Abstract
Background
Studies reveal that ileal pouch-anal anastomosis (IPAA) has long-term success. These reports, however, use well-selected cohorts and exclude patients presenting with fulminant colitis (FC). Herein, we aimed to characterize long-term functional outcomes in patients with fulminant ulcerative colitis (UC) undergoing IPAA.
Methods
A prospective database identified patients who underwent IPAA between 1998 and 2008. Patients with FC and chronic UC were matched by age, gender, date of surgery, and follow-up duration. Clinical and laboratory parameters, immunomodulator use at the time of surgery, and functional outcomes were compared.
Results
Forty patients with FC and 73 patients with chronic UC were identified. Preoperative albumin, hemoglobin, leukocyte count, and steroid dose were significantly different for those with FC. Average survey follow-up was 5.2 years for FC and 6.7 years for chronic UC patients. Functional outcomes were not significantly different. The 3-year fistula-free rate was 91.4 versus 98.6 % and the 3-year stricture-free rate was 79.3 versus 87.2 % for FC versus chronic UC patients, respectively.
Conclusion
Patients undergoing colectomy for FC secondary to UC have similar long-term functional outcomes after IPAA despite significantly worse presentation. This study confirms that IPAA is an appropriate and durable treatment for patients with FC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery is a common intervention utilized to treat fulminant ulcerative colitis (FC) when patients present with sepsis or when medical therapy has proven ineffective. A number of studies [1–3] have demonstrated successful surgical outcomes in ulcerative colitis (UC) patients who underwent total colectomy with ileal pouch-anal anastomosis (IPAA). This includes significant long-term follow-up, with 92 % pouch success at 20 years [1].
These studies, however, were not comprehensive and failed to represent all patients undergoing IPAA for UC. Few reports have evaluated the outcome of colectomy with eventual IPAA in patients who present with severe disease requiring emergent resection. Further complicating the interpretation of these outcomes is the varying definition of “fulminant” in the literature. Descriptions of UC severity by Truelove and Witts criteria [4] continue to be employed; however, these criteria have been modified [5], renamed, and intermittently utilized so that no single definition is universally accepted [5, 6]. Due to the lack of recent long-term data evaluating the outcomes in patients with FC, we aimed to compare the durability of IPAA in this patient population to those with a less severe presentation.
Materials and methods
Using a prospectively maintained database of colorectal surgical patients, we identified individuals who had undergone a 2- or 3-stage IPAA between the years 1998 and 2008. This database included details pertaining to the initial surgical dates, as well as follow-up survey data related to quality of life, pouch function, and postoperative complications. Patients lacking follow-up survey results or clinical visits at 1 year, those who were pregnant at the time of initial surgery, and patients without a diagnosis of UC at the time of their first operation, were excluded. Once identified, surgical indications were obtained from the operative reports. Patients were classified as fulminant/severe (FC), chronic ulcerative colitis (CUC), or surgery for neoplasm/prophylactic etiology (i.e., dysplasia, FAP). Demographic variables including date of colectomy, gender, age at time of colectomy, and number of years of follow-up were then obtained for all patients. After classification by disease severity at the time of operation, 40 patients with FC were identified. This cohort was then matched by age, gender, and duration of follow-up to 73 patients with CUC. These patient records were further reviewed for laboratory data at time of presentation for colectomy including: lowest hemoglobin and highest leukocyte count, most recent albumin, and need for transfusion within the 2-week period preceding the operative intervention. Clinical data consisting of daily bowel movements, BMI, daily prednisone dose (or prednisone equivalent dose) prior to surgery, and active use of immunomodulator therapy, were also obtained. Long-term quality of life data was extracted from a prospectively maintained database that houses information from patient surveys sent out annually. These surveys consisted of questions pertaining to IPAA function, social impact, or postoperative complications. This study was approved by the Mayo Clinic Institutional Review Board.
Statistical analysis
Descriptive statistics are reported as either number (percentage) or as mean (SD) as appropriate. The association of factors present at clinical presentation and responses to disease status at latest survey were assessed using logistic regression, reporting the odds ratio (OR), and 95 % confidence interval (CI). Three- and five-year complication-free survival estimates were generated using Kaplan–Meier analysis. The association of patient status (FC vs. CUC) with complications was assessed with Cox proportional hazards, reported as hazard ratio (HR), and 95 % CI. The alpha-level was set at 0.05 for statistical significance. All statistical analyses were conducted utilizing SAS (SAS version 9.2; SAS Institute Inc., Cary, NC, USA 2009).
Results
Demographics
A total of 1147 patients between 1998 and 2008 were identified as having undergone a total proctocolectomy with IPAA. Among this cohort, 74 patients were identified as having FC based on the operative report; 40 of these had sufficient follow-up (at least 1 year postoperatively) data to merit inclusion in this study. Additionally, 73 patients with CUC were chosen and matched by age, gender, date of surgery, and duration of follow-up. Refer to Table 1 for a summary of demographic information. The majority (67.3 %) of patients were men and average age at time of colectomy was 38.3 years (range 15–60 years).
Clinical presentation
Laboratory values prior to abdominal colectomy or total proctocolectomy including mean albumin (2.7 vs. 3.8 g/dL, p < 0.01), hemoglobin (8.9 vs. 12.5 g/dL, p < 0.01), and leukocyte count (13.4 × 109/L vs. 8.8 × 109/L, p < 0.01) were significantly worse for patients presenting with FC compared to CUC. In this cohort, 64 % of FC patients required preoperative transfusion, whereas only 3 % of CUC patients needed blood (p ≤ 0.01). Of the other clinical presentation variables, only steroid dosage was significantly different, with a mean daily oral prednisone dose (or equivalent) of 69.7 mg (IQR 60–75) in the FC patients vs. 19.0 mg (IQR 0–33) in the CUC patients, (p < 0.01). Body Mass Index (22.9 in FC vs. 25.6 in CUC) was statistically different (p < 0.01), but likely not clinically significant. The number of patients who had >10 bowel movements per day was not significantly greater for the FC cohort than the CUC cohort (55.2 vs. 36.9 %, p = 0.10); interestingly, both groups had a large proportion of patients with these symptoms. Thirty-five of 41 (85 %) patients with FC underwent a 3-stage procedure, whereas 72 of 73 patients with chronic ulcerative colitis underwent a 2-stage procedure. Among patients who underwent a 3-stage procedure, the mean albumin (4.2 g/dL), hemoglobin (13.1 g/dL), and leukocyte count (6.8 × 109/L) significantly improved prior to their 2nd stage IPAA creation. For the initial colectomy, 40 % of FC cases were completed with laparoscopic/hand-assistance, while 32 % of CUC cases were performed in this fashion.
Short and long-term pouch function
Thirty-day postoperative outcomes were similar for both groups. In total, 4 patients in the FC group (10 %) developed a pelvic abscess within 30 days of their 2-stage procedure. All 4 were successfully managed with IV antibiotics and drain placement. Two of these patients have reported no further problems 11 and 12 years post-IPAA. Of the remaining 2 patients, one developed Crohn’s disease with perianal fistula (11 years post-IPAA) and the other underwent pouch excision with end-ileostomy secondary to perianal fistula formation (12 years post-IPAA). Similarly, 4 patients in the CUC group developed a pelvic abscess within 30 days of their total proctocolectomy (TPC) with IPAA. Two of these patients continue to have chronic pouchitis (9 and 11 years post-IPAA) and 2 have reported no long-term complications or problems with their pouch at 3 and 8 years of follow-up.
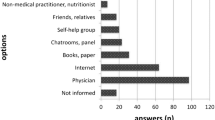
Mean survey follow-up was 5.2 years for the FC group and 6.6 years for the CUC group. No significant difference was noted with IPAA function or social factors (refer to Table 2). The only long-term postoperative complication with a significant difference was occurrence of pouchitis, with 5-year survival estimates of 52.9 %, (95 % CI 37.5–74.5 %) and 38.4 %, (95 % CI 28.1–52.4 %) for FC and CUC, respectively. In addition, patients with FC had significantly lower risk of pouchitis, (HR = 0.56, 95 % CI 0.32–0.989, p value = 0.046). The above rates reflect the total prevalence of any complication, as notation of a complication on prior surveys was included irrespective of whether the complication resolved on subsequent evaluation. These findings are summarized in Table 2 and Fig. 1.
Discussion
Our results reveal that long-term outcomes for patients who present with fulminant ulcerative colitis and had eventual restoration of continuity with IPAA are no different in regard to postoperative complications or pouch function when compared to patients who present with less severe disease.
Ulcerative colitis has varying degrees of severity which may fluctuate over time and require medical, surgical, or combined treatment modalities. The majority of patients with UC have a mild or moderate form of the disease, for which maintenance medical therapies (including aminosalicylates and steroids) have long been utilized. Newer generations of immunomodulators and biologics such as cyclosporine and infliximab, are increasingly being prescribed for patients with steroid-refractory colitis. Patients presenting for surgical intervention typically are intolerant to medical therapies, have chronic poorly controlled colitis, or presence of dysplasia on histopathology. Data on the short and long-term outcomes in this cohort are favorable; IPAA has been shown to be successful in 92 % of patients at 20 years [1]. Infrequently, there are patients who are unable to be medically managed due to the acute or severe nature of their disease. These patients have historically either been excluded from existing studies on functional outcomes or included within the general cohort. Reports which have focused on FC have therefore been small and often have a shorter follow-up period [7, 8]. Harms et al. [8] examined only 23 patients, of which only 20 met criteria for severe ulcerative colitis. Disease severity in this cohort was not significant enough to merit a 3-stage procedure; only 3 patients in this study required an ileostomy. Another study by Ziv et al. [7] evaluated the outcomes of 12 patients described as having FC. They found that in 11 surviving patients, pouch function was good to excellent, with a median follow-up of 29 months. While these are promising initial studies, the small sample size precludes formulation of definitive conclusions. A study from the Mayo Clinic in 2007 analyzed the short-term outcomes (30 days) and complications in 50 patients who underwent laparoscopic colectomy with IPAA after presenting with severe or fulminant ulcerative colitis as defined by Truelove and Witt’s criteria [9]. Although long-term results were not an emphasis of this study, the focus on the laparoscopic approach limited the study population by excluding patients deemed too sick to tolerate laparoscopy. This current study corroborates the short-term findings by Holubar et al. [9] in the laparoscopic population and extends these results to all patients with FC irrespective of operative approach. With the addition of long-term follow-up in our current cohort, we conclude that a laparoscopic approach can be safely utilized for patients presenting with fulminant disease.
In this review of our practice, we evaluated the subgroup of patients described clinically as fulminant or toxic and presenting with systemic manifestations of disease. Historic criteria for defining severity of ulcerative colitis have focused on vital signs, stool frequency, and erythrocyte sedimentation rate (ESR) [4]. More current measures have incorporated hemoglobin levels [5]. While these criteria reasonably reflect the acute physiology of fulminant disease, they do not fully capture the increased morbidity associated with unsuccessful medical therapy. Compared to their CUC matched cohort, this population demonstrated significantly worse anemia, hypoalbuminemia, and higher preoperative doses of steroids; all factors which have been associated with increased postoperative complications such as pelvic sepsis [10, 11]. This is critical information because pelvic sepsis is the single largest risk factor for pouch dysfunction long term. While these patients have the benefit of a 3-stage operation to allow for convalescence and recovery from their acute injury, it remained to be seen if their long-term outcomes would mirror those of less severe disease.
There are several limitations to our study. First, since this is a single institution study based partly on a voluntary patient survey, there are many potential biases. We were unable to define our patients as fulminant based on historic criteria; some parameters such as initial vital signs were not recoverable due to the retrospective nature of the study. However, other characteristics clearly indicate the severity of the disease. This had a notable impact on the decision of the operative surgeons to pursue a 3-stage procedure. The majority of our patients underwent surgical intervention when immunomodulators such as Infliximab were still investigational for the treatment of inflammatory bowel disease. Since FDA approval in 2005, an increasing number of patients have undergone salvage therapy for severe disease [12–14]. There is conflicting data regarding the impact of these drugs on short-term outcomes for this population since their adoption [15–17]. As more patients present in advanced immunocompromised states due to these powerful new medications, it is unclear if long-term outcomes will be worse. Anecdotally, we have noticed over the past several years that more of these patients undergo a 3-stage approach.
Conclusion
The short and long-term functional outcomes for IPAA in patients with FC versus CUC do not appear to be significantly different. Although a 3-stage procedure may be necessary, these patients can be counseled with confidence that the severity of their disease at presentation, does not preclude them from having a favorable outcome with a reasonable quality of life.
References
Hahnloser D et al (2007) Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg 94(3):333–340
Michelassi F et al (2003) Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg 238(3):433–441 (discussion 442–445)
Rokke O et al (2011) Long-term followup with evaluation of the surgical and functional results of the ileal pouch reservoir in restorative proctocolectomy for ulcerative colitis. ISRN Gastroenterol 2011:625842
Edwards FC, Truelove SC (1963) The course and prognosis of ulcerative colitis. Gut 4:299–315
Satsangi J et al (2006) The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 55(6):749–753
Hanauer SB (1996) Inflammatory bowel disease. N Engl J Med 334(13):841–848
Ziv Y et al (1995) Safety of urgent restorative proctocolectomy with ileal pouch-anal anastomosis for fulminant colitis. Dis Colon Rectum 38(4):345–349
Harms BA et al (1994) Management of fulminant ulcerative colitis by primary restorative proctocolectomy. Dis Colon Rectum 37(10):971–978
Holubar SD et al (2009) Minimally invasive subtotal colectomy and ileal pouch-anal anastomosis for fulminant ulcerative colitis: a reasonable approach? Dis Colon Rectum 52(2):187–192
Hoda KM et al (2008) Predictors of pouchitis after ileal pouch-anal anastomosis: a retrospective review. Dis Colon Rectum 51(5):554–560
Heuschen UA et al (2002) Risk factors for ileoanal J pouch-related septic complications in ulcerative colitis and familial adenomatous polyposis. Ann Surg 235(2):207–216
Jarnerot G et al (2005) Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology 128(7):1805–1811
Ferrante M et al (2008) Long-term outcome after infliximab for refractory ulcerative colitis. J Crohns Colitis 2(3):219–225
Reinisch W et al (2012) Recommendations for the treatment of ulcerative colitis with infliximab: a gastroenterology expert group consensus. J Crohns Colitis 6(2):248–258
Selvasekar CR et al (2007) Effect of infliximab on short-term complications in patients undergoing operation for chronic ulcerative colitis. J Am Coll Surg 204(5):956–962 (discussion 962–963)
Mor IJ et al (2008) Infliximab in ulcerative colitis is associated with an increased risk of postoperative complications after restorative proctocolectomy. Dis Colon Rectum 51(8):1202–1207 (discussion 1207–1210)
Kunitake H et al (2008) Perioperative treatment with infliximab in patients with Crohn’s disease and ulcerative colitis is not associated with an increased rate of postoperative complications. J Gastrointest Surg 12(10):1730–1736 (discussion 1736–1737)
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fasen, G.S., Pandian, T.K., Pavey, E.S. et al. Long-Term Outcome of IPAA in Patients Presenting with Fulminant Ulcerative Colitis: A Matched Cohort Study. World J Surg 39, 2590–2594 (2015). https://doi.org/10.1007/s00268-015-3114-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3114-5