Abstract
Purpose
We compared the magnetic resonance imaging (MRI)-confirmed cyst formation rate after meniscal tear repair using a new all-inside suture device (N group) versus the older all-inside suture device (O group).
Methods
Between October 2008 and July 2017, 94 consecutive menisci of 89 patients were diagnosed with meniscal tears and underwent arthroscopic meniscal repair using the all-inside suture device. Five of these patients were lost to follow-up within 12 months and were excluded from the study. The remaining 89 menisci were followed up for at least 12 months and were included in this retrospective cohort study. Older all-inside suture devices (FasT-Fix, Ultra FasT-Fix) were used until December 2012, while the new all-inside suture device (FasT-Fix 360) was used from January 2013 onwards. Meniscal cysts were detected on T2-weighted fat-suppressed MRI at 12 months postoperatively. Multiple logistic regression analysis was used to identify demographic and clinical factors associated with the use of the new all-inside suture device and cyst formation.
Results
In total, 36 and 53 menisci were included in the N and O groups, respectively. The incidence of meniscal cysts was significantly greater in the O group (14 out of 53, 26.4%) than in the N group (two out of 36, 5.56%) (P = 0.012). Two patients in the O group had symptomatic cysts that required removal. Multivariate logistic analyses showed that the cyst formation risk significantly decreased after using the new all-inside suture device than the older all-inside suture devices (odds ratio = 0.139; P = 0.04).
Conclusions
The MRI-confirmed cyst formation rate after meniscal tear repair was significantly lower using the new than the older all-inside suture devices, indicating that the use of a low-profile device may decrease the cyst formation rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The formation of meniscal cysts is related to meniscal mucoid degeneration, trauma, and meniscal tear and repair [1,2,3,4,5]. Meniscal cyst formation after meniscal repair is considered relatively rare. Although there are limited reported cases [2,3,4,5,6,7,8], the use of an all-inside (AI) device and medial meniscal tears are suggested to be risk factors for cyst formation after meniscal repair [2,3,4,5,6, 8, 9]. The AI device was designed to shorten the operative time and minimize the risk of neurovascular structure injury compared with the inside-out technique. Moreover, there were no significant differences in the clinical outcomes between all-inside meniscal repair using sutures and the AI device [10, 11]. However, the AI device was reportedly associated with complications, including cyst formation, implant breakage/migration, swelling, nerve irritation, and chondral damage [12, 13]. The FasT-Fix (Smith & Nephew, Endoscopy Division, Andover, MA) has been widely used as a meniscal repair device worldwide since its release in 2002 [14, 15]; then, the Ultra FasT-Fix was released in 2005, and the low-profile FasT-Fix 360 was released in 2013 in Japan. To the best of our knowledge, only limited data are available regarding the incidence rate of cyst formation after meniscal repair using the FasT-Fix 360 compared to those after using the older FasT-Fix devices (FasT-Fix and Ultra FasT-Fix).
We aimed to compare the magnetic resonance imaging (MRI)-confirmed cyst formation rate after meniscal repair using the new and older FasT-Fix devices. We hypothesized that the new FasT-Fix 360 would decrease the cyst formation rate compared with the older FasT-Fix devices.
Patients and methods
Consecutive patients who were diagnosed with meniscal tears and underwent arthroscopic meniscal repair with the AI technique between October 2008 and July 2017 by a single senior surgeon were retrospectively evaluated. The inclusion criteria were the diagnosis of meniscal tears, previous arthroscopic meniscal repair with the FasT-Fix, and previous MRI examination. The exclusion criteria were a prior meniscal surgery and a follow-up period < 12 months. Ninety-four consecutive menisci of 89 patients underwent arthroscopic meniscal repair with a FasT-Fix. Five of these patients were lost to follow-up within 12 months and were excluded from the study. The remaining 89 menisci were followed up for at least 12 months and were included in this retrospective cohort study. The indication for meniscal repair was a tear at the red-red or red-white zone of the posterior to middle portions of the medial or lateral meniscus. The FasT-Fix was used for meniscal tears less than 2 cm in length. If the tear was more than 2 cm, the menisci were repaired with an inside-out repair technique and the FasT-Fix was used for the lesion of the posterior horn. The older FasT-Fix devices were used until December 2012, while the new FasT-Fix 360 was used from January 2013.
Surgical technique
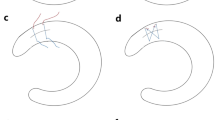
General anaesthesia was administered to all patients. Tourniquet was only used for the posteromedial incision when using the inside-out technique. Diagnostic arthroscopy was performed via an anterolateral portal with 30° oblique arthroscope; a probe was introduced via an anteromedial portal to determine the meniscal tear’s morphology. After confirmation of meniscal instability, defined as a longitudinal tear in the vascular area of the meniscus, the tear edge was freshened with a meniscus rasp and shaver to stimulate healing. Longitudinal tears with mild instability and horizontal tears with no peripheral tear were repaired with the AI technique only using the FasT-Fix. Longitudinal tears with instability and horizontal tears with a peripheral tear were repaired with the inside-out technique and with the AI technique using the FasT-Fix, if necessary (Fig. 1). When a FasT-Fix device was used for AI repair, the FasT-Fix device was used in accordance with the manufacturer’s recommendations and previously described techniques [14, 16, 17].
Patients with a discoid lateral meniscus (DLM) first underwent saucerization that consisted of centrifugal resection to shape the meniscus until a residual peripheral rim of 6–8 mm was confirmed at the meniscal mid-body with a calibrated probe. All anterior cruciate ligament (ACL) injuries were reconstructed with double-bundle ACL reconstruction using the inside-out technique.
Post-operative rehabilitation protocol
The postoperative rehabilitation protocol was dictated by the presence of concurrent ACL injury. The knee was fixed with a brace for one week and, then, the range-of-motion training of the knee was initiated. Passive range of motion was restricted from 0° to 90° of flexion for one week, and then progressed to 120° of flexion for six weeks. Full squatting beyond 120° and bicycling were allowed after 12 weeks. A non-weight-bearing period of three weeks was imposed. Partial and full weight-bearing began at three and six weeks post-operatively, respectively. Jogging was permitted from three months after isolated meniscal repair and after meniscal repair with ACL reconstruction. Return to sports activity was allowed from six months after isolated meniscal repair and after meniscal repair with ACL reconstruction.
Clinical evaluation
The pre- and postoperative Lysholm scores and the preinjury Tegner activity scale were used as subjective and objective assessments of the clinical parameters. Side-to-side difference was calculated using the KT-2000 knee arthrometer (MEDmetric Corporation, San Diego, CA) in those who underwent ACL reconstruction. If a meniscal cyst was present, the presence of pain around the cyst was investigated. Data were collected preoperatively and at 12 months post-operatively.
Radiographic evaluation
Meniscal cysts were detected on T2-weighted fat-suppressed MRI at 12 months postoperatively (Fig. 2). MRI examinations were performed for all cases pre-operatively and at 12 months post-operatively with a 3.0-Tesla scanner (Achieva 3.0 T TX; Philips, Amsterdam, The Netherlands). Meniscal cysts were not detected on MRI pre-operatively. The sequences used for image interpretation were coronal, sagittal, and axial proton density scans (TR/TE, 2117/10 ms; field of view, 16 cm; matrix, 256 9 256–192; slice thickness, 3.3 mm) and fat saturation scans (TR/TE, 3460/80 ms; field of view, 16 cm; matrix, 256 9 256–192; slice thickness, 3.3 mm). Two orthopaedic specialists who were blinded to the cases analyzed the MR images. Parameniscal cysts related to the FasT-Fix were defined as the presence of a mass more than 5 mm in size on sagittal and coronal images (“fish-eye” sign) in the area, in which the FasT-Fix was inserted (Fig. 2) [9, 13]. The fish-eye sign indicates a toggle anchor is observed in the cyst. The cyst size was measured on sagittal and coronal images, and the larger one was selected. Based on a previous study [18], meniscal healing was defined as a lower MRI signal intensity of the repaired portion of the meniscus than that of intra-articular fluid, while failure was defined as an equivalent MRI signal intensity to intra-articular fluid in the repaired portion.
Sagittal and coronal MRI images showing the “fish-eye” sign, which indicates the encasement of a suture anchor in a meniscal cyst (white arrow) [11, 13]. a A meniscal cyst case from the N group. b A meniscal cyst case from the O group. The meniscal cyst from the N group was smaller than the cyst from the O group. MRI, magnetic resonance imaging
Statistical analysis
The t test was used for continuous variables (age, Lysholm score, Tegner activity scale, and number of sutures). The χ2 test was used for categorical variables (sex, location of the meniscal tear, DLM, concomitant ACL tear, and cyst occurrence). Multivariable logistic regression was used to identify demographic and clinical factors associated with the use of new FasT-Fix and cyst formation. The odds ratios (OR) and 95% confidence intervals (CI) for cyst formation were determined among all patients. The significance level was set at P < 0.05. All hypotheses were tested assuming a 0.05 significance level and a two-sided alternative hypothesis. All statistical analyses were performed using SAS software, version 9.1 (SAS Institute Inc., Cary, NC). The reliability of measurements of the cyst was assessed using the interobserver and intraobserver intraclass correlation coefficient (ICC). The ICC was interpreted as poor, marginal, and good when it was < 0.4, ≧ 0.4 and < 0.75, and > 0.75, respectively.
Results
Pre- and intra-operative data
Demographic data are summarized in Table 1. Medial meniscal tears and concurrent ACL injury were significantly larger, and the follow-up duration was significantly longer in the O group than in the N group. The type of meniscal tear using FasT-Fix was as follows: N group: longitudinal, 35; bucket handle, seven; horizontal, six; flap, three; radial, two; O group: longitudinal, 23; bucket handle, one; horizontal, 11; flap, one.
Post-operative data
The post-operative data are summarized in Table 1. The incidence of meniscal cysts was significantly greater in the O group (14 out of 53, 26.4%) than in the N group (two out of 36, 5.56%) (P = 0.012). Meniscus tears were healed in more cases in the N group than in the O group. The data of the 16 patients with cyst formation are summarized in Table 2. The cyst size tended to be smaller in the N group than in the O group (Fig. 2). Two patients in the O group had a symptomatic cyst that required removal. In these patients, arthroscopy revealed that the meniscus was completely healed and, therefore, the cyst was removed via open excision. The cyst was found to be continuous with the anchors.
The mean Lysholm score significantly improved from preoperatively to post-operatively in the N and O groups (both P < 0.001). The mean post-operative Lysholm score did not differ significantly between the two groups (P = 0.485).
The interobserver ICC was 0.761 indicating a high agreement between evaluators. The intraobserver ICC was 0.907 indicating high agreement.
Logistic regression analyses of relative contribution of variables to use of new FasT-Fix
Table 3 shows demographic and clinical factors associated with use of new FasT-Fix according to multivariate logistic regression analyses. Multivariate logistic analyses showed that the risk of meniscal cyst formation decreased using the new FasT-Fix 360 (OR = 0.187; P = 0.053).
Comparison of cases with versus without meniscal cysts
Table 4 shows comparison of cases with versus without meniscal cysts. There were significantly more cyst cases in younger patients, male individuals, use of older more FasT-Fix devices, concurrent ACL injury, and increased use of FasT-Fix.
Risk factors contributing to cyst formation
Table 5 shows demographic and clinical factors associated with meniscal cyst formation according to multivariate logistic regression analyses. Multivariate logistic analyses showed that the meniscal cyst formation risk significantly decreased with the new FasT-Fix 360 (OR = 0.139; P = 0.04), and older age (OR = 0.850; P = 0.012), and significantly increased with a higher suture number of FasT-Fix (OR = 1.73; P = 0.042), and the presence of a medial meniscal tear (OR = 17.2; P = 0.005).
Discussion
The most important finding of this study was that the incidence of meniscal cysts was significantly lower in the new all-inside suture device group than in the older all-inside suture device group. Moreover, the use of the new FasT-Fix 360 significantly decreased the cyst formation risk compared with that after using older FasT-Fix devices. These results were consistent with our hypothesis.
Six previous case reports have described meniscal cyst formation after AI meniscal repair. Of these six cases, three underwent removal of the cyst and anchors via open excision and one underwent arthroscopic partial cystectomy, and in two cases the symptoms resolved without additional surgery [2, 5, 6, 8, 19]. Some authors have recommended arthroscopic partial meniscectomy and cyst decompression for unrepaired meniscal cysts [1, 20]. In this study, two patients underwent removal of the cyst and anchors via open excision, as arthroscopic decompression was considered insufficient because the non-absorbable anchors and sutures may have contributed to cyst formation. Intra-operatively, it was found that the anchors were located in the cyst in these cases.
A previous study reported that meniscal cysts occur after arthroscopic meniscal repair in 1.7–40.0% of cases and suggested that the risk factors for cyst formation are medial meniscal tears and the AI device use [9]. Other studies have also reported meniscal cyst formation after medial meniscal repair [2, 4, 6,7,8, 19, 21]. In this study, multivariate logistic analyses showed that the cyst formation risk significantly increased in patients with a medial meniscal tear compared with those with a lateral meniscal tear (OR = 17.2; P = 0.005). Possible reasons for cysts being more likely to occur in the medial meniscus have previously been reported [9, 13] and state the translation of the medial meniscus is smaller than that of the lateral meniscus, and the load is concentrated on the posterior segment of the medial meniscus during deep flexion [22,23,24].
The incidence of cyst formation detected on follow-up MRI after meniscal repair with AI devices is reportedly 8.0–40.0% [9, 10, 13, 25]. These cases are mostly asymptomatic or involve mild pain/effusion. Tschirch et al. [26] also reported that meniscal cysts might be present in asymptomatic knees. Cyst excision is reportedly only needed in 0–14.2% of patients with meniscal cysts because of pain and tenderness along the joint line [2, 5, 6, 8,9,10, 13, 25]. In this study, as in previous reports, cyst formation was mostly asymptomatic or involved mild symptoms, and only two patients in the O group needed cyst excision because of pain during activity (Table 1). The incidence rates of cyst formation were 26.4% and 5.56% in the O and N groups, respectively. The use of the new FasT-Fix 360 resulted in a lower incidence rate of meniscal cyst formation than that reported in previous studies, which used the old FasT-Fix [9, 10, 13, 25].
The proposed causes of meniscal cyst formation include direct contact between the meniscal cyst and an adjacent meniscal horizontal tear [27], extrusion of synovial fluid through an adjacent meniscal tear [28,29,30,31], and the pumping action of joint motion [6]. In this study, there were significantly more cyst cases in young patients. Younger patients may have higher activity levels, which may have contributed to the increased incidence of cysts. On the other hand, contrary to the previous report [27], in this study, there was no significant difference in horizontal tears between cases with and those without meniscal cysts.
Sutures and AI devices are considered to affect cyst formation [4, 7, 9, 13, 21]. Moreover, meniscal cysts after surgery using bioabsorbable implants reportedly resolve within 18 weeks [19]. Terai et al. [13] suggested that the hole created by the needle of the AI device could promote cyst formation. The new FasT-Fix 360 includes a 17-gauge needle, no. 2–0 braided polyester, and lower profile implants with diameters of 1 and 1.5 mm. However, older FasT-Fix devices include a 17-gauge needle, the suture material is no. 0 non-absorbable braided polyester, and the implant diameter is 2 mm. The size of the hole created by the use of implant is considered to be primarily affected by the implant diameter and, therefore, the implant size may affect cyst formation. In this study, the cyst formation rate was low, and the cyst size tended to be smaller in the N than in the O group. Previous case reports have described the presence of large cysts (15–30 mm) with older type implants [2, 5, 6, 8, 19], which could be attributed to the fact that the use of low-profile devices has resulted in a decreased rate of cyst formation and smaller cyst size. Moreover, the suture number of FasT-Fix was larger in cases with cysts than in those without cysts. It is considered that a larger number of used sutures may increase the chance for cyst formation with that mechanism. The other proposed causes of meniscal cyst formation after meniscal repair include soft tissue irritation with repetitive trauma by non-absorbable suture materials [3] and degeneration of the unhealed meniscus [4, 7]. In this study, there was no significant difference in meniscal healing between cases with and those without meniscal cysts.
The present study had some limitations. First, it was a retrospective cohort study; thus, it was vulnerable to bias associated with the patient background characteristics. For example, as medial meniscal repair using an AI device was found to be a risk factor for meniscal cyst formation, over time, the surgeon tended to refrain from using AI devices in such cases. Moreover, a surgeon’s skill may improve annually with experience and it could be a confounder for lower meniscal cyst formation in the N group. Second, the number of patients was relatively small. A power analysis revealed that 50 cases in each group were the minimum required sample to detect a difference of cyst formation between the N and O groups. Third, the follow-up period might have been too short to detect meniscal cyst formation. However, Terai et al. [13] reported that 15 cyst formations were observed in 12 menisci within one year post-operatively and in three menisci at two years post-operatively, suggesting that meniscal cysts are likely to occur within 1 year postoperatively. Fourth, the follow-up period was significantly shorter in the N group than in the O group because the two groups were divided by the time period. Fifth, meniscal healing was assessed using MRI rather than arthroscopy.
Conclusion
The MRI-confirmed cyst formation rate after meniscal repair was significantly lower using the new FasT-Fix 360 device rather than the older FasT-Fix devices, suggesting that use of a low-profile device may decrease the cyst formation rate.
Availability of data and materials
The data and materials of the current study are available from the corresponding author on reasonable request.
Abbreviations
- AI:
-
All-inside
- MRI:
-
Magnetic resonance imaging
- DLM:
-
Discoid lateral meniscus
- ACL:
-
Anterior cruciate ligament
- OR:
-
Odds ratios
- CI:
-
Confidence intervals
References
Lu KH (2006) Arthroscopic meniscal repair and needle aspiration for meniscal tear with meniscal cyst. Arthroscopy 22(12):1367. https://doi.org/10.1016/j.arthro.2006.04.087
Yoo JH, Yoon JR, Lee SJ (2008) Parameniscal cyst formation after arthroscopic meniscal repair with biodegradable meniscal arrow: a case report. Knee Surg Sports Traumatol Arthrosc 16(9):815–817. https://doi.org/10.1007/s00167-008-0553-7
Kang HJ, Chun CH, Kim SH, Kim KM (2012) A ganglion cyst generated by non-absorbable meniscal repair suture material. Orthop Traumatol Surg Res 98(5):608–612. https://doi.org/10.1016/j.otsr.2011.12.006
Kimura M, Hagiwara A, Hasegawa A (1993) Cyst of the medial meniscus after arthroscopic meniscal repair. Am J Sports Med 21(5):755–757. https://doi.org/10.1177/036354659302100524
Kulkarni V, Mulford J (2012) Cyst following meniscal repair. Knee Surg Sports Traumatol Arthrosc 20(11):2197–2199. https://doi.org/10.1007/s00167-011-1803-7
Lombardo S, Eberly V (1999) Meniscal cyst formation after all-inside meniscal repair. Am J Sports Med 27(5):666–667. https://doi.org/10.1177/03635465990270052001
Nagura I, Yagi M, Kokubu T, Yoshiya S, Kurosaka M (2004) Generation of meniscal cyst after arthroscopic meniscal repair. Arthroscopy 20(8):869–871. https://doi.org/10.1016/j.arthro.2004.07.008
Nakamae A, Deie M, Yasumoto M, Kobayashi K, Ochi M (2004) Synovial cyst formation resulting from nonabsorbable meniscal repair devices for meniscal repair. Arthroscopy 20(2):16–19. https://doi.org/10.1016/j.arthro.2004.04.014
Nishino K, Hashimoto Y, Nishida Y, Terai S, Takahashi S, Yamasaki S, Nakamura H (2019) Incidence and risk factors for meniscal cyst after meniscal repair. Arthroscopy 35(4):1222–1229. https://doi.org/10.1016/j.arthro.2018.11.039
Choi NH, Kim BY, Hwang Bo BH, Victoroff BN (2014) Suture versus FasT-Fix all-inside meniscus repair at time of anterior cruciate ligament reconstruction. Arthroscopy 30(10):1280–1286. https://doi.org/10.1016/j.arthro.2014.05.023
Seo SS, Kim CW, Lee CR, Park DH, Kwon YU, Kim OG, Kim CK (2020) Second-look arthroscopic findings and clinical outcomes of meniscal repair with concomitant anterior cruciate ligament reconstruction: comparison of suture and meniscus fixation device. Arch Orthop Trauma Surg 40(3):365–372. https://doi.org/10.1007/s00402-019-03323-3
Grant JA, Wilde J, Miller BS, Bedi A (2012) Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med 40(2):459–468. https://doi.org/10.1177/0363546511411701
Terai S, Hashimoto Y, Yamasaki S, Takahashi S, Shimada N, Nakamura H (2019) Prevalence, development, and factors associated with cyst formation after meniscal repair with the all-inside suture device. Arch Orthop Trauma Surg 139(9):1261–1268. https://doi.org/10.1007/s00402-019-03176-w
Haas AL, Schepsis AA, Hornstein J, Edgar CM (2005) Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy 21(2):167–175. https://doi.org/10.1016/j.arthro.2004.10.012
Kocabey Y, Chang HC, Brand JC Jr, Nawab A, Nyland J, Caborn DN (2006) A biomechanical comparison of the FasT-Fix meniscal repair suture system and the RapidLoc device in cadaver meniscus. Arthroscopy 22(4):406–413. https://doi.org/10.1016/j.arthro.2005.12.009
Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH (2006) Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy 22(1):3–9. https://doi.org/10.1016/j.arthro.2005.10.017
Popescu D, Sastre S, Caballero M, Lee JW, Claret I, Nuñez M, Lozano L (2010) Meniscal repair using the FasT-Fix device in patients with chronic meniscal lesions. Knee Surg Sports Traumatol Arthrosc 18(4):546–550. https://doi.org/10.1007/s00167-009-0926-6
McCauley TR (2005) MR imaging evaluation of the postoperative knee. Radiology 234(1):53–61
Tingstad EM, Teitz CC, Simonian PT (2001) Complications associated with the use of meniscal arrows. Am J Sports Med 29(1):96–98. https://doi.org/10.1177/03635465010290012201
Erginer R, Yücel I, Oğüt T, Kesmezacar H, Babacan M (2004) Medial meniscus anterior horn cyst: arthroscopic decompression. Arthroscopy 20(2):9–12. https://doi.org/10.1016/j.arthro.2004.04.006
Choi NH, Kim SJ (2004) Meniscal cyst formation after inside-out meniscal repair. Arthroscopy 20(1):E1-3. https://doi.org/10.1016/j.arthro.2003.11.020
Thompson WO, Thaete FL, Fu FH, Dye SF (1991) Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med 19(3):210–216. https://doi.org/10.1177/036354659101900302
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br 81(1):37–41. https://doi.org/10.1302/0301-620x.81b1.8928
Yao J, Lancianese SL, Hovinga KR, Lee J, Lerner AL (2008) Magnetic resonance image analysis of meniscal translation and tibio-menisco-femoral contact in deep knee flexion. J Orthop Res 26(5):673–684. https://doi.org/10.1002/jor.20553
Hoffelner T1, Resch H, Forstner R, Michael M, Minnich B, Tauber M (2011) Arthroscopic all-inside meniscal repair–does the meniscus heal? A clinical and radiological follow-up examination to verify meniscal healing using a 3-T MRI Skeletal Radiol 40(2):181-187https://doi.org/10.1007/s00256-010-0965-6
Tschirch FT, Schmid MR, Pfirrmann CW, Romero J, Hodler J, Zanetti M (2003) Prevalence and size of meniscal cysts, ganglionic cysts, synovial cysts of the popliteal space, fluid-filled bursae, and other fluid collections in asymptomatic knees on MR imaging. AJR Am J Roentgenol 180(5):1431–1436. https://doi.org/10.2214/ajr.180.5.1801431
Campbell SE, Sanders TG, Morrison WB (2001) MR imaging of meniscal cysts: incidence, location, and clinical significance. AJR Am J Roentgenol 177:409–413. https://doi.org/10.2214/ajr.177.2.1770409
De Smet AA, Graf BK, del Rio AM (2011) Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. AJR Am J Roentgenol 196(2):W180–W186. https://doi.org/10.2214/ajr.10.4754
Barrie HJ (1979) The pathogenesis and significance of meniscal cysts. J Bone Joint Surg Br 61(2):184–189. https://doi.org/10.1302/0301-620x.61b2.582035
Tasker AD, Ostlere SJ (1995) Relative incidence and morphology of lateral and medial meniscal cysts detected by magnetic resonance imaging. Clin Radiol 50(11):778–781. https://doi.org/10.1016/s0009-9260(05)83219-2
Tyson LL, Daughters TC Jr, Ryu RK, Crues JV 3rd (1995) MRI appearance of meniscal cysts. Skeletal Radiol 24(6):421–424. https://doi.org/10.1007/bf00941237
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Takuya Kinoshita, Yusuke Hashimoto, Kazuya Nishino, Yohei Nishida, Shinji Takahashi, and Hiroaki Nakamura. The first draft of the manuscript was written by Takuya Kinoshita and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the hospital ethics committee and the internal review board of our institution (3071).
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kinoshita, T., Hashimoto, Y., Nishino, K. et al. Comparison of new and old all-inside suture devices in meniscal cyst formation rates after meniscal repair. International Orthopaedics (SICOT) 46, 1563–1571 (2022). https://doi.org/10.1007/s00264-022-05375-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05375-4