Abstract
Backgrounds
The neutrophil–lymphocyte ratio (NLR) is a simple and low-cost index that may be a benchmark for systemic inflammatory response and antitumor immunity. The goal of the study was to investigate the prognostic value of preoperative NLR in patients with lung adenocarcinoma after complete resection.
Methods
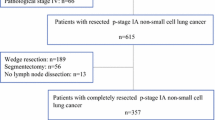
The subjects were 361 consecutive patients with lung adenocarcinoma who underwent complete resection between 2000 and 2009. Perioperative clinical and laboratory data were evaluated retrospectively. The cohort was divided using the cut-off value for preoperative NLR identified in receiver operating characteristic analysis. Correlations of NLR with clinicopathological characteristics and prognosis were examined.
Results
A high NLR was significantly correlated with a smoking history >10 pack-years (p = 0.023), pathological stage II or III (p < 0.001), lymphatic invasion (p = 0.003), and pleural invasion (p = 0.039). In univariate analysis, the high NLR group had significantly lower 5-year overall survival (86.0 vs. 77.1 %, p < 0.001) and 5-year recurrence-free survival (75.1 vs. 59.9 %, p < 0.001). Multivariate analysis showed that NLR was an independent prognostic factor (hazard ratio 1.822, 95 % confidence interval 1.133–2.931, p = 0.013).
Conclusion
These results show that preoperative NLR is an independent prognostic factor in patients with lung adenocarcinoma after complete resection. NLR may reflect host immunity and systemic inflammation that facilitates tumor growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-small cell lung cancer (NSCLC) is the leading cause of cancer-related death worldwide [1]. Among NSCLCs, cases of lung adenocarcinoma have gradually increased and now accounts for almost 40 % of NSCLCs in developed countries [2]. Surgical resection, if possible and appropriate, is the only curative treatment for NSCLC. However, despite recent progress in diagnostic and therapeutic approaches, approximately 50 % of NSCLC cases have tumor recurrence or death after complete resection [3, 4]. These patients may have occult metastasis at the time of surgery and a tumor microenvironment that facilitates cancer progression. Thus, a more accurate prognostic and therapeutic marker is required that reflects this kind of microenvironment.
The neutrophil–lymphocyte ratio (NLR) has been proposed as a simple and low-cost prognostic marker in various cancers, and may be a benchmark for a systemic inflammatory response and antitumor immunity [5]. In the current work, we examined the potential role of NLR as a prognostic factor in lung adenocarcinoma. We note that there are many biological differences between lung adenocarcinoma and NSCLCs with other histology, in terms of driver gene mutations [2], expression of anticancer immunity-related molecules [6–8], and characteristics of the tumor infiltrative lymphocyte [9, 10]. Given this background, we hypothesized that the prognostic significance of preoperative NLR in adenocarcinoma may differ from that in NSCLCs with other histology. Thus, the aim of this study was to examine whether preoperative NLR is a prognostic factor in patients with completely resected lung adenocarcinoma.
Patients and methods
The subjects were patients who underwent surgical resection for primary lung adenocarcinoma at the Tokyo Metropolitan Cancer and Infectious Disease Center Komagome Hospital between January 2000 and March 2009. Patients who underwent limited resection were excluded. Informed consent was obtained from all patients and the study was approved by the Institutional Review Board.
Clinicopathological data were collected from medical records of each patient. Uniform preoperative evaluations included a physical examination, blood chemistry analysis, measurement of tumor markers, bronchoscopy, chest radiography, computed tomography, brain MRI, and bone scintigraphy. Since 2004, integrated positron emission tomography and a CT (PET/CT) scan has also been performed if appropriate. Patients underwent lobectomy, bilobectomy, or pneumonectomy with systematic lymph node dissection for complete resection of the primary lesion. If necessary, combined resection of organs with tumor invasion was also performed. The preoperative NLR was calculated based on blood counts performed within a week before surgery in each patient.
Pathology reports were also reviewed. Cases were diagnosed according to the current World Health Organization histological classification [11] and were staged according to the Seventh Edition of the Tumor Node Metastasis Classification of the International Union Against Cancer [12]. Vascular invasion was diagnosed by identifying conspicuous clusters of intravascular cancer cells surrounded by an elastic layer with Victoria Blue van Gieson staining. Lymphatic invasion was defined as the presence of clusters of tumor cells within the lymphatic endothelial lining in lumen with a close relationship with venous vessels. In cases with unclear findings, immunohistochemical staining using antibodies specific for endothelial cells (CD31 and D2-40; Dako, Glostrup, Denmark) was performed.
Based on the postoperative follow-up policy of our department, we examined patients at 3-month intervals for the first 3 years and typically at 6-month intervals thereafter on an outpatient basis, with the aim of continuing follow-up for 10 years after surgery. Patients were routinely evaluated using physical examinations, chest radiography, chest CT, and blood examinations, including serum tumor markers, on an outpatient basis. If symptoms or signs of recurrence were detected, further examinations were performed, including CT of the chest and abdomen, brain MRI, bone scintigraphy, and PET/CT. Lesions that were suspected to be possible recurrence were subjected to biopsy for histological confirmation, if necessary.
The optimal cut-off value for NLR as a prognostic factor was defined as the closest point to the upper left-hand corner on a receiver operating characteristic (ROC) curve. Cut-off values for age during surgery and smoking history were determined as the respective medians of the cohort. The cut-off point for serum CEA was 5.0 ng/ml (based on the manufacturer’s instructions in the kit). Overall survival (OS) was measured from the date of surgery to the date of death from any cause or the date on which the patient was last known to be alive. Survival curves were plotted using the Kaplan–Meier method and comparisons were made by log-rank test in univariate analysis. The recurrence-free survival (RFS) time was measured as the interval between the date of surgery and the date of recurrence, the date of death from any cause, or the most recent date on which the patient was last known to be alive. To identify independent prognostic factors, multivariate analysis was conducted using a Cox proportional hazard model. Two-category comparisons were performed by Fisher exact test for categorical variables. All tests were two-sided and p values < 0.05 were considered to be significant. All statistical analyses were performed using SPSS (ver. 22; SPSS Inc., Chicago, IL).
Results
A total of 361 consecutive patients with complete medical and follow-up data were included in the analysis. The study cohort included 160 men (44.3 %) and 201 women (55.7 %), and had a mean age of 68 years (range 19–87 years; standard deviation: 10.7 years). Of the 361 patients, 347 (96.1 %) underwent lobectomy, 11 (3.0 %) underwent bilobectomy, and 3 (0.8 %) underwent pneumonectomy. There were total of 80 patients who received adjuvant chemotherapy. 12 patients with stage IB disease underwent oral UFT and 68 patients underwent cisplatin-based chemotherapy. The median follow-up time was 69.0 months (range 2–166 months). The patients had a mean neutrophil count of 3535 ± 1508/mm3, a mean lymphocyte count of 1720 ± 1575/mm3, and a mean NLR of 2.26 ± 1.53.
The optimal cut-off of NLR to test the predictive ability for disease recurrence was determined from a ROC curve (Fig. 1). The sensitivity and specificity for predicting recurrence after resection were 65.6 and 66.9 %, respectively, at a cut-off of 2.495 for NLR, with an area under the curve (AUC) of 0.670. Thus, a cut-off of 2.5 for NLR was used in the following analysis.
A comparison of clinicopathological factors in cases with high and low NLRs (Table 1) showed that patients with a smoking history ≥10 pack-years (p = 0.023), pathological stage II or III (p < 0.001), lymphatic invasion (p = 0.003), and pleural invasion (p = 0.039) were significantly more common in the high NLR group. In a univariate prognostic analysis using the Kaplan–Meier method (Table 2), the clinically significant survival predictors were gender (male vs. female, p = 0.007), smoking history (<10 vs. ≥ 10 pack-years, p = 0.042), pathological stage (I vs. II–III, p = 0.004), lymphatic invasion (absence vs. presence, p < 0.001), vascular invasion (absence vs. presence, p < 0.001), pleural invasion (absence vs. presence, p < 0.001), and NLR (<2.5 vs. ≥2.5, p < 0.001).
High NLR was associated with poorer OS (5-year OS, 86.0 % for low NLR vs. 77.1 % for high NLR; p < 0.001; Fig. 2a). In addition, high NLR was also associated with poorer RFS (5-year RFS, 75.1 % for low NLR vs. 59.9 % for high NLR; p < 0.001; Fig. 2b).
Kaplan–Meier survival curves. a The 5-year overall survival rates of patients with low NLR (<2.5) and high NLR (≥2.5) were 86.0 and 77.1 %, respectively, and OS in low NLR cases was significantly longer than that in high NLR cases (p < 0.001). b The 5-year RFS rates of patients with low NLR and high NLR were 75.1 and 59.9 %, respectively, and RFS in patients with low NLR was also significantly longer than that in patients with high NLR (p < 0.001)
To determine whether NLR was an independent significant prognostic factor, a multivariate analysis was performed, using the seven factors shown to be significant survival predictors in univariate analysis as covariates in the Cox proportional hazard model. The results (Table 3) showed that pathological stage II-III (hazard ratio (HR) = 2.018, 95 % confidence interval (CI) 1.185–3.436, p = 0.010), pleural invasion (HR = 2.289, 95 % CI 1.353–3.874, p = 0.002), vascular invasion (HR = 2.433, 95 % CI 1.432–4.132, p = 0.001), and NLR ≥ 2.5 (HR = 1.822, 95 % CI 1.133–2.931, p = 0.013) were independent prognostic factors.
In addition, we analyzed the correlation between NLR and the initially observed recurrence site to investigate whether NLR could influence disease recurrence patterns, (Table 4). In total, 100 (27.7 %) patients had disease recurrence, 42 cases with NLR ≥ 2.5 and 58 cases with NLR < 2.5. Contralateral lung was the most common site of distant metastasis in both the low NLR group (18 of 34) and high NLR group (16 of 29). Among the patients who developed recurrences, 34 patients with NLR < 2.5 and 29 patients with NLR ≥ 2.5 developed distant metastases (including patients with both distant and locoregional recurrence). The proportion of patients who developed distant metastases was significantly higher in the high NLR group than in the low NLR group (p < 0.001, χ 2 test). On the other hand, the proportion of patients who developed locoregional recurrence was not significantly different between the two groups (p = 0.236).
Discussion
The results of the study clearly show that increased preoperative NLR in the peripheral blood is an independent prognostic factor for OS and RFS after complete resection of lung adenocarcinoma. To the best of our knowledge, this is the first report to show that NLR is an independent prognostic factor in a population limited to patients with lung adenocarcinoma.
An increased pretreatment NLR is correlated with a poor prognosis in patients with gastric cancer [13], breast cancer [14], colorectal cancer [15], pancreatic cancer [16], renal cell carcinoma [17], and soft-tissue sarcoma [18]. Increased preoperative NLR is also associated with higher tumor stage and is an independent predictor of survival in resected NSCLC [19–21]. Our results are consistent with these studies, in which the cohorts were more diverse populations with surgically resected NSCLC. In a previous study, we found that NLR of patients with adenocarcinoma was significantly lower than that for other histology. Procter et al. also found that the prognostic value of NLR varied according to tumor histology and origin in patients with various types of cancer [5]. In the current study, we also found a significant correlation of NLR with histological invasive factors of tumors, such as higher pathological stage and presence of vascular and pleural invasion, which are widely accepted as poor prognostic factors. The greater proportion of the distant recurrence as an initial recurrence site could partly support to explain the unfavorable outcome of high NLR cases, which agrees our previous data [22]. This could partly explain the worse prognosis of the high NLR cases. On the other hand, we should note that the multivariate analysis in this study revealed that the prognostic impact of the preoperative NLR was lesser than that of pathological stage, pleural invasion, and vascular invasion in the current cohort.
The tumor microenvironment is a major contributor to tumor progression, along with the genetic characteristics of the tumor, and is mainly influenced by inflammatory cells including leukocytes [23]. Each step of tumor progression, including proliferation, migration, inhibition of apoptosis, and promotion of angiogenesis, is affected by inflammatory cells [15, 24, 25]. The abnormal phenotype of the tumor may also stimulate infiltration of inflammatory cells into tissues around the tumor, which facilitates tissue destruction, and subsequent disruption caused by the physical neoplastic growth may trigger more generalized and non-specific inflammatory responses [26]. As a consequence of these inflammatory processes, neutrophils increase and lymphocytes decrease, resulting in an increased NLR with cancer progression [27]. Thus, the NLR is a simple and reliable predictor of survival in patients with cancer [28]. The significant association of an increased NLR with poor OS and poor RFS found in the current study suggests that NLR has oncological relevance and that an increased NLR may reflect a microenvironment facilitating disease progression in patients with lung adenocarcinoma.
An increased NLR has also been associated with outcome in patients with myocardial infarction undergoing coronary intervention [29, 30], chronic kidney disease [31], chronic critical limb ischemia [32], and cerebral stroke [33]. An increased NLR may reflect an inflammatory response and subsequent weakened immune system, which may affect the prognosis of many diseases. Thus, the NLR might be a benchmark of the general condition of patients.
In this study, we set the cut-off value for NLR at 2.5, similar to two previous studies [21, 34], but lower than the value of 5 used in two other studies [19, 20]. Interracial differences in NLR may influence this cut-off, and we have also found differences in NLR according to histology in our previous analyses (data not shown). Thus, we identified an optimal cut-off of 2.5 in the current cohort using a ROC curve to test the predictive ability of NLR for cancer-specific death. This methodological precision is an advantage of the current study prior to previous studies, although linearity of the ROC curve was not investigated. Moreover, the most appropriate cut-off value is still not fully established and the current value could be viewed as arbitrary because we also did not validate the results in different cases. Further work is necessary for the validation of the cut-off value.
To our knowledge, this is the first report showing a prognostic implication of the NLR in a population limited to cases of lung adenocarcinoma. The findings suggest that the prognostic value of NLR in lung adenocarcinoma is similar to that in all NSCLCs, in contrast to our original hypothesis. Expression levels of several molecules related to immunity [8, 35, 36] and characteristics of the tumor-infiltrative lymphocyte [10, 37, 38] in patients with lung cancer support our findings. A treatment strategy according to histological type has recently been established [39], which permits the prognostic significance of several factors to be investigated depending on histological type [36, 40, 41]. This background supports the finding that the NLR, which may reflect inflammatory response and immune status, can predict both OS and RFS in patients with adenocarcinoma. Thus, accurate risk stratification using preoperative NLR according to histology may help with treatment selection. However, the relationship of inflammation and immunity with tumor progression requires further evaluation to identify predictors of survival in patients with lung adenocarcinoma.
It would be of greater concern whether adjuvant chemotherapy can be beneficial for high NLR patients. Thus, we tried to analyze the outcome in high NLR cases and we could not find the significant difference between patients who underwent adjuvant chemotherapy and who did not in both Stage IB and Stage II or III cases (Supplemental Fig. 1). However, the number of patients in each group was very small that there were only 3 of stage IB patients who underwent adjuvant chemotherapy and 4 of stage II or III patients who did not undergo adjuvant chemotherapy among the high NLR cases. There were also significant differences of histological invasive factors including lymphatic invasion, vascular invasion, and pleural invasion, between patients who underwent adjuvant chemotherapy and those who did not undergo adjuvant chemotherapy (Supplemental Table 1). Therefore, we considered that it is not suitable to appropriately compare the outcome between each subgroup in our cohort.
The two major limitations of the study were that it was performed in a retrospective manner in a limited number of patients, which might contribute to selection bias. Therefore, the current data should be followed by further studies with larger number of cases. In addition, values of NLR may change according to time of measurement and medications, although we collected hematological data exclusively within a week before surgery. Within these limitations, our findings show the prognostic value of the NLR for OS and RFS after complete resection of lung adenocarcinoma. Thus, we conclude that the NLR is a simple and readily available prognostic marker that provides an additional level of risk stratification. An increased preoperative NLR is associated with a poorer prognosis and more frequent distant metastasis in patients with lung adenocarcinoma, and this provides useful information for preoperative and postoperative management.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- NLR:
-
Neutrophil–lymphocyte ratio
- CT:
-
Computed tomography
- PET/CT:
-
Positron emission tomography scan and CT scan
- ROC:
-
Receiver operating characteristics
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- AUC:
-
Area under the curve
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
An SJ, Chen ZH, Su J, Zhang XC, Zhong WZ, Yang JJ, Zhou Q, Yang XN, Huang L, Guan JL, Nie Q, Yan HH, Mok TS, Wu YL (2012) Identification of enriched driver gene alterations in subgroups of non-small cell lung cancer patients based on histology and smoking status. PLoS ONE 7:e40109
Asamura H, Goya T, Koshiishi Y, Sohara Y, Eguchi K, Mori M, Nakanishi Y, Tsuchiya R, Shimokata K, Inoue H, Nukiwa T, Miyaoka E, Japanese Joint Committee of Lung Cancer Registry (2008) A Japanese lung cancer registry study: prognosis of 13,010 resected lung cancers. J Thorac Oncol 3:46–52
Goldstraw P, Ball D, Jett JR, Le Chevalier T, Lim E, Nicholson AG, Shepherd FA (2011) Non-small-cell lung cancer. Lancet non-small-cell lung cancer. Lancet 378:1727–1740
Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ (2012) A derived neutrophil and lymphocyte ratio predicts survival in patients with various cancer. Br J Cancer 107:695–699
D’Incecco A, Andreozzi M, Ludovini V, Rossi E, Capodanno A, Landi L, Tibaldi C, Minuti G, Salvini J, Coppi E, Chella A, Fontanini G, Filice ME, Tornillo L, Incensati RM, Sani S, Crinò L, Terracciano L, Cappuzzo F (2015) PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br J Cancer 112:95–102
Ichiki Y, Hanagiri T, Takenoyama M, Baba T, Fukuyama T, Nagata Y, Mizukami M, So T, Sugaya M, Yasuda M, So T, Sugio K, Yasumoto K (2005) Tumor specific expression of survivin-2B in lung cancer as a novel target of immunotherapy. Lung Cancer 48:281–289
Sun PL, Jin Y, Kim H, Seo AN, Jheon S, Lee CT, Chung JH (2013) Survivin expression is an independent poor prognostic marker in lung adenocarcinoma but not in squamous cell carcinoma. Virchows Arch 463:427–436
Black CC, Turk MJ, Dragnev K, Rigas JR (2013) Adenocarcinoma contains more immune tolerance regulatory t-cell lymphocytes (versus squamous carcinoma) in non-small-cell lung cancer. Lung 191:265–270
Nakamura H, Saji H, Ogata A, Hosaka M, Hagiwara M, Kawasaki N, Konaka C, Kato H (2002) Immunologic parameters as significant prognostic factors in lung cancer. Lung Cancer 37:161–169
Travis WDBE, Mueller-Hermelink HK, Harris CC (eds) (2002) World Health Organization classification of tumours: pathology and genetics of tumours of the lung, pleura, thymus and heart. IARC Press, Lyon
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, Postmus PE, Rusch V, Sobin L, International Association for the Study of Lung Cancer International Staging Committee; Participating Institutions (2007) The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2:706–714
Graziosi L, Marino E, De Angelis V, Rebonato A, Cavazzoni E, Donini A (2015) Prognostic value of preoperative neutrophils to lymphocytes ratio in patients resected for gastric cancer. Am J Surg 209:333–337
Yao M, Liu Y, Jin H, Liu X, Lv K, Wei H, Du C, Wang S, Wei B, Fu P (2014) Prognostic value of preoperative inflammatory markers in Chinese patients with breast cancer. Oncol Targets Ther 7:1743–1752
Jaiswal M, LaRusso NF, Burgart LJ, Gores GJ (2000) Inflammatory cytokines induce DNA damage and inhibit DNA repair in cholangiocarcinoma cells by a nitric oxide-dependent mechanism. Cancer Res 60:184–190
Ben Q, An W, Wang L, Wang W, Yu L, Yuan Y (2015) Validation of the pretreatment neutrophil-lymphocyte ratio as a predictor of overall survival in a cohort of patients with pancreatic ductal adenocarcinoma. Pancreas 44:471–477
Pichler M, Hutterer GC, Stoeckigt C, Chromecki TF, Stojakovic T, Golbeck S, Eberhard K, Gerger A, Mannweiler S, Pummer K, Zigeuner R (2013) Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer 108:901–907
Szkandera J, Absenger G, Liegl-Atzwanger B, Pichler M, Stotz M, Samonigg H, Glehr M, Zacherl M, Stojakovic T, Gerger A, Leithner A (2013) Elevated preoperative neutrophil/lymphocyte ratio is associated with prognosis in soft-tissue sarcoma patients. Br J Cancer 108:1677–1683
Pinato DJ, Shiner RJ, Seckl MJ, Stebbing J, Sharma R, Mauri FA (2014) Prognostic performance of inflammation-based prognostic indices in primary operable non-small cell lung cancer. Br J Cancer 110:1930–1935
Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E (2009) Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 137:425–428
Tomita M, Shimizu T, Ayabe T, Yonei A, Onitsuka T (2011) Preoperative neutrophil to lymphocyte ratio as a prognostic predictor after curative resection for non-small cell lung cancer. Anticancer Res 31:2995–2998
Takahashi Y, Horio H, Hato T, Harada M, Matsutani N, Morita S, Kawamura M (2015) Prognostic significance of preoperative neutrophil-lymphocyte ratios in patients with stage I non-small cell lung cancer after complete resection. Ann Surg Oncol. doi:10.1245/s10434-015-4735-5, Jul 22 2015)
Kundu JK, Surh YJ (2008) Inflammation: gearing the journey to cancer. Mutat Res 659:15–30
Jackson JR, Seed MP, Kircher CH, Willoughby DA, Winkler JD (1997) The codependence of angiogenesis and chronic inflammation. FASEB J 11:457–465
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444
Nagtegaal ID, Marijnen CA, Kranenbarg EK, Mulder-Stapel A, Hermans J, van de Velde CJ, van Krieken JH (2001) Local and distant recurrences in rectal cancer patients are predicted by the nonspecific immune response; specific immune response has only a systemic effect–a histopathological and immunohistochemical study. BMC Cancer 1:7
Jilma B, Blann A, Pernerstorfer T, Stohlawetz P, Eichler HG, Vondrovec B, Amiral J, Richter V, Wagner OF (1999) Regulation of adhesion molecules during human endotoxemia. No acute effects of aspirin. Am J Respir Crit Care Med 159:857–863
Teramukai S, Kitano T, Kishida Y, Kawahara M, Kubota K, Komuta K, Minato K, Mio T, Fujita Y, Yonei T, Nakano K, Tsuboi M, Shibata K, Furuse K, Fukushima M (2009) Pretreatment neutrophil count as an independent prognostic factor in advanced non-small cell lung cancer: an analysis of japan Multinational Atrial Organization LC00-03. Eur J Cancer 45:1950–1958
Roxburg CS, McMillan DC (2010) Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 6:149–163
Park JJ, Jang HJ, Oh IY, Yoon CH, Suh JW, Cho YS, Youn TJ, Cho GY, Chae IH, Choi DJ (2013) Prognostic value of neutrophil to lymphocyte ratio in patients presenting ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol 11:55–59
Sen N, Afsar B, Ozcan F, Buyukkaya E, Isleyen A, Akcay AB, Yuzgecer H, Kurt M, Karakas MF, Basar N, Hajro E, Kanbay M (2013) The neutrophil to lymphocyte ratio was associated with impaired myocardial perfusion and long term outcome in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Atherosclerosis 228:203–210
Kocyigit I, Eroglu E, Unal A, Sipahioglu MH, Tokgoz B, Oymak O, Utas C (2013) Role of neutrophil/lymphocyte ratio in prediction of disease progression in patients with stage-4 chronic kidney disease. J Nephrol 26:358–365
Spark JI, Sarveswaran J, Blest N, Charalabidis P, Asthana S (2010) An elevated neutrophil-lymphocyte ratio independently predicts mortality in chronic critical limb ischemia. J Vasc Surg 52:632–636
Gökhan S, Ozhasenekler A, Mansur Durgun H, Akil E, Ustündag M, Orak M (2013) Neutrophil lymphocyte ratios in stroke subtypes and transient ischemic attack. Eur Rev Med Pharmacol Sci 17:653–657
Tomita M, Shimizu T, Ayabe T, Nakamura K, Onitsuka T (2012) Elevated preoperative inflammatory markers based on neutrophil-to lymphocyte ratio and C-reactive protein predict poor survival in resected non-small cell lung cancer. Anticancer Res 32:3535–3538
Uramoto H, So T, Nagata Y, Kuroda K, Shigematsu Y, Baba T, So T, Takenoyama M, Hanagiri T, Yasumoto K (2010) Correlation between HLA alleles and EGFR mutation in Japanese patients with adenocarcinoma of the lung. J Thorac Oncol 5:1136–1142
Zhang Y, Wang L, Li Y, Pan Y, Wang R, Hu H, Li H, Luo X, Ye T, Sun Y, Chen H (2014) Protein expression of programmed death 1 ligand 1 and ligand 2 independently predict poor prognosis in surgically resected lung adenocarcinoma. Oncol Targets Ther 7:567–573
Kinoshita T, Ishii G, Hiraoka N, Hirayama S, Yamauchi C, Aokage K et al (2013) Forkhead box P3 regulatory T cells coexisting with cancer associated fibroblasts are correlated with a poor outcome in lung adenocarcinoma. Cancer Sci 104:409–415
Suzuki K, Kadota K, Sima CS, Nitadori J, Rusch VW, Travis WD, Sadelain M, Adusumilli PS (2013) Clinical impact of immune microenvironment in stage I lung adenocarcinoma: tumor interleukin-12 receptor β2 (IL-12Rβ2), IL-7R, and stromal FoxP3/CD3 ratio are independent predictors of recurrence. J Clin Oncol 31:490–498
Ettinger DS, Akerley W, Borghaei H, Chang AC, Cheney RT, Chirieac LR, D’Amico TA, Demmy TL, Govindan R, Grannis FW Jr, Grant SC, Horn L, Jahan TM, Komaki R, Kong FM, Kris MG, Krug LM, Lackner RP, Lennes IT, Loo BW Jr, Martins R, Otterson GA, Patel JD, Pinder-Schenck MC, Pisters KM, Reckamp K, Riely GJ, Rohren E, Shapiro TA, Swanson SJ, Tauer K, Wood DE, Yang SC, Gregory K, Hughes M, National comprehensive cancer network (2013) Non-small cell lung cancer, version 2.2013. J Natl Compr Canc Netw 11:645–653
Kwon MJ, Seo J, Kim YJ, Kwon MJ, Choi JY, Kim TE, Lee DH, Park S, Shin YK, Han J, Choi YL (2013) Prognostic significance of CD151 overexpression in non-small cell lung cancer. Lung Cancer 81:109–116
Acknowledgments
The authors thank Dr. Keith Kretzmer for the editorial review of this manuscript.
Funding
This work was supported by the institutional grants. The sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takahashi, Y., Kawamura, M., Hato, T. et al. Neutrophil–Lymphocyte Ratio as a Prognostic Marker for Lung Adenocarcinoma After Complete Resection. World J Surg 40, 365–372 (2016). https://doi.org/10.1007/s00268-015-3275-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3275-2