Abstract
Purpose
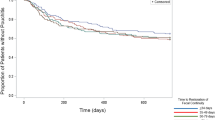
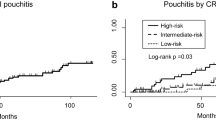
The primary end point of this study was to determine the risk factors that predict chronic pouchitis in those patients having ileal pouch-anal anastomosis.
Methods
A total of 237 patients with ulcerative colitis and undergoing ileal pouch-anal anastomosis by one surgeon at Oregon Health & Science University from 1993 to 2003 were evaluated. Data were gathered via retrospective chart reviews and by a questionnaire administered by telephone in 2004. Patients were excluded if there was less than one-year follow-up documented in the chart or they could not be contacted by telephone (n = 62), postoperative diagnosis of Crohn’s disease (n = 3), failed ileoanal procedure (n = 1), and one-stage ileal pouch-anal anastomosis (n = 3), leaving 167 patients for evaluation. Patients were defined as having chronic pouchitis (>3 episodes of pouchitis) or no pouchitis (≤ 3 episodes of pouchitis). Potential risk factors included number of operations used to perform ileal pouch-anal anastomosis, fulminant ulcerative colitis with two-stage operation, duration of diverting ileostomy after pouch formation, primary sclerosing cholangitis, other extraintestinal manifestations of ulcerative colitis, preoperative liver function tests, duration of ulcerative colitis, and the occurrence of postoperative complications. Initial univariate analysis was performed on all risk factors. Multivariate analysis was performed on all univariate risk factors with P values < 0.2.
Results
The prevalence of chronic pouchitis in our population was 46 percent. The following variables were identified during univariate analysis and entered into a multivariate model: preoperative serum albumin (P = 0.07), PSC (P = 0.126), duration of diverting ileostomy (P = 0.111), fulminant ulcerative colitis with two-stage operation, (P = 0.051), the presence of postoperative complications (P = 0.031), and the type of postoperative complications (anastomotic complications, P = 0.013). Patients who did not undergo diverting ileostomy at the time of their ileal pouch-anal anastomosis trended toward a lower likelihood of developing chronic pouchitis (P = 0.06). Multivariate analysis showed that patients with postoperative complications (53 percent, P = 0.042), specifically anastomotic complications, were more likely to develop chronic pouchitis (P = 0.005). Eight percent of patients had primary sclerosing cholangitis and 11 percent of patients had at least one extraintestinal manifestation of ulcerative colitis. Patients with primary sclerosing cholangitis were not more likely to develop chronic pouchitis (P = 0.168). Patients with extraintestinal manifestations also were not more likely to develop chronic pouchitis (P = 0.273).
Conclusions
Chronic pouchitis is a frequent complication after ileal pouch-anal anastomosis. In this study patients with primary sclerosing cholangitis or other extraintestinal manifestations of ulcerative colitis were not more likely to develop chronic pouchitis. Patients with postoperative complications, specifically anastomotic complications after ileal pouch-anal anastomosis, were more likely to develop chronic pouchitis and may benefit from early strategies to prevent pouchitis.





Similar content being viewed by others
References
Achkar JP, Al-Hadda M, Lashner B, et al. Differentiating risk factors for acute and chronic pouchitis. Clin Gastroenterol Hepatol 2005;3.
Aisenberg J, Shim WJ, Peen AE, et al. Perinuclear anti-neutrophil cytoplasmic antibody and refractory pouchitis. A case control study. Dig Dis Sci 1995;40:1866–72.
Hata K, Watanabe T, Shinozaki M, Nagawa H. Patients with extraintestinal manifestations have a higher risk of developing pouchitis in ulcerative colitis: multivariate analysis. Scand J Gastroenterol 2003;38:1055–8.
Fleshner PR, Vasiliauskas EA, Kam LY, et al. High level perinuclear cytoplasmic antibody (pANCA) in ulcerative colitis patients before colectomy predicts the development of chronic pouchitis after ileal pouch-anal anastomosis. Gut 2001;49:671–7.
Sandborn WJ, Landers CJ, Tremaine WJ, Targan SR. Antineutrophilic cytoplasmic antibody correlates with chronic pouchitis after ileal pouch-anal anastomosis. Am J Gastroenterol 1995;40:740–6.
Lohmuller JL, Pemberton JH, Dozosi RR, et al. Pouchitis and extraintestinal manifestations of inflammatory bowel disease after ileal pouch-anal anastomosis. Ann Surg 1990;5:622–9.
Yantiss RK, Sapp HL, Farraye FA, et al. Histologic predictors of pouchitis in patients with chronic ulcerative colitis. Am J Surg Pathol 2004;28:999–1006.
Merrrett MN, Mortensen N, Kettlewell M, Jewell DO. Smoking may prevent pouchitis in patients with restorative proctocolectomy for ulcerative colitis. Gut 1996;38:362–4.
Luukkonen P, Jarvinen H, Tanskanen M, Kahri A. Pouchitis-recurrence of the inflammatory bowel disease. Gut 1994;35:243–6.
Cheifetz A, Itzkowitz S. The diagnosis and treatment of pouchitis in inflammatory bowel disease. J Clin Gastroenterol 2004;38:S44–50.
Shen B, Achkar JP, Connor JT, et al. Modified pouchitis disease activity index: a simplified approach to the diagnosis of pouchitis. Dis Colon Rectum 2003;46:748–53.
Shen B, Lashner BA, Achkar JP, et al. Endoscopic and histologic evaluation together with symptom assessment are required to diagnose pouchitis. Gastroenterology 2001;121:261–7.
Levin KE, Pemberton JH, Phillips SF, et al. Role of oxygen free radicals in the etiology of pouchitis. Dis Colon Rectum 1992;35:452–6.
Tonelli F, Dolara P, Batignani G, et al. Effects of short chain fatty acids on mucosal proliferation and inflammation of ileal pouches in patients with ulcerative colitis and familial polyposis. Dis Colon Rectum 1995;38:974–8.
Mignon M, Stettler C, Phillips SF. Pouchitis: a poorly understood entity. Dis Colon Rectum 1995;38:100–3.
Ruseler-van Embden JG, Schouten WR, van Lieshout LM. Pouchitis: result of microbial imbalance? Gut 1994;35:658–64.
Shen B, Lashner BA, Achkar JP, et al. Irritable pouch syndrome: a new category of diagnosis for symptomatic patients with ileal pouch anal anastomosis. Am J Gastroenterol 2002;97:972–8.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hoda, K.M., Collins, J.F., Knigge, K.L. et al. Predictors of Pouchitis after Ileal Pouch-Anal Anastomosis: A Retrospective Review. Dis Colon Rectum 51, 554–560 (2008). https://doi.org/10.1007/s10350-008-9194-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10350-008-9194-7