Abstract
Purpose
Severe acetabular bone defect is challenging in revision hip arthroplasty. In the present study, we aimed to present new treatment options with the 3D printing technique and analyze the clinical and radiographic outcomes of 3D-printed titanium implants for the treatment of severe acetabular bone defects in revision hip arthroplasty.
Methods
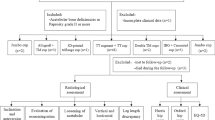
A total of 35 patients with Paprosky type 3 bone defect and pelvic discontinuity (PD), who underwent hip revisions using 3D-printed titanium implants between 2016 and 2019 at our institution, were retrospectively reviewed. Patient-specific 3D-printed titanium augments and shells (strategy A) were used in 22 type 3A and two type 3B patients. Custom 3D-printed flanged components (strategy B) were used in 11 type 3B patients, including five PD. The clinical outcomes were evaluated with the Harris hip score (HHS). In addition, radiographic results were analyzed by the hip centre of rotation (V-COR and H-COR), implant failure, and survivorship.
Results
The mean follow-up was 41.5 months (range, 16–62). The HHS was improved from 47.8 ± 8.2 pre-operatively to 78.1 ± 10.1 at one year follow-up and 86.4 ± 5.1 at the last follow-up (p < 0.01). Post-operative V-COR and H-COR of the operated side were 20.8 ± 2.0 mm and 30.2 ± 1.6 mm compared with 51.4 ± 4.1 mm and 33.9 ± 9.0 mm pre-operatively (p < 0.01). The complications included one dislocation and one partial palsy of the sciatic nerve. At the latest follow-up, no radiological component loosening or screw breakage was present.
Conclusions
3D-printed titanium implants showed satisfactory short- and mid-term clinical and radiographic outcomes. It was an effective therapeutic regimen with a low rate of complications, providing a patient-specific and reliable strategy for the severe acetabular bone defect in revision hip arthroplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With an aging population and a trend for primary total hip arthroplasty (THA) being performed in younger patients, the number of THA procedures is growing rapidly in recent years, which is accompanied by a corresponding increase in revision THA [1, 2]. As common findings in hip revisions, acetabular bone defects are usually caused by osteolysis, infection, trauma, and adverse reaction to wear debris. Severe acetabular bone defects, involving Paprosky type 3A, 3B, and pelvic discontinuity (PD), are characterized by unsupportive acetabular rim or columns, commonly with a remarkable migration of the hip center [3]. The treatment of severe acetabular bone defect in the revision THA procedure is challenging. Multiple therapeutic regimens have been reported for addressing this issue, including porous metal augments and shells, jumbo cups, structural allografts, antiprotrusio cages, and cup-cage constructs [4,5,6,7,8]. However, the best surgical strategy has not been recognized, and none of the mentioned options has provided predictable and satisfactory long-term clinical outcomes [9,10,11].
More recently, with the development of 3D additive manufacturing, a new alternative has become available to manage severe acetabular bone defects in hip revisions [12, 13]. In the present study, we introduced patient-specific 3D-printed titanium augments and flanged components, manufactured with the electron beam melting (EBM) technique [14], to manage Paprosky type 3A, 3B bone defects, and PD.
The purpose of the current study was to present the whole treatment process with the 3D-printing technique, including bone defect assessment, preoperative planning, strategic decision-making, and the usage of 3D-printed implants to guide the treatment of severe acetabular bone defects in hip revisions with 3D printing technique. We also analyzed complications and clinical and radiographic outcomes of this technique. We hypothesized that a 3D-printed titanium implant was an effective treatment for severe acetabular bone defects in revision hip arthroplasty.
Material and methods
Participants
Our institutional database was retrospectively reviewed to identify patients with acetabular bone defects, who underwent a hip revision using 3D-printed titanium implants between January 2016 and December 2019. Acetabular bone defects were evaluated according to Paprosky classification using pre-operative plain radiographs. The inclusion criteria were set as follows: patients with Paprosky type 3A, 3B bone defects, and PD. Exclusion criteria were set as follows: (i) recent periprosthetic infection; (ii) acetabular defects due to bone tumours; and (iii) less than one year of follow-up. The study was approved by our institutional review board (IRB) and ethical committee.
Pre-operative planning and implant manufacture
Following a thin-slice CT scan, 3D reconstruction images of the patient’s hemipelvis (Fig. 1B) were generated with software (Mimics, Materialise, Belgium) by a professional engineer. A life-sized model of the involved hemipelvis (Figs. 1C and 2B) was then created by 3D printing based on the data of 3D reconstruction images, providing a visualized geometry and accurate assessment of the acetabular bone defect. With the computer-aided design (CAD) software (Magics, Materialise, Belgium), a digital design proposal for the implant was created (Fig. 1D).
A 65-year-old female with Paprosky 3A acetabular bone defect. A Pre-operative radiograph of bilateral hips. B 3D reconstruction images. C Life-sized hemipelvis model. D Digital proposal with the CAD: a patient-specific augment with a shell. E Pre-operative trial surgery using prototype augment and hemipelvis model. F–G 3D-printed titanium augment and shell. H–I The prototype augment highly matched the defect, and the trial shell was impacted stably. J One-month post-operative radiograph
A 66-year-old female with Paprosky 3B acetabular bone defect. A Pre-operative radiograph. B Life-sized hemipelvis model. C Pre-operative trial surgery using custom component prototype and hemipelvis model. D Custom 3D-printed flanged component. E–F One-month post-operative radiograph and CT. G-K Two-year post-operative radiograph and CT
After the virtual proposal was confirmed by the surgeon, prototype implants were created and utilized on the hemipelvis model for pre-operative trial surgery (Figs. 1E and 2C). In general, a patient-specific augment with a hemisphere cup (strategy A) was commonly accepted and preferred. However, in some complex cases of Paprosky type 3B or PD, if augments and residual host bone could not ensure sufficient stability of a hemispherical cup, a custom 3D-printed flanged component (strategy B) was recommended. Additionally, some considerations were taken into account while proposing, including (i) a maximal filling of the bone defect to restore bone stock; (ii) an optimal size and location of the component to restore the centre of rotation; and (iii) proper number, positions, lengths, and trajectories of screws to ensure a stable implant fixation while avoiding the risk of neurovascular injury.
Once the surgical plan was testified feasible, the design proposal of patient-specific implants was finalized. Then, implants were manufactured from layered titanium alloy (Ti6Al4V) powders with the EBM 3D printing system (Arcam AB, Sweden) (Figs. 1F–G and 2D).
Surgical procedure
All operations were performed by a senior surgeon (XLS). In the lateral decubitus position, an extended Hardinge approach was used for all hips. After achieving adequate exposure, all failed implants were carefully removed, and a meticulous debridement was performed. Then, the residual bone stock and defect were reassessed. If the intra-operative situation was consistent with the pre-operative evaluation, the predetermined plan was carried out.
In strategy A, after the osseous bed was prepared by gentle reaming, the prototype augment and a trial shell with a pre-measured size were introduced to reconfirm the bone defect match and host bone contact (Fig. 1H–I). Then, the patient-specific titanium augment was placed into the defect and fixed with screws. Subsequently, a porous titanium acetabular shell (3D ACT cup, AK Medical, China) was impacted, connecting the augment with cement. At least two dome or peripheral screws through the acetabular shell were necessary to gain sufficient initial stability. If possible, more screws through both the shell and augment were recommended. Finally, a polyethylene liner was used with a large femoral head.
In strategy B, adequate exposure of the ilium, ischium, and sometimes pubis was needed to gain a broad view of the defect and enough surfaces for implant fixation. Meanwhile, care must be taken to avoid damage to the sciatic nerve and the superior gluteal neurovascular bundle. Fresh frozen femoral head bone allografts were used to fill defects in all cases, particularly at the site of PD. Subsequently, the custom 3D-printed flanged component was inserted and fixed to the host bone by as many screws as possible. The polyethylene liner was then cemented into the component with proper abduction and anteversion angles to restore the hip center of rotation.
Femoral revisions were carried out with long cementless stems (SL, AK Medical, China) in eight type 3A patients and eight type 3B patients, including four PD.
All patients received prophylactic anti-infection and low-dose anticoagulation post-operatively. Partial weight-bearing was permitted for the first six weeks with a gradual increase to full weight-bearing thereafter.
Clinical and radiological evaluations
Clinical and radiological evaluations were performed preoperatively, at one, three, six and 12 months after discharge and then one or two annually thereafter. Harris hip score (HHS) was recorded to assess the clinical function of the hip. All patients underwent an anteroposterior radiograph or CT scan of bilateral hips at each follow-up. The hip centre of rotation (COR) was evaluated by V-COR and H-COR. V-COR was measured as the vertical distance between the centre of the femoral head and the inter-teardrop line. H-COR was measured as the horizontal distance between the centre of the femoral head and the perpendicular line through the inferior point of the teardrop (Fig. 3). Radiologic failures were defined as a component migration of more than 5 mm, variation of inclination greater than 5°, progressive radiolucencies, and hardware breakage.
Radiographic measurements of the hip center of rotation (COR). V-COR: the vertical distance between the centre of the femoral head and the inter-teardrop line (line A). H-COR: the horizontal distance between the centre of the femoral head and the perpendicular line (line B) through the inferior point of the teardrop
Statistical analysis
The paired t-test was performed to analyze the difference between pre- and post-operative HHS, V-COR, and H-COR using SPSS software (Version 25, IBM, USA). A p < 0.05 was considered statistically significant.
Results
Demographic details
A total of 35 patients, including 12 males and 23 females, met the inclusion criteria and were finally enrolled in the study cohort. The average age for revision surgery was 70.6 years (range, 53–83 years). The mean interval from primary THA to revision surgery was 10.2 years (range, 6–20 years). Reasons for revision included aseptic loosening in 27 hips, osteolysis related to metal wear debris in six hips, and a two-stage procedure for periprosthetic infection in two hips. In this series, the surgery was the first revision for 33 of 35 patients except for two patients with a two-stage procedure for periprosthetic infection. According to Paprosky classification, 22 hips were type 3A, and 13 hips were type 3B, including five PD. Patient-specific titanium augments and shells (strategy A) were used in 22 type 3A and two type 3B patients. Custom 3D-printed flanged components (strategy B) were used in 11 type 3B patients, including five PD. The mean duration of postoperative follow-up was 41.5 months (range, 16–62 months). None of the patients died or was lost during follow-up (Table 1).
Clinical and radiographic outcomes
The HHS was increased from 47.8 ± 8.2 pre-operatively to 78.1 ± 10.1 at one year follow-up and 86.4 ± 5.1 at the last follow-up. Significant differences (p < 0.05) were observed between any two of the three datasets.
The V-COR of the operated side was decreased from 51.4 ± 4.1 mm pre-operatively to 20.8 ± 2.0 mm at one year post-operative follow-up (p < 0.001). Post-operative H-COR of the operated side was 30.2 ± 1.6 mm compared with 33.9 ± 9.0 mm pre-operatively (p < 0.001). Both the post-operative V-COR (19.5 ± 1.2 mm) and H-COR (31.2 ± 1.7 mm) of the contralateral side were different from those of the operated side respectively (p < 0.001) (Table 2).
In one patient with Paprosky type 3B defect of strategy A, a 2-mm cranial migration of the acetabular component was observed on the radiograph at a one month follow-up. Without any weight-bearing in the following two months, the component was stabilized with osteointegration at three month follow-up post-operatively. At the latest follow-up, no radiological component loosening or screw breakage was present. In the hips with PD, the acetabular bone stock appeared to be incorporated.
Complications
Complications were recorded in two patients in the present study. One patient had a partial palsy of the sciatic nerve and resolved spontaneously within four weeks post-operatively. The other patient presented with dislocation five weeks after surgery and was treated with closed reduction, followed by transcutaneous traction for four weeks, and no further dislocations were encountered thereafter. No cases of deep infection, thromboembolism, or implant failure were noted.
Discussion
Hip revision with a severe acetabular bone defect is challenging, especially when major segmental bone loss or PD is involved, in which the defect is highly variable, and residual host bone is incapable of supporting a hemispherical cup [15, 16]. In the present study, we reported the usage of 3D-printed titanium implants to address severe acetabular bone defects and restore hip biomechanics in revision hip arthroplasty. This technique showed encouraging outcomes with no implant failure or major complications at a mean follow-up of 41.5 months.
Compared with traditional treatments, the new alternative with the 3D-printing technique in this article had several advantages. First, a more accurate assessment of bone defects was achieved pre-operatively. We believed that a precise bone defect assessment was the crucial premise to determine the optimal surgical strategy. According to the 3D reconstruction images generated by software, the bone defect could be easily identified and assessed from multiple views. Meanwhile, a 3D-printed life-sized hemipelvis model was manufactured to provide more realistic insights into the anatomy of the patient’s pelvic and the geometry of complex bone defects.
Second, the optimal surgical strategy could be determined. It was a core issue in this article that how to choose between two strategies for different types of severe acetabular bone defects. In general, a patient-specific augment with a hemisphere shell (strategy A) was preferred to be considered. An operative plan could be designed, modified, and presented by 3D software on the computer. According to the 3D simulation figures, we could evaluate the contact area between the shell and the host bone. We highlighted the support from the posterior stock (especially the posteroinferior part), anterior stock (especially the anterosuperior part), and the top of the acetabulum. If these areas were deficient and might not be restored by augments or bone grafts, the stability of a hemispherical cup was probably not ensured. Then custom flanged components (strategy B) should be used. Moreover, strategy A was not recommended for PD because the augment could not restore the continuity of the pelvis. Once the surgeon confirmed the preliminary plan, a trial surgery would be performed with 3D-printed prototype implants on the life-sized hemipelvis model. With the trial surgery, the placement of implants, the stability of the component, and the fixation of screws could be tested in advance. As a result, the time of actual surgery and the risk of intra-operative complications were reduced [17,18,19].
Third, compared with conventional treatments, 3D-printed implants could well match the patient’s anatomy and reconstruct better hip COR. To the best of our knowledge, there are few reports of patient-specific augments used for acetabular bone defects in hip revisions. Compared with a conventional augment, a patient-specific augment could better match the irregular bone defect and avoid a mismatch between the inner diameter of the augment and the outer diameter of the chosen hemispherical shell (Fig. 1F). In our series, post-operative radiographs showed the patient-specific implants highly match the host bone and defects in all cases. Additionally, all implants were placed in the expected positions, which were highly consistent with pre-operative plans. Our results were comparable with those of Weber [20] and Durand-Hill [21], who have reported the deviation between planned and achieved component positions by CT scans in patients undergoing hip revisions with custom 3D-printed components.
Recent literature has reported that Paprosky type 3A acetabular bone defects can also be treated by jumbo cups [6]. However, jumbo cup revision does not restore bone stock and more host bone will be removed when reaming the oval acetabulum to form a large hemisphere. Additionally, as the cup diameter increases, the hip COR shifts superiorly and laterally, leading to a variation of offset and an increased risk of dislocation [22, 23]. The issue of COR deviation has also been reported in using conventional cages for Paprosky type 3B defects and PD [10]. Compared with these treatments without the 3D printing technique, our results showed that both the postoperative V-COR and H-COR of the operated side were very close to those of the contralateral side (less than 2 mm on average), demonstrating that 3D-printed implants could reconstruct better hip COR.
Forth, 3D-printed titanium implants had better biomechanics and capacity for bone ingrowth. In our present study, severe Paprosky type 3B bone defect and PD were the most challenging scenarios, in which augments with a hemispherical shell could not yield a stable reconstruction. Antiprotrusio cages are widely reported for treating these problems [9]. However, there is no bone ingrowth in the cage, leading to high failure rates in mid- and long-term follow-ups [10, 24]. Therefore, antiprotrusio cages are only suitable for elderly patients with low activities [9]. Recently, the cup-cages have been increasingly reported to treat Paprosky type 3B defect and PD [8, 11, 25]. Nevertheless, the flanges of the cage have no bone ingrowth, and the success of the cup-cage construct relies on how much bony ingrowth is into the cup itself. If the cup can not span the defect or be fixed stably with multiple screws, the cup-cage construct is still likely to fail. However, in our study, this challenging issue was well resolved by a custom 3D-printed flanged component, which was able to span huge bone defects and obtain initial stability with multiple iliac and ischial screws [19, 26]. Manufactured by EBM 3D printing technology, the custom titanium flanged components were characterized by high porosity, low modulus of elasticity, and high friction coefficient, providing better primary stability, improved physiological stress transfer, and favorable bone ingrowth [14, 27, 28]. In our series, 11 type 3B patients, including five PD, were treated with EBM-produced flanged components. All the components had radiological osseointegration, and there was no implant loosening or failure on the radiographs at the last follow-up.
Compared with previous literature using custom 3D-printed implants for severe acetabular bone defects in hip revisions [13, 19, 29, 30], the present study showed better clinical and functional results with fewer complications. There were several reasons. First, the proportion of PD was low in our series. Second, most patients underwent the operation as the first revision surgery without muscle injury, superior gluteal nerve injury, or abductor insufficiency secondary to repeated hip surgery. Third, 16 of 35 patients underwent a concomitant femoral revision, which helped restore combined anteversion, leg length, and hip offset. Therefore, the dislocation rate was low. Moreover, we highlighted the importance of multiple-screw fixation to provide initial implant instability. We recommended introducing screws as much as possible, preferably in the direction of load transfer. However, care must be taken to avoid injury to the superior gluteal neurovascular pedicle and sciatic nerve. Finally, abundant bone allografts were highly recommended to fill the defect and improve osseointegration.
There are some limitations in this study, including the relatively small sample size and retrospective design. A further limitation is that the mean follow-up of 41.5 months is relatively short. Longer follow-up remains to be performed to better reveal long-term clinical outcomes, complications, and survivorship. Besides, another drawback of a 3D-printed implant is that several additional weeks are required from design to manufacture. Moreover, its overall cost is higher than other techniques.
Conclusions
This study demonstrated that the 3D-printed titanium implant was an effective treatment for severe acetabular bone defects in hip revision. This technique provided satisfactory clinical and radiographic outcomes, a low complication rate, and a high survival rate of implants with short- and mid-term follow-ups. However, long-term outcomes still need to be examined.
Author contribution statement
Sheng Fang and Huan Li contributed to the study design. Yiming Wang and Peng Xu constructed the database and collated the data. Junke Zhu and Jinbo Liu analyzed the data. Sheng Fang and Xiaoliang Sun contributed to writing the manuscript. All authors read and approved the final manuscript.
References
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 100:1455–1460. https://doi.org/10.2106/jbjs.17.01617
Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr (2020) Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty 35:S79-s85. https://doi.org/10.1016/j.arth.2020.02.030
Telleria JJ, Gee AO (2013) Classifications in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res 471:3725–3730. https://doi.org/10.1007/s11999-013-3264-4
Fryhofer GW, Ramesh S, Sheth NP (2020) Acetabular reconstruction in revision total hip arthroplasty. J Clin Orthop Trauma 11:22–28. https://doi.org/10.1016/j.jcot.2019.11.004
Löchel J, Janz V, Hipfl C, Perka C, Wassilew GI (2019) Reconstruction of acetabular defects with porous tantalum shells and augments in revision total hip arthroplasty at ten-year follow-up. Bone Joint J 101-b:311–316. https://doi.org/10.1302/0301-620x.101b3.Bjj-2018-0959.R1
Gustke KA, Levering MF, Miranda MA (2014) Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty 29:199–203. https://doi.org/10.1016/j.arth.2012.11.010
Hosny HAH, El-Bakoury A, Fekry H, Keenan J (2018) Mid-term results of graft augmentation prosthesis II cage and impacted allograft bone in revision hip arthroplasty. J Arthroplasty 33:1487–1493. https://doi.org/10.1016/j.arth.2017.11.060
Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE (2009) Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br 91:870–876. https://doi.org/10.1302/0301-620x.91b7.22181
Baauw M, van Hooff ML, Spruit M (2016) Current construct options for revision of large acetabular defects: a systematic review. JBJS reviews 4. https://doi.org/10.2106/jbjs.Rvw.15.00119
Chang CY, Wu CT, Numan H, Kuo FC, Wang JW, Lee MS (2021) Survival analysis of allografting and antiprotrusio cage in treating massive acetabular bone defects. J Arthroplasty 36:682–687. https://doi.org/10.1016/j.arth.2020.08.050
Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI (2018) Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J 100-b:1442–1448. https://doi.org/10.1302/0301-620x.100b11.Bjj-2018-0481.R1
Burastero G, Cavagnaro L, Chiarlone F, Zanirato A, Mosconi L, Felli L, de Lorenzo FDR (2020) Clinical study of outcomes after revision surgery using porous titanium custom-made implants for severe acetabular septic bone defects. Int Orthop 44:1957–1964. https://doi.org/10.1007/s00264-020-04623-9
Chiarlone F, Zanirato A, Cavagnaro L, Alessio-Mazzola M, Felli L, Burastero G (2020) Acetabular custom-made implants for severe acetabular bone defect in revision total hip arthroplasty: a systematic review of the literature. Arch Orthop Trauma Surg 140:415–424. https://doi.org/10.1007/s00402-020-03334-5
Tamayo JA, Riascos M, Vargas CA, Baena LM (2021) Additive manufacturing of Ti6Al4V alloy via electron beam melting for the development of implants for the biomedical industry. Heliyon 7:e06892. https://doi.org/10.1016/j.heliyon.2021.e06892
Paprosky WG, Sporer SS, Murphy BP (2007) Addressing severe bone deficiency: what a cage will not do. J Arthroplasty 22:111–115. https://doi.org/10.1016/j.arth.2007.01.018
Petrie J, Sassoon A, Haidukewych GJ (2013) Pelvic discontinuity: current solutions. Bone Joint J 95-b:109–113. https://doi.org/10.1302/0301-620x.95b11.32764
Tserovski S, Georgieva S, Simeonov R, Bigdeli A, Röttinger H, Kinov P (2019) Advantages and disadvantages of 3D printing for pre-operative planning of revision hip surgery. J Surg Case Rep 2019:rjz214. https://doi.org/10.1093/jscr/rjz214
Hughes AJ, DeBuitleir C, Soden P, O’Donnchadha B, Tansey A, Abdulkarim A, McMahon C, Hurson CJ (2017) 3D printing aids acetabular reconstruction in complex revision hip arthroplasty. Adv Orthop 2017:8925050. https://doi.org/10.1155/2017/8925050
Berasi CCT, Berend KR, Adams JB, Ruh EL, Lombardi AV Jr (2015) Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res 473:528–535. https://doi.org/10.1007/s11999-014-3969-z
Weber M, Witzmann L, Wieding J, Grifka J, Renkawitz T, Craiovan B (2019) Customized implants for acetabular Paprosky III defects may be positioned with high accuracy in revision hip arthroplasty. Int Orthop 43:2235–2243. https://doi.org/10.1007/s00264-018-4193-3
Durand-Hill M, Henckel J, Di Laura A, Hart AJ (2020) Can custom 3D printed implants successfully reconstruct massive acetabular defects? A 3D-CT assessment. J Orthop Res 38:2640–2648. https://doi.org/10.1002/jor.24752
Nwankwo CD, Ries MD (2014) Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res 472:2793–2798. https://doi.org/10.1007/s11999-014-3632-8
Nwankwo C, Dong NN, Heffernan CD, Ries MD (2014) Do jumbo cups cause hip center elevation in revision THA? A computer simulation. Clin Orthop Relat Res 472:572–576. https://doi.org/10.1007/s11999-013-3169-2
Marongiu G, Podda D, Mastio M, Capone A (2019) Long-term results of isolated acetabular revisions with reinforcement rings: a 10- to 15-year follow-up. Hip Int 29:385–392. https://doi.org/10.1177/1120700018802750
Amenabar T, Rahman WA, Hetaimish BM, Kuzyk PR, Safir OA, Gross AE (2016) Promising mid-term results with a cup-cage construct for large acetabular defects and pelvic discontinuity. Clin Orthop Relat Res 474:408–414. https://doi.org/10.1007/s11999-015-4210-4
Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ (2012) Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res 470:428–434. https://doi.org/10.1007/s11999-011-2126-1
Goto M, Matsumine A, Yamaguchi S, Takahashi H, Akeda K, Nakamura T, Asanuma K, Matsushita T, Kokubo T, Sudo A (2021) Osteoconductivity of bioactive Ti-6Al-4V implants with lattice-shaped interconnected large pores fabricated by electron beam melting. J Biomater Appl 35:1153–1167. https://doi.org/10.1177/0885328220968218
Huang Y, Zhou YX, Tian H, Wang JW, Liu WG, Li H (2021) Minimum 7-year Follow-up of a porous coated trabecular titanium cup manufactured with electron beam melting technique in primary total hip arthroplasty. Orthop Surg 13:817–824. https://doi.org/10.1111/os.12846
De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK (2019) Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplasty 34:2511–2518. https://doi.org/10.1016/j.arth.2019.05.032
Berend ME, Berend KR, Lombardi AV, Cates H, Faris P (2018) The patient-specific triflange acetabular implant for revision total hip arthroplasty in patients with severe acetabular defects: planning, implantation, and results. Bone Joint J 100-b:50–54. https://doi.org/10.1302/0301-620x.100b1.Bjj-2017-0362.R1
Acknowledgements
This work was supported by the Youth Talents Science and Technology Project of Changzhou Health Commission (QN201919).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by the internal review board and ethical committee of the Third Affiliated Hospital of Soochow University.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fang, S., Wang, Y., Xu, P. et al. Three-dimensional-printed titanium implants for severe acetabular bone defects in revision hip arthroplasty: short- and mid-term results. International Orthopaedics (SICOT) 46, 1289–1297 (2022). https://doi.org/10.1007/s00264-022-05390-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05390-5