surgery. Dis Colon Rectum 50:1297–1305
Carapeti EA, Kamm MA, McDonald PJ et al (1998) Double-blind randomised controlled trial of effect of metronidazole on pain after day-case haemorrhoidectomy. Lancet 351:169–172
Wałega P, Scheyer M, Kenig J et al (2008) Two-center experience in the treatment of hemorrhoidal disease using Doppler-guided hemorrhoidal artery ligation: functional results after 1-year follow-up. Surg Endosc 22:2379–2383
Wexner SD (2001) The quest for painless surgical treatment of hemorrhoids continues. J Am Coll Surg 193:174–178
Milligan ET, Morgan CN, Jones LE et al (1937) Surgical anatomy of the anal canal and the operative treatment of haemorrhoids. Lancet 2:1119–1124
Ferguson JA, Heaton JR (1959) Closed hemorrhoidectomy. Dis Colon Rectum 2(176):179
Wolfe JS, Munoz JJ, Rosin JD (1979) Survey of haemorrhoidectomy practices: open versus closed techniques. Dis Colon Rectum 22:536–538
Khubchandani IT, Trimpi HD, Sheets JA (1972) Closed haemorrhoidectomy with local anesthesia. Surg Gynecol Obstet 135:955–957
Shaikh AR, Dalwani AG, Soomro N (2013) An evaluation of Milligan-Morgan and Ferguson procedures for haemorrhoidectomy at Liaquat University Hospital Jamshoro, Hyderabad, Pakistan. Pak J Med Sci 29:122–127
Pokharel N, Chhetri RK, Malla B et al (2009) Haemorrhoidectomy: Ferguson’s (closed) vs Milligan Morgan’s technique (open). Nepal Med Coll J 11:136–137
Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5·3·. http://www.cochrane-handbook.org. Accessed 30 May 2015
Review Manager (RevMan) [Computer program] (2008) Version 5.0. The Nordic Cochrane Centre. The Cochrane Collaboration, Copenhagen
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
DeMets DL (1987) Methods for combining randomized clinical trials: strengths and limitations. Stat Med 6:341–350
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Smith GD, Altman DG (2006) Systematic reviews in healthcare. BMJ Publishing, London
Deeks JJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG (eds) Systemic reviews in health care: meta-analysis in context, 2nd edn. BMJ Publication group, London
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Chalmers TC, Smith H Jr, Blackburn B et al (1981) A method for assessing the quality of a randomized control trial. Control Clin Trials 2:31–49
Cochrane IMS http://ims.cochrane.org/revman/otherresources/gradepro/download. Accessed 30 May 2015
Arbman G, Krook H, Haapaniemi S (2004) Closed vs. open hemorrhoidectomy–is there any difference? Dis Colon Rectum 43:31–34
Arroyo A, Pérez F, Miranda E et al (2004) Open versus closed day-case haemorrhoidectomy: is there any difference? Results of a prospective randomised study. Int J Colorectal Dis 19:370–373
Carapeti EA, Kamm MA, McDonald PJ et al (1999) Randomized trial of open versus closed day-case haemorrhoidectomy. Br J Surg 86:612–613
Gaj F, Trecca A, Crispino P (2007) Transfixed stitches technique versus open haemorrhoidectomy. Results of a randomised trial. Chir Ital 59:231–235
Gençosmanoğlu R, Sad O, Koç D et al (2002) Hemorrhoidectomy: open or closed technique? A prospective, randomized clinical trial. Dis Colon Rectum 45:70–75
Ho YH, Seow-Choen F, Tan M et al (1997) Randomized controlled trial of open and closed haemorrhoidectomy. Br J Surg 84:1729–1730
Jóhannsson HO, Påhlman L, Graf W (2006) Randomized clinical trial of the effects on anal function of Milligan-Morgan versus Ferguson haemorrhoidectomy. Br J Surg 93:1208–1214
Mik M, Rzetecki T, Sygut A et al (2008) Open and closed haemorrhoidectomy for fourth degree haemorrhoids–comparative one center study. Acta Chir Iugosl 55:119–125
Khalil-ur-Rehman Hasan A, Taimur M et al (2011) A comparison between open and closed hemorrhoidectomy. J Ayub Med Coll Abbottabad 23:114–116
Uba AF, Obekpa PO, Ardill W (2004) Open versus closed haemorrhoidectomy. Niger Postgrad Med J 11:79–83
You SY, Kim SH, Chung CS et al (2005) Open vs. closed haemorrhoidectomy. Dis Colon Rectum 48:108–113
Ho YH, Buettner PG (2007) Open compared with closed haemorrhoidectomy: meta-analysis of randomized controlled trials. Tech Coloproctol 11:135–143
Authors Contribution
Study conception: Mr MS Sajid, MBBS, MBA, MSc, FRCS, Specialist Registrar Colorectal Surgery; Mr MK Baig, MBBS, MD, FRCS, Consultant Colorectal Surgeon. Design: Mr MS Sajid, Mr MI Bhatti, MBBS, FRCS, Specialist Registrar Colorectal Surgery. Literature search: Mr MS Sajid, Mr MI Bhatti. PRISMA flow chart for study selection: Mr MS Sajid, Mr MI Bhatti, Mr MK Baig. Data acquisition: Mr MS Sajid, Mr I Bhatti. Data confirmation: Mr MK Baig. Data analysis: Mr MS Sajid, Mr MK Baig, Mr I Bhatti. Data interpretation: Mr MS Sajid, Mr MK Baig, Mr WFA Miles, Mr MI Bhatti. Proofreading of the article: Mr MK Baig. Final approval of the version to be published: Mr MS Sajid, Mr MI Bhatti, Mr MK Baig.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None to declare.
Disclosures
All authors have read the manuscript and agreed for submission. We also declare no conflict of interest, no financial disclosure needs be declared and we do not have any political interest in the publication of this article. We are happy to transfer all publishing rights to CD and associated companies for this article if accepted for publication.
Rights and permissions
About this article
Cite this article
Bhatti, M.I., Sajid, M.S. & Baig, M.K. Milligan–Morgan (Open) Versus Ferguson Haemorrhoidectomy (Closed): A Systematic Review and Meta-Analysis of Published Randomized, Controlled Trials. World J Surg 40, 1509–1519 (2016). https://doi.org/10.1007/s00268-016-3419-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3419-z