Abstract
Background
Organ reconstruction is one of the most challenging tasks in plastic and reconstructive surgery. This is particularly true of ear reconstruction, which requires enormous attention to detail.
Methods
In the first of two articles, we set out details and precautions for each step of the preoperative and intraoperative stages of the ear reconstruction process for microtia patients. We cover preoperative screening and assessment of surgical conditions, the design of intraoperative incisions, flap separations, costal cartilage extraction, framework carving and cranial ear angle surgery.
Results
Over the period Jan 2015–July 2021, our surgical team carried out 1012 microtia ear reconstructions, at the rate of 3–4 per week. This article presents the key learnings from this high volume of operations. Two typical cases involving different types of microtia are presented in order to illustrate the process of total ear reconstruction.
Conclusions
This article describes in detail the preoperative and intraoperative stages of the ear reconstruction process. We share our cumulative surgical experience gained over 20 years, especially the latest practical lessons gleaned over the last six and a half years.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At present, autologous costal cartilage ear reconstruction is still the most commonly used method in external auricle reconstructive surgery. Since reports by Tanzer [1], Brent [2, 3], Nagata [4], Firmin [5] and others on microtia reconstruction methods, ear reconstructive surgery has seen further improvements and become more mature. This is good news for patients. However, for young doctors learning ear reconstruction surgery, there is an urgent need for a complete set of reference methods. Most ear reconstruction articles published in recent years focus on the improvement of some aspect of operative methods. We adopt a more comprehensive approach based on our own experience. In this first article, we describe in detail the preoperative and intraoperative methods and procedures used in recent years. A follow-up article looks at postoperative methods and procedures. Together the two articles provide an up-to-date overview of the entire ear reconstruction process, for which there is no equivalent in the literature. The methods we present are safe, stable and mature, and relatively easy for young doctors to learn and implement.
Materials and Methods
Preoperation
Indications
All ear reconstruction patients must be at least 6 years old and have a chest circumference of more than 60 cm below the xiphoid process. Begin by checking whether the skin flap in the operating area has a history of trauma or scars and whether the fascia has been damaged, because these factors will affect blood supply to the flap. Before the operation, shave an area three fingers wide around the ear. Check and confirm that there is no local inflammation such as folliculitis in the operating area.
Ear Mold Film Production
Use transparency film to make ear molds according to the preoperation normal ear contour. For patients with bilateral microtia, base the ear molds on the auricles of their parents. Draw the structure of the external helix, antihelix, upper and lower feet of the antihelix, earlobe, tragus, antitragus and the notch between the earlobes. Make two copies: one for disinfection during intraoperation and one for preoperative design of the affected side.
Intraoperation
Reconstructive Ear Positioning Design
The long axis of the reconstructive ear is parallel to the axis of the back of the nose. Measure the distances from the upper ridge point of the external helix to the outer edge of the outer canthus and from the lower edge of the earlobe of the normal ear to the nasal alar. Use the margin points to determine the upper ridge point of the external helix and the lower edge point of the earlobe of the affected ear. Determine the separation range of the mastoid flap and the transposition position of the earlobe flap according to the contour of the ear mold. For microtia patients with hemifacial microsomia, achieving balance and harmony between the bilateral auricles and the face is more important than absolute positional symmetry. The distances from the upper ridge point of the external helix to the outer edge of the outer canthus and from the lower edge of the earlobe of the normal ear to the nasal alar should be shorter than the measurements taken on the normal side. The positioning design method described above is therefore not suitable for those patients. Adjust it to ensure visual harmony.
Earlobe Transposition
Trace a symmetrical “W”-shaped incision on the back of the residual earlobe and the skin of the mastoid area. Transpose the upper earlobe flap to the mastoid area and connect it to its base, so that it plays an active role in the embedding of the ear cartilage framework. There are four different earlobe design strategies. In a previous article [6], we gave a detailed description of the four strategies for reconstructing the earlobe from the remnant ear.
Skin Flap Separation
Inject 1:200,000 epinephrine saline into the subcutaneous layer along the incision to reduce bleeding and ensure uniform thickness of the separated skin flap. Make the incision and separate the flap in the subcutaneous layer. The flap in this area is thin, so a superficial layer of fat should be reserved on the flap to ensure good blood supply. Reserve a subcutaneous pedicle with a diameter of about 1 cm at the intertragic notch to facilitate the blood supply. Experience has taught us that the subcutaneous pedicle should be as wide as possible—provided it does not affect the rotation of the ear cartilage framework—to ensure the blood supply at the distal end of the flap. Remove the original remnant ear cartilage close to the cartilage surface and preserve the skin. Insert the ear cartilage framework and trim the redundant skin. Considering the height of the ear framework and the need for rotation, the flap separation should exceed the edge of the external ear by 2 cm. After the ear framework is rotated into position, place the costal cartilage part of the earlobe behind the earlobe to ensure the fullness of the transposed earlobe and the complete connection effect of the whole ear.
Rib Cartilage Acquisition
Locate the 6th, 7th and 8th costal cartilage; then, design an incision that can expose the upper pole to the 6th/7th costal cartilage joint and the lower pole to the soft and hard junction of the 8th rib, taking skin elasticity into account. Since the perichondrium is weak and the cartilage is soft, carefully control the force used when cutting the perichondrium to avoid damaging the costal cartilage. Use a small periosteum stripper to separate the periosteum along the cut perichondrium. There is usually a latent space between the periosteum and the cartilage, so it can be easily peeled off. However, in a small number of patients, the perichondrium and cartilage space are dense, and the use of the periosteum stripper may cause cartilage damage. Proceed carefully. When peeling to the edge of the costal cartilage, turn the periosteum stripper to the underside of the cartilage to leave the perichondrium in the body. The lower edge of the costal cartilage is loosely combined with the perichondrium and is easily removed, but the upper edge often forms a dense combination with intercostal muscles, making it difficult to peel off. When peeling the periosteum at the back of the cartilage, be careful to keep the perichondrium intact, so as to reduce the incidence of thoracic deformities. Keep the periosteum stripper horizontal to avoid puncturing the pleura and causing pneumothorax. Careful manipulation of the periosteum stripper is a key factor in avoiding pneumothorax.
Cut off about 2cm of the 6th/7th costal cartilage joint as well as the hard and soft junction of the sixth, seventh and eighth costal cartilage. When cutting the soft and hard junction, stay as close to the hard bone as possible so that the cartilage is as long as possible. By contrast, the resection of joint 6 and 7 should be as close as possible to preserve the joint cartilage to avoid thoracic deformity. If the left thorax is close to the heart, take more care. After removing the costal cartilage, suture the complete perichondrium to close it. When it is clear that there is no bleeding and pneumothorax, inject 1:1 ropivacaine into the lower edge of the intercostal space to relieve postoperative chest pain. The perichondrium, muscle layer, subcutaneous tissue layer and skin layer can then be sutured in sequence. Place a drainage tube in the muscular layer, suctioned by negative pressure.
Framework Carving
Bottom Plate: Draw the shape of the external auricle on the 6th and 7th costal cartilage and their joints according to the ear mold film and carve them to be the bottom plate of the ear framework.
External Helix: Separate the 8th costal cartilage into two parts longitudinally. Do not reduce the height of the external helix, but it can be bent naturally to form an arc. The outer side serves as the external helix. The shape of the complete external helix from the helix foot to the intersection of the helix tail and the earlobe should be thick, high and wide, gradually becoming narrower and lower in height. The highest point of the outer helix curvature should be the upper ridge of the external helix, and the bottom of the helix foot should connect to the bottom plate joint. The optimal anatomical length of the external helix is about 8.5–10cm. If the floating ribs are not long enough, our practice is to sacrifice part of the helix feet to ensure that the external helix is completely connected with the transposition earlobe. The prominent spiral structure is a crucial part of sculpting the final ear contour. The success of spiral engraving largely depends on the utilization of the complex properties of the original cartilage. A previous report [7] looked at the spiral shape of the eighth costal cartilage and its properties and the corresponding differences in surgical methods for the external auricle.
Antihelix: The remaining part of the inner side is used as a complete structure to engrave the "Y" shape to make the antihelix and its upper and lower feet. Its height is about 3~5mm. The antihelix, the lower foot and the upper foot decrease in sequence. According to our many years of experience in postoperative follow-up of patients [8], a natural antihelix structure is best achieved not by chiseling a sharp "Y"-shaped cartilage graft to highlight the structure, but by widening the upper and lower feet of the antihelix and transitioning with a gentle slope. The width of the lower foot of the antihelix is limited to about one-third of the upper foot and the lower foot maintains high relief. In this way, the harmonious structure of the helix and its upper and lower feet correspond to the external helix, which enhances the overall three-dimensional beauty of the external auricle without becoming unnatural.
Tragus, antitragus and intertragic notch: Select the remaining part of the 6th and 7th costal cartilage and engrave a "V" shape. The tragus and the antitragus are at the same height and the same level as the tail of the helix. The height of the intertragic notch is slightly lower. After finishing the ear framework, add 1 or 2 pieces of 5 mm high remaining cubic cartilage under the bottom plate to increase the thickness of the bottom plate and deepen the concha cavity. The success of ear framework carving depends largely on the appropriate utilization of cartilage, generally various sizes of residual cartilage. In the previous study [9], we discuss in detail tragus carving and the antitragus complex under different cartilage residue conditions.
Excess cartilage: The excess costal cartilage block is buried under the chest skin for use in stage II cranial ear angle reconstruction.
Stage II Cranioauricular Angle Reconstruction
Cranioauricular angle reconstruction is performed 6 months after the first-stage operation. Cut the 2~3 mm outside the external helix of the ear framework and turn over the ear framework along the thin tissue layer. For the framework coverage in stage II, we recommend choosing the modified retroauricular fascia [10, 11]. Separate the skin and the retroauricular fascia below the subcutaneous fat layer. The fascia dissection range is 2.5 to 3.0 cm from the outer edge of the external helix, slightly longer than the longitudinal axis of the auricle. Turn the fascia up to the ear side. The combination of the posterior fascia and the subfascial tissue is relatively loose. The area of the fascia should completely cover the cartilage framework behind the ear. Carefully turn the posterior fascia along the longitudinal axis that contains the main posterior auricular artery.
Take out the costal cartilage block buried under the chest skin in the first stage and trim the edges to remove sharp points. Position it at the cranioauricular groove to reach the angle same as the contralateral side fixed using steel wire. If there is not enough stage I cartilage, a hydroxyapatite support or titanium mesh strut can be used [12]. Fold the retroauricular fascia forward, covering it with 5/0 absorbable sutures. Fix the outer edge of the fascia to the subcutaneous tissue. Push the skin flap behind the ear forward and fix it in place by suturing under the skin.
Select the ipsilateral scalp skin on the fascia [13], and pack and fix it to avoid any space under the skin. After 10 days, remove the skin graft pressurized gauzes and the sutures. The patient should wear an external cranioauricular groove mold for 3 to 6 months to maintain a good cranioauricular angle.
Case Reports
Case 1
A 28-year-old male patient presented with lobule type microtia (Fig. 1). The design of intraoperative incisions, flap separations, costal cartilage extraction, framework carving and cranial ear angle surgery followed the procedures described above. The first stage postoperative view after 6 months showed that a satisfactory result was achieved, with all the essential morphologic structures of the auricle well defined. The auricle appeared smooth and natural. The second stage was performed and the bilateral cranioauricular angles were observed to be symmetrical at a follow-up visit.
A 28-year-old male patient presented with lobule type microtia. A, B Preoperative anterior and lateral view. C Intraoperative sculpted cartilage framework. D Intraoperative auricular appearance immediately after implanting the ear framework. E, F Preoperative anterior and lateral view before the second stage. G, H Postoperative anterior and lateral view after the second stage
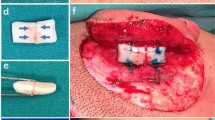
Case 2
A 12-year-old boy presented with concha type microtia (Fig. 2). The earlobe incision preserved the lower half of the earlobe with no need to rotate. The tragus and intertragic notch structures of the cartilage framework did not have to be reconstructed because they naturally existed. The first-stage postoperative view after 6 months confirmed a satisfactory result, with all the essential morphologic structures of the auricle well defined. The auricle appeared smooth and natural. On a follow-up visit, the second-stage surgery was performed and bilateral cranioauricular angles were made symmetrical
A 12-year-old boy presented with concha type microtia. A, B Preoperative anterior and lateral view. C Intraoperative sculpted cartilage framework. D Intraoperative auricular appearance immediately after implanting the ear framework. E, F Preoperative anterior and lateral view before the second stage. G, H Postoperative anterior and lateral view after the second stage
Discussion
The characteristics of a normal external ear structure include size, orientation and three-dimensional positioning on the head and face. The final anatomical landmarks must be fully reflected in the ear shape so that the reconstructed ear is accepted. Balance between the shape and position of the residual ear and the anatomy of the ear framework and flap is the key factor in obtaining satisfactory remodeling of the auricle. The set of techniques and detailed attention points we share from our preoperative to postoperative experience in this and the follow-up article make it possible to construct delicate, beautiful, matching ears.
Skin quality differs from one ethnic group to another. In general, Caucasians have thinner, more elastic skin that is more resistant to shrinkage than the thicker, less elastic skin of Asians and therefore has a lower risk of blood supply damage. Our experience with Asian patients has shown us that the pedicle must be preserved when the flaps are separated.
Be gentle and careful when acquiring rib cartilage. In our 20-year surgical experience of more than 4000 ear reconstructions, only 3 cases of pneumothorax have occurred. The key is to define the proper space when separating the perichondrium, especially at the back of the cartilage. Keep the stripper horizontal, so as not to puncture the pleura and cause pneumothorax. When separating the perichondrium, careless operation of the stripper can lead to pneumothorax. If pneumothorax occurs, not all cases require closed chest drainage. In our experience, it is often sufficient to simply insert a urinary catheter into the gap, suck out the gas or liquid using a syringe and then suture the gap.
The technique for carving the auricular cartilage framework focuses on its three-dimensional prominent structures: external helix, antihelix, tragus and antitragus, allowing the concave structures to emerge naturally. Ideally, the external helix will be sufficiently long and wide; the antihelix should have a broadened upper foot and gentle slope to avoid a sharp “Y” shape; the tragus and antitragus should be stable with a prominent morphology. If the costal cartilage is calcified and hardened, in particular if the eighth costal cartilage is difficult to cut or bend, then it can easily break or become angled. We therefore use the outer edge of the framework bottom plate as the external helix. Since the helix has a notch at the junction of the 6/7 joint, we suggest wrapping it with a small piece of fascia to eliminate this notch. This maintains the natural curvature and transition of the framework. The edges of each protruding anatomical structure of the cartilage framework must be rounded and smooth to avoid excessive pressure and necrosis of the covered skin. The contour of the reconstructed ear after surgery should not be too sharp. Otherwise, when the skin contracts, the contours will become too obvious, and the gentle transition between the various structures will be lost.
We believe that steel wire is more reliable than nylon sutures to resist tension in different directions. Therefore, we recommend the use of steel wire to fix the ear cartilage support and stage II posterior cartilage support. A steel wire of a suitable size determines the stability and self-exposure rate of the frame. We found that a steel wire with a diameter of about 0.20 mm is strong enough to maintain the integrity of the frame. During follow-up, most cases of exposed wire occurred with wires that had a diameter of approximately 0.25 mm. Even in these cases, the exposed steel wire can be easily removed and does not affect the shape of the external auricle.
For microtia patients with normal anatomy of the posterior auricular artery, we recommend using the posterior fascia to cover the posterior auricular support framework during cranioplasty. There are several advantages to choosing this modified fascial flap: It is near the superficial temporal fascia, it contains 2 to 3 branches of the posterior auricular artery in the mastoid area and does not affect the blood supply; furthermore, it is easy to dissect during the operation. More importantly, in cranioplasty, the turnover and use of the posterior fascia will not affect the blood supply of the superficial temporal fascia, and the superficial temporal fascia tissue can be fully preserved. The posterior fascia is used as the coating material. In the case of accidents such as exposure of the framework or ear trauma after the second stage, the superficial temporal fascia can also be used as a material for re-ear repair, cartilage or framework coating.
To determine the most suitable donor area for the stage II operation, a previous study [13] compared the contralateral postauricular, groin and scalp as potential donor areas in terms of color matching, flatness, depth of sulcus and symmetry of angle. Each skin graft donor site has advantages and disadvantages; we chose the scalp. The principal advantage of the scalp site is esthetic: It causes no new surgical scar, a benefit of particular interest to growing children.
Conclusions
This article describes the preoperative and intraoperative stages of the ear reconstruction process. A second article deals with the postoperative stage. The aim of the two articles is to help doctors master ear reconstruction methods more easily, conveniently and comprehensively.
References
Tanzer RC (1959) Total reconstruction of the external ear. Plast Reconstr Surg 23:1–15
Brent B (1980) The correction of microtia with autogenous cartilage grafts: II. Atypical and complex deformities. Plast Reconstr Surg 66(1):13–21
Brent B (1980) The correction of microtia with autogenous cartilage grafts: I. The classic deformity. Plast Reconstr Surg 66(1):1–12
Nagata S (1993) A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg 92:187–201
Firmin F (1998) Ear reconstruction in cases of typical microtia. Personal experience based on 352 microtic ear corrections. Scand J Plast Reconstr Surg Hand Surg. 32:35–47
Xu Z, Zhang R, Zhang Q, Xu F, Li D, Li Y (2018) New strategies for remnant ear treatment in lobule-type microtia reconstruction. Plast Reconstr Surg 142(2):471–479
Xu Z, Xu F, Zhang R, Zhang Q, Li D, Li Y (2017) A new classification of helix fabrication methods with autogenous costal cartilage in microtia reconstruction. Plast Reconstr Surg 139(6):1315e–1324e
Li D, Zhang R, Zhang Q et al (2014) A novel method of naturally contouring the reconstructed ear: modified antihelix complex affixed to grooved base frame. Plast Reconstr Surg 133(5):1168–1174
Xu Z, Zhang R, Zhang Q, Xu F, Li D, Li Y (2019) New strategies for tragus and antitragus complex fabrication in lobule-type microtia reconstruction. Plast Reconstr Surg 144(4):913–921
Li Y, Zhang R, Zhang Q, Xu Z, Xu F, Li D (2017) An alternative posterosuperior auricular fascia flap for ear elevation during microtia reconstruction. Aesthet Plast Surg 41(1):47–55
Li Y, Cui C, Zhang R et al (2018) Anatomical and histological evaluation of the retroauricular fascia flap for staged auricular reconstruction. Aesthet Plast Surg 42(3):625–632
Li DT, Zhang RH, Zhang Q, Xu F, Xu ZC, Tang XJ (2012) Titanium mesh strut: a novel instrument for firm elevation of the reconstructed auricle. Aesthet Plast Surg 36(3):746–749
Li D, Zhang R, Zhang Q et al (2020) Clinical results of ear elevations in patients with microtia using skin grafts from three donor sites: a retrospective study. Aesthet Plast Surg 44(5):1545–1552
Funding
This work was supported by grants from the National Natural Science Foundation of China (NO. 81974291) and Fundamental research program funding of Ninth People's Hospital affiliated to Shanghai Jiao Tong university School of Medicine (JYZZ143).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent has been signed by patient or guardian.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, X., Zhang, R., Zhang, Q. et al. Microtia Part I: Preoperation and In-operation Lessons from 1012 Ear Reconstruction Operations. Aesth Plast Surg 46, 2781–2787 (2022). https://doi.org/10.1007/s00266-022-02818-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02818-6