Abstract
Purpose
This retrospective cohort study aimed to evaluate the efficacy and safety of percutaneous endoscopic lumbar decompression (PELD) in elderly patients with lumbar spinal stenosis (LSS).
Study Design
A matched retrospective study.
Setting
The research was conducted in Beijing Chaoyang Hospital, Capital Medical University, China.
Methods
This study included patients treated with PELD for LSS from September 2016 to September 2020. Patients with LSS aged ≥ 80 years were screened according to the inclusion and exclusion criteria as the study group, and then the same number of patients with LSS aged 50–80 years were matched according to gender, stenosis type, and surgical segment as the control group. Preoperative patient status was assessed using the Charlson comorbidity index (CCI) and the American Society of Anesthesiologists (ASA) physical status classification score. Clinical outcomes were assessed using the visual analog scale (VAS), Oswestry Disability Index (ODI) scores, modified Macnab criteria, radiological parameters and complication rates.
Results
A total of 624 LSS patients met the screening criteria between September 2016 and September 2020, with 47 LSS patients ≥ 80 years old serving as the study group. Forty-seven LSS patients aged 50–80 years were matched to the study group according to gender, stenosis type, and stenosis segment. The CCI score (1.77 ± 1.67) and ASA classification (2.62 ± 0.74) of the study group were significantly higher than the CCI score (0.66 ± 0.96) and ASA classification (1.28 ± 0.54) of the control group, and the difference was statistically significant. Compared with preoperative data, postoperative ODI, leg pain VAS scores and back pain VAS scores were significantly improved in both groups (p < 0.05). However, no significant difference was found between two groups in preoperative and postoperative ODI, leg pain VAS scores and back pain VAS scores (p > 0.05). The operation time and postoperative hospital stay in control group were significantly lower than those in study (p < 0.05), but there was no significant difference in blood loss between the two groups (p > 0.05). Besides, overall radiological parameters were comparable in elder and younger patients (p > 0.05), and disc height (DH), lumbar lordosis and segmental lordosis decreased after two year follow-up in both groups (p < 0.05). In addition, complication rates were similar between the two groups (p > 0.05), and no serious complications and deaths were found.
Limitations
Single-centre retrospective design, non-randomized sample, small sample size.
Conclusion
Although elderly LSS patients (≥ 80 years old) are less fit and have more comorbidities, satisfactory outcomes can be achieved with PELD, comparable to those of LSS patients < 80 years old, and without increased complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Population aging is the inevitable result of population transformation, and it is an important issue facing human society in the twenty-first century. With the development of technology, people over the age of 80 are the fastest growing age group worldwide, which leads to an increase in the incidence of age-related diseases. Lumbar spinal stenosis (LSS) is a common age-related degenerative disease [1]. In the national low back pain study, 22% of patients with chronic low back pain were ultimately diagnosed with LSS [2]. LSS can cause moderate to severe pain that affects the quality of life of patients [3]. Elderly patients with LSS usually suffer from long-term pain and underlying diseases, and conservative treatment results are poor [4]. Patients with LSS who fail conservative treatment often require surgery.
Open decompression (OD) has been considered the gold standard surgical option for LSS [5]. OD can relieve nerve damage and improve associated pain by relieving lumbar spinal stenosis and removing excess tissue [6]. However, due to the disadvantages of OD, such as large trauma, long operation time, high blood loss, and increasing the incidence of complications in elderly patients, most elderly LSS patients cannot achieve satisfactory results after OD treatment [7,8,9]. Therefore, it is still necessary to explore new surgical solutions for elderly LSS patients with many comorbidities. With the improvement of surgical techniques, optical equipment and surgical instruments, minimally invasive techniques for the spine have developed rapidly. The percutaneous endoscopic lumbar decompression (PELD) method has become a popular minimally invasive technique for the treatment of lumbar degenerative diseases [10, 11]. According to studies, PELD has the advantages of less tissue trauma and shorter operation time than OD [12, 13]. Additionally, studies have found that PELD and OD have similar efficacy in the treatment of LSS, but less complications and mortality than OD [14]. PELD has emerged as an important alternative treatment for LSS. However, no relevant studies have reported the efficacy and safety of PELD in the treatment of elderly LSS patients (especially those with multiple comorbidities and poor physical conditions). Therefore, we designed a gender, stenosis type and surgical segment-matched retrospective study to investigate the clinical outcomes of elderly LSS patients (≥ 80 years) treated with PELD in order to provide clinical guidance for surgeons in the treatment of elderly LSS patients.
Patients and methods
Patients
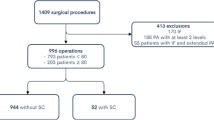
A retrospective analysis was performed on patients with LSS who received PELD from September 2016 to September 2020. The inclusion criteria for this study were: 1. Patients aged ≥ 50 years; 2. Clinically diagnosed with symptomatic LSS and ineffective conservative treatment for three months; 3. Patients receiving PELD therapy. Patients with cervical and thoracic spinal diseases; history of previous spinal surgery; spinal deformity, spondylolisthesis and lumbar instability; combined lumbar infection and tumour; and patients with incomplete data or lost to follow-up were excluded. During this period, a total of 624 patients with LSS underwent PELD surgery, including 47 patients with LSS ≥ 80 years as the study group. Then, 47 LSS patients aged 50–80 years who matched the study group in terms of gender, stenosis type, and stenosis segment were selected as the control group. All patients were followed up for two years after surgery. This study was approved by the ethics committee, and all patients signed informed consent.
Surgical technique
PELD procedures were all performed by a senior spine surgeon (ZL) with sufficient experience, at a single level, under local anaesthesia, with the patient placed in a prone position. The patient can communicate with the surgeon during the entire operation to prevent intraoperative nerve root injury. For patients with multilevel stenosis, to determine the level most responsible to symptoms, best suiting for the procedure, a transforaminal selective nerve root block was performed.
The entry point was set at 12 to 14 cm lateral to spinal middle line at the index intervertebral level. Then puncture needle was inserted into the superior articular process (SAP) of the targeted segment. Through the puncture needle, serial cannulated dilators were inserted into the SAP. The ligamentum flavum and the ventral elements on the SAP were removed. Then, a tubular retractor with an outer diameter of 7.9 mm was passed over the dilators and secured to the upper lamina and burrs were used to further enlarge the foramen if necessary. The herniated disc, parts of posterior longitudinal ligament, posterior upper margin of the inferior vertebral body, posterior lower margin of the superior vertebral body (if necessary) and the dorsal ligamentum flavum were removed with rongeur, endoscopic forceps, endoscopic bone knife or a highspeed drill. Finally, the entire nerve root and dural sac was probed to ensure complete decompression. Adequate irrigation and haemostasis were performed to reduce postoperative infection and hematoma.
Clinical evaluation
Demographic data of all study participants were collected, including gender, age, Obesity (BMI ≥ 28), smoking, length of postoperative hospital stays, lesion segment, operative time, blood loss, stenosis type, Charlson comorbidity index (CCI) [15], the American Society of Anesthesiologists (ASA) physical status classification score [16]. The visual analog scale (VAS) was used to assess leg pain and low back pain. The Oswestry Disability Index (ODI) was used to assess clinical functional status. The surgical satisfaction was assessed using the modified Macnab criteria. In addition, postoperative complications were also assessed in this study.
Radiological evaluation
Disc degeneration status were identified by disc height (DH) and the Pfirrmann grade of disc. DH was measured as the mean distance of the anterior and posterior disc heights on mid-sagittal MRI T2-weighted sequence. The Pfirrmann grading system ranging from I to V was also used in assessing disc degeneration [17]. Lumbar lordosis was measured as the angle between superior endplate of L1 and the superior endplate of S1, and segmental lordosis was measured as the angle between the inferior endplate of the superior vertebrae and the superior endplate of the inferior vertebrae at the index level by lateral radiographs. Newly developed disc herniation, lumber stenosis, spondylolisthesis, and lumbar instability were detected by the comparison of the final follow-up and preoperative MRI, lateral radiographs, or flexion–extension radiographs.
Statistical analysis
Data analysis was performed with GraphPad Prism 8 (GraphPad Software, San Diego, CA). Data are presented as mean ± standard deviation (SD). Data comparisons between preoperative and postoperative time points were analyzed using paired samples t-tests or McNemar-Bowker tests. Comparisons between the two groups were assessed using an independent samples t-test. The chi-square test was used to compare discontinuous variables between the two groups. The p < 0.05 indicated that the difference was statistically significant.
Results
A total of 624 LSS patients met the screening criteria between September 2016 and September 2020, with 47 LSS patients ≥ 80 years old serving as the study group. Forty-seven LSS patients aged 50–80 years were matched to the study group according to gender, stenosis type, and stenosis segment.
Those patient baseline characteristics were shown in Table 1. The mean age of patients in study and control group was 83.26 ± 2.53 and 64.55 ± 8.32 years, respectively. The most common lumbar spine level in study and control group was L4-5 (study group: n = 36, control group: n = 36), followed by L5-S1 (study group: n = 6, control group: n = 6) and L3-4 (study group: n = 5, control group: n = 5). All patients in study group had comorbidities, including hypertension, diabetes mellitus, cardiovascular diseases, cerebrovascular disease, pulmonary disease, liver / gastrointestinal diseases, renal insufficiency, history of anticoagulants or antiaggregants use, osteoporosis and cancer history (Table 2). In control group, 29 patients (61.7%) had comorbidities. The incidence of comorbidities was significantly different between the two groups (P < 0.05). The mean CCI score and ASA classification in study group were 1.77 ± 1.67 and 2.62 ± 0.74, respectively; while the mean CCI score and ASA classification in control group were 0.66 ± 0.96 and 1.28 ± 0.54, respectively. There were statistically significant differences in CCI score and ASA classification between the two groups (p < 0.05). The operative time and postoperative hospital stays of the control group were significantly lower than those of the study group (p < 0.05). In addition, there was no significant difference in blood loss between the two groups (p > 0.05).
There were no major complications or procedure-related deaths in either group. Eight patients in study group had general complications including cardiovascular disease, pulmonary disease, liver/gastrointestinal disease, renal insufficiency, urinary tract infection and deep venous thrombosis; four patients in control group had general complications, and there was no statistical difference between the two groups (p > 0.05, Table 3). In addition, surgical complications occurred in 11 patients (7 patients (14.9%) in study group, four patients (8.5%) in control group, p > 0.05, Table 3). Six patients from both groups underwent reoperation for different reasons: incomplete decompression (2 patients), contralateral symptoms after decompression (1 patient) and recurrent disc herniation (3 patients).
Compared with preoperative data, both groups showed significant improvements in ODI, leg pain VAS scores and back pain VAS scores at three months, one year and two years postoperatively (p < 0.05, Fig. 1). ODI, leg pain VAS scores and back pain VAS scores in study group decreased from preoperative 67.94 ± 5.57, 6.17 ± 1.03 and 6.15 ± 0.86 to two years postoperative 21.17 ± 4.33, 2.26 ± 1.01 and 2.3 ± 1.16, respectively. In control group, ODI, leg pain VAS scores and back pain VAS scores were significantly decreased from preoperative 69.51 ± 5.83, 5.98 ± 1.01 and 6.04 ± 0.83 to postoperative 20.55 ± 4.89, 2.11 ± 0.91 and 2.17 ± 0.99, respectively. No significant differences were found in ODI, leg pain VAS score and back pain VAS score between the two groups in the preoperative, three month, one year and two year postoperative periods (p > 0.05, Fig. 1).
According to the modified MacNab criteria, 39 patients (83%) in study group had a good-to-excellent outcome and 42 patients (89.4%) in control group had a good-to-excellent outcome, with no statistical difference between the two groups (p > 0.05, Fig. 2). Representative case is presented in Fig. 3.
Percutaneous endoscopic lumbar decompression performed on a 81-year-old female patient diagnosed with L5/S1 left lateral recess stenosis. A1, preoperative CT on sagittal scans. A2, preoperative CT on axial scans. B1, postoperative CT on sagittal scans. B2, postoperative CT on axial scans. C1, preoperative MRI on sagittal scans. C2, preoperative MRI on axial scans. D1, postoperative MRI on sagittal scans. D2, postoperative MRI on axial scans
Radiological parameters were further evaluated (Table 4). Compared to preoperative disc degeneration status, DH at final follow-up decreased significantly (study group: [7.6 ± 2.3] mm vs. [7.9 ± 2.2] mm, P < 0.01; control group: [8.2 ± 1.6] mm vs. [8.5 ± 1.6] mm, P < 0.01). Although more patients suffered from Pfirrmann grading ≥ IV at the index disc in study group compared with control group, no significant differences were identified in the two groups between preoperative and final follow-up data. Both lumbar lordosis and segmental lordosis were significantly decreased at final follow-up in the study and control group, yet there was no difference between the two groups. There were five patients (3 in study group and 2 in control group) suffered from newly developed disc herniation, and four patients (2 in study group and 2 in control group) suffered from newly developed lumbar stenosis. Furthermore, four patients developed spondylolisthesis (1 in study group and 3 in control group), and one patient in study group developed lumbar instability postoperatively. None of disc herniation, lumbar stenosis, spondylolisthesis, and lumbar instability significantly differed between the two groups.
Discussion
Few studies have reported the efficacy and safety of PELD in the treatment of elderly LSS. Therefore, this study is the first to compare the efficacy and safety of PELD in treating LSS patients ≥ 80 years old and < 80 years old. Our results showed that LSS patients aged ≥ 80 years can achieve satisfactory efficacy after PELD treatment, which is comparable to that of LSS patients aged < 80 years without increased complications.
OD is considered the gold standard for surgical treatment of LSS in patients with LSS who are refractory to conservative treatment or in severe disease [18]. Many studies have demonstrated that OD is effective in the treatment of LSS [19, 20]. However, laminectomy due to OD may affect the stability of the spine, resulting in varying degrees of injury and complications [21]. In addition, because elderly LSS patients are often accompanied by poor physical conditions and many comorbidities, the large trauma and blood loss of OD surgery will be detrimental to the recovery of elderly LSS patients [22, 23]. With the development of technology and concepts, PELD has become a treatment for degenerative diseases of the lumbar spine and has been shown to be effective for LSS [24, 25]. PELD is becoming more and more popular in LSS due to the advantages of short operative time, low surgical risk, minimal impact on spinal stability, quick postoperative recovery, and fewer complications [26, 27]. Lv et al. compared the outcomes of PELD versus fenestration for the treatment of external lumbar indentation stenosis in elderly patients over 75 years of age [14]. They found that both PELD and fenestration showed good clinical outcomes for the treatment of lumbar scoliotic stenosis, with fewer complications from PELD. A retrospective study showed that the clinical outcomes of PELD for external pit stenosis were excellent, with an improvement in the VAS total score from 7.9 ± 1.2 to 2.3 ± 1.0 and an ODI decrease from 69.1 ± 7.3 to 24.7 ± 6.4 [28]. However, there are few studies on the efficacy and safety of PELD in the treatment of elderly LSS. Only one study reported the efficacy of PELD in patients over 75 years of age. They found that PELD was safe and effective for LSS treatment in elderly patients, with significantly lower postoperative VAS scores for both low back and leg pain compared to preoperatively [25]. Similar to their results, our study also found that PELD has good clinical efficacy in elderly LSS patients (≥ 80 years). Patients with LSS ≥ 80 years had significantly improved postoperative ODI, leg pain VAS scores, and back pain VAS scores after PELD treatment compared with preoperative data. According to Macnab criteria, 39 patients (83%) had a good-to-excellent outcome. Moreover, Li et al. also showed that elderly LSS patients can achieve the same satisfactory outcomes as younger patients after PELD treatment [25], which is similar to the results of our study. Our results also show that LSS patients ≥ 80 years old can achieve the same curative effect as patients < 80 years old after PELD treatment, and there is no significant difference in complications between the two groups, indicating that PELD treatment of LSS patients ≥ 80 years old is safe and effective.
Patients ≥ 80 years old had more comorbidities, and the ASA grade and CCI index were higher than younger patients. It has been reported that higher CCI and ASA scores are associated with higher likelihood of complications [29]. Studies have demonstrated that the risk of postoperative severe complication is independently associated with heart disease and anticoagulant use [30, 31]. A nationwide population-based study showed that after LSS surgery, patients with diabetes were approximately 1.35 times more likely to die than those without diabetes [32]. In our study, all patients in study (≥ 80 years) had comorbidities, and the CCI and ASA scores were higher than those in control group (< 80 years), the difference was statistically significant. However, elderly LSS patients in study could achieve similar efficacy to control group after PELD treatment, and there was no significant increase in complications. These results suggest that PELD can be safely treated in elderly patients with multiple comorbidities without increasing complications.
Complication rate is an important factor in evaluating the safety of surgery. Studies have reported complication rates of 6 to 52% for all LSS decompression procedures and 10 to 20% for patients ≥ 80 years [20, 33]. Previous studies have shown that patients aged ≥ 85 years had more postoperative complications after decompression surgery than other age groups [33, 34]. In our study, we found that the complications of PELD in the treatment of LSS patients ≥ 80 years old are rare, the incidence of general complications is 17.0%, and that of surgery-related complications is 14.9%. Moreover, we also found that there was no significant difference in the risk of complications between patients ≥ 80 years old and patients < 80 years old. In our study, for general complications, we keep close contact with physicians and actively treat related complications. For the surgery-related complications, different types adopt different ways to deal with them. Haematoma is a rare complication of spinal surgery and should be detected promptly and surgically removed as soon as possible. In our study, one patient developed a haematoma, numbness and weakness of the lower extremities and decreased muscle strength after PELD. Surgery was performed urgently to remove the haematoma and after that the symptoms of nerve root compression were relived. To reduce the risk of postoperative bleeding and hematoma formation, we usually decrease the irrigation water pressure to detect and haemostasis potential bleeding before the end of the operation. Dural tear is a common complication associated with surgery. In this study, there were four patients with dural tears, all of which occurred at the nerve root sleeve and were caused by the severe adhesion. They were treated conservatively by abdominal compression bandaged bed rest for one week, no cerebrospinal fluid leakage and wound infection. For patients who need re-surgery, PELD can be used again for revision surgery.
Few studies have evaluated the morphometric effects after PELD. Li et al. found no significant difference of DH, lumbar lordosis and segmental lordosis after PELD during a at least one year follow-up compared to those preoperatively [35]. However, the follow-up period of the study was relatively shorter. In our study, we found all of DH, lumbar lordosis and segmental lordosis were decreased after PELD with a at least two year follow-up. However, no statistical differences were identified between elder and younger patients. We believe this may attribute to the natural degeneration of patients instead of the influence of surgical intervention, and PELD can achieve sufficient morphometric effect in both elder and younger patients with LSS.
There are some limitations in this study. First, this study is a single-centre, small sample size retrospective study and has a short follow-up period. Second, although the two matched groups of individuals had the same gender, stenosis type, and surgical segment, some variables such as the degree of spinal canal and foraminal stenosis could not be controlled, which may have influenced the results. Finally, this study did not evaluate the clinical outcomes of PELD versus OD in the treatment of elderly LSS patients. Therefore, additional studies with larger sample sizes are needed for supplementation and validation.
Conclusion
This study demonstrated that PELD is effective and safe for LSS patients aged ≥ 80 years. In addition, this study also found that PELD has similar benefits and risks in LSS patients over and under 80 years of age. Our results may provide a good treatment option for surgeons treating elderly LSS patients (≥ 80 years) with comorbidities.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Lurie J, Tomkins-Lane C (2016) Management of lumbar spinal stenosis. Bmj 352:h6234. https://doi.org/10.1136/bmj.h6234
Long DM, BenDebba M, Torgerson WS et al (1996) Persistent back pain and sciatica in the United States: patient characteristics. J Spinal Disord 9(1):40–58
Hadianfard MJ, Aminlari A, Daneshian A et al (2016) Effect of Acupuncture on Pain and Quality of Life in Patients with Lumbar Spinal Stenosis: A Case Series Study. J Acupunct Meridian Stud 9(4):178–182. https://doi.org/10.1016/j.jams.2015.11.032
Minamide A, Yoshida M, Maio K (2013) The natural clinical course of lumbar spinal stenosis: a longitudinal cohort study over a minimum of 10 years. J Orthop Sci 18(5):693–698. https://doi.org/10.1007/s00776-013-0435-9
Gibson JN, Waddell G (2005) Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine (Phila Pa 1976) 30 (20):2312–2320. https://doi.org/10.1097/01.brs.0000182315.88558.9c
Tsutsui S, Kagotani R, Yamada H et al (2013) Can decompression surgery relieve low back pain in patients with lumbar spinal stenosis combined with degenerative lumbar scoliosis? Eur Spine J 22(9):2010–2014. https://doi.org/10.1007/s00586-013-2786-5
Carreon LY, Puno RM, Dimar JR 2nd et al (2003) Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 85(11):2089–2092. https://doi.org/10.2106/00004623-200311000-00004
Cassinelli EH, Eubanks J, Vogt M et al (2007) Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976) 32 (2):230–235. https://doi.org/10.1097/01.brs.0000251918.19508.b3
Glassman SD, Carreon LY, Dimar JR et al (2007) Clinical outcomes in older patients after posterolateral lumbar fusion. Spine J 7(5):547–551. https://doi.org/10.1016/j.spinee.2006.11.003
Kim HS, Paudel B, Jang JS et al (2017) Percutaneous Full Endoscopic Bilateral Lumbar Decompression of Spinal Stenosis Through Uniportal-Contralateral Approach: Techniques and Preliminary Results. World Neurosurg 103:201–209. https://doi.org/10.1016/j.wneu.2017.03.130
Kim HS, Patel R, Paudel B et al (2017) Early Outcomes of Endoscopic Contralateral Foraminal and Lateral Recess Decompression via an Interlaminar Approach in Patients with Unilateral Radiculopathy from Unilateral Foraminal Stenosis. World Neurosurg 108:763–773. https://doi.org/10.1016/j.wneu.2017.09.018
Li X, Han Y, Di Z et al (2016) Percutaneous endoscopic lumbar discectomy for lumbar disc herniation. J Clin Neurosci 33:19–27. https://doi.org/10.1016/j.jocn.2016.01.043
Kim M, Lee S, Kim HS et al (2018) A Comparison of Percutaneous Endoscopic Lumbar Discectomy and Open Lumbar Microdiscectomy for Lumbar Disc Herniation in the Korean: A Meta-Analysis. Biomed Res Int 2018:9073460. https://doi.org/10.1155/2018/9073460
Lv Z, Jin L, Wang K et al (2019) Comparison of Effects of PELD and Fenestration in the Treatment of Geriatric Lumbar Lateral Recess Stenosis. Clin Interv Aging 14:2187–2194. https://doi.org/10.2147/cia.S226295
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Sankar A, Johnson SR, Beattie WS et al (2014) Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth 113(3):424–432. https://doi.org/10.1093/bja/aeu100
Pfirrmann CW, Metzdorf A, Zanetti M et al (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26 (17):1873–1878. https://doi.org/10.1097/00007632-200109010-00011
Brouwer PA, Peul WC, Brand R et al (2009) Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial. BMC Musculoskelet Disord 10:49. https://doi.org/10.1186/1471-2474-10-49
Antoniadis A, Ulrich NH, Schmid S et al (2017) Decompression surgery for lumbar spinal canal stenosis in octogenarians; a single center experience of 121 consecutive patients. Br J Neurosurg 31(1):67–71. https://doi.org/10.1080/02688697.2016.1233316
Shabat S, Arinzon Z, Folman Y et al (2008) Long-term outcome of decompressive surgery for lumbar spinal stenosis in octogenarians. Eur Spine J 17(2):193–198. https://doi.org/10.1007/s00586-007-0514-8
Kalff R, Ewald C, Waschke A et al (2013) Degenerative lumbar spinal stenosis in older people: current treatment options. Dtsch Arztebl Int 110 (37):613–623; quiz 624. https://doi.org/10.3238/arztebl.2013.0613
Deyo RA, Mirza SK, Martin BI et al (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–1265. https://doi.org/10.1001/jama.2010.338
Saleh A, Thirukumaran C, Mesfin A et al (2017) Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J 17(8):1106–1112. https://doi.org/10.1016/j.spinee.2017.03.019
Lee CH, Choi M, Ryu DS et al (2018) Efficacy and Safety of Full-endoscopic Decompression via Interlaminar Approach for Central or Lateral Recess Spinal Stenosis of the Lumbar Spine: A Meta-analysis. Spine (Phila Pa 1976) 43 (24):1756–1764. https://doi.org/10.1097/BRS.0000000000002708
Li H, Ou Y, Xie F et al (2020) Linical efficacy of percutaneous endoscopic lumbar discectomy for the treatment of lumbar spinal stenosis in elderly patients: a retrospective study. J Orthop Surg Res 15(1):441. https://doi.org/10.1186/s13018-020-01968-0
Hu D, Fei J, Chen G et al (2019) Treatment for lumbar spinal stenosis in elderly patients using percutaneous endoscopic lumbar discectomy combined with postoperative three-dimensional traction. Expert Rev Med Devices 16(4):317–323. https://doi.org/10.1080/17434440.2019.1599282
Lin Y-P, Wang S-L, Hu W-X et al (2020) Percutaneous Full-Endoscopic Lumbar Foraminoplasty and Decompression by Using a Visualization Reamer for Lumbar Lateral Recess and Foraminal Stenosis in Elderly Patients. World Neurosurgery 136:e83–e89. https://doi.org/10.1016/j.wneu.2019.10.123
Tang S, Jin S, Liao X et al (2018) Transforaminal Percutaneous Endoscopic Lumbar Decompression by Using Rigid Bendable Burr for Lumbar Lateral Recess Stenosis: Technique and Clinical Outcome. Biomed Res Int 2018:2601232. https://doi.org/10.1155/2018/2601232
Whitmore RG, Stephen JH, Vernick C et al (2014) ASA grade and Charlson Comorbidity Index of spinal surgery patients: correlation with complications and societal costs. Spine J 14(1):31–38. https://doi.org/10.1016/j.spinee.2013.03.011
Rault F, Briant AR, Kamga H et al (2022) Surgical management of lumbar spinal stenosis in patients over 80: is there an increased risk? Neurosurg Rev 45(3):2385–2399. https://doi.org/10.1007/s10143-022-01756-w
Park JH, Park S, Choi SA (2020) Incidence and risk factors of spinal epidural hemorrhage after spine surgery: a cross-sectional retrospective analysis of a national database. BMC Musculoskelet Disord 21(1):324. https://doi.org/10.1186/s12891-020-03337-8
Lee CK, Choi SK, Shin DA et al (2019) Influence of diabetes mellitus on patients with lumbar spinal stenosis: A nationwide population-based study. PLoS One 14(3):e0213858. https://doi.org/10.1371/journal.pone.0213858
Li G, Patil CG, Lad SP et al (2008) Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine (Phila Pa 1976) 33 (11):1250–1255. https://doi.org/10.1097/BRS.0b013e3181714a44
Imajo Y, Taguchi T, Neo M et al (2017) Complications of spinal surgery for elderly patients with lumbar spinal stenosis in a super-aging country: An analysis of 8033 patients. J Orthop Sci 22(1):10–15. https://doi.org/10.1016/j.jos.2016.08.014
Li P, Tong Y, Chen Y et al (2021) Comparison of percutaneous transforaminal endoscopic decompression and short-segment fusion in the treatment of elderly degenerative lumbar scoliosis with spinal stenosis. BMC Musculoskelet Disord 22(1):906. https://doi.org/10.1186/s12891-021-04804-6
Author information
Authors and Affiliations
Contributions
Conceptualization: Lei Wang and Lei Zang; methodology: Lei Wang and Tianyi Wang; formal analysis and investigation: Ning Fan and Shuo Yuan; writing—original draft preparation: Lei Wang and Peng Du; writing—review and editing: Peng Du and Fangda Si; resources: Lei Zang; supervision: Lei Zang.
Corresponding author
Ethics declarations
Ethics approval
The research conducted has been performed in accordance with the Declaration of Helsinki. Approval for the study was obtained from the ethics committees of the Beijing Chaoyang Hospital (2021-KE-478). Informed consent to this study was waived because of this was a retrospective study, which was also approved by the institutional ethical review board.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Conflicts of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, L., Wang, T., Fan, N. et al. Clinical outcome of percutaneous endoscopic lumbar decompression in treatment of elderly patients with lumbar spinal stenosis: a matched retrospective study. International Orthopaedics (SICOT) 48, 201–209 (2024). https://doi.org/10.1007/s00264-023-05947-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05947-y