Abstract
Purpose
Though numerous studies highlighted benefits of ambulatory total joint arthroplasty (TJA), most had selected patients with age and comorbidities thresholds. We aimed to report proportions of unselected TJAs that could be scheduled for and operated in ambulatory settings, and to determine factors that hinder same-day discharge (SDD).
Methods
We studied 1100 consecutive primary TJAs (644 THAs and 456 TKAs) that were prepared following a multidisciplinary protocol for patient education and logistical preparation. Data were stratified for THA vs TKA and for success vs failure of SDD to home and multivariable analysis was performed to determine factors associated with failure of scheduled SDD to home.
Results
In total, 860 (78.2%) were scheduled for ambulatory surgery, but only 819 (74.5%) achieved SDD to home; 240 (21.8%) were scheduled for non-ambulatory surgery, but 103 (9.3%) achieved SDD to rehabilitation centre. Re-operations were required in 9 (1.0%) ambulatory TJAs vs 2 (0.8%) non-ambulatory TJAs (p = 0.769), while revisions were required in 13 (1.5%) ambulatory TJAs vs 1 (0.4%) non-ambulatory TJAs (p = 0.181). Multivariable analysis confirmed that failure of SDD to home was greater for women (OR 2.59; p = 0.011) and THA (vs TKA, OR 2.41; p = 0.023).
Conclusion
With appropriate education and preparation, 75% of unselected primary hip and knee arthroplasties achieved SDD to home without compromising risks of complications, re-operations, or revisions. A further 9% achieved SDD to rehabilitation centre, implying that 84% of patients did not require overnight stay. These findings suggest that ambulatory surgery is feasible and safe to implement in most unselected lower limb arthroplasties.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total joint arthroplasty (TJA) is increasingly performed in fast-track and ambulatory settings [1], with proven patient safety and cost savings when compared to conventional hospitalization [2,3,4]. Beyond economic benefits, ambulatory TJA has the potential advantages of early mobilization and quicker return to normal living environment [5], which could reduce thromboembolisms, opioid consumption, and mental confusion [2, 6, 7]. And while fast-track and ambulatory surgery were originally intended for younger patients with little or no comorbidities, some studies suggested that elderly patients have the most to gain from rapid recovery programs after TJA [8].
One of the key factors for success of fast-track and ambulatory TJA is the multidisciplinary approach to accelerate clinical pathways [9, 10], which includes extensive pre-operative patient education, physical and logistical preparation [11,12,13], and early rehabilitation and physical therapy [4]. At our private hospital, the proportions of ambulatory total hip arthroplasty (THA) and total knee arthroplasty (TKA) increased considerably in recent years thanks to the implementation of a dedicated protocol for patient preparation, which comprises a detailed pre-operative assessment of medical comorbidities and logistical considerations. The protocol also includes sessions with anesthesiologists, physiotherapists, and discharge nurses, who help patients prepare and optimize their pre- and peri-operative conditions at home.
The primary goal of the present study was to report the proportion of unselected lower limb TJA patients that could be scheduled for and effectively operated in ambulatory settings following the aforementioned protocol for patient preparation. The secondary goals were to determine factors that hinder scheduled same-day discharge (SDD) to home and to compare 90-day complication rates of ambulatory THA and TKA. The hypotheses were that the majority of procedures would be successfully performed in ambulatory settings, and that neither the factors that hinder SDD to home nor complication rates differ among THA and TKA.
Material and methods
The authors retrospectively analyzed the records of 1114 consecutive primary lower limb TJA procedures (657 THAs and 457 TKAs) performed between April 2018 and December 2020, by three experienced surgeons (BLINDED) at the same center. The authors excluded 13 THA cases operated for femoral neck fractures and one TKA case that had prior knee arthrodesis, but included all other indications of primary and secondary osteoarthritis (OA) and osteonecrosis, which left a study cohort of 1100 TJAs (644 THAs and 456 TKAs). For each patient, the pre-operative case notes were consulted to record age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) score, indication for surgery, and any medical comorbidities (cardiovascular, respiratory, diabetes, renal, or other), allergies (medicinal, metallic, dietary, or other), pre-operative anticoagulant regimen, and smoking habits (Table 1).
All patients followed a dedicated protocol for patient preparation, which started 30 days prior to surgery by consultation with the surgeon, routine laboratory tests, and provision of formal documents and educational booklet as well as scheduling appointments with dentists and home nurses. Prehabilitation exercises were supervised by physiotherapists for 30 days prior to TKA (but not THA). Preoperative evaluation 15 days before surgery, including radiographic imaging, cardiac assessment, and nasal swabs, as well as consultations with the anesthesiologist, physiotherapist, and discharge nurse, to help patients prepare and optimize their pre- and peri-operative home environment. Skin preparation was required three days before surgery using hair removal cream or electric shavers. Patients were reminded the day before surgery to remove any accessories, make-up, etc., and to prepare all necessary documents, radiographs, crutches, and compressive socks, as well as appropriate clothes and toiletries.
-
A total of 860 TJAs were scheduled for ambulatory surgery with SDD to home (530 THAs and 330 TKAs). The remaining 240 TJAs (114 THAs and 126 TKAs) were scheduled for non-ambulatory surgery due to logistical or medical reasons identified by the anesthesiologist during pre-operative consultation on a patient-by-patient basis. There were otherwise no predefined criteria related to age, BMI, or ASA score for patient allocation to non-ambulatory surgery. The non-ambulatory TJAs were scheduled as follows: 106 for SDD to a rehabilitation centre (52 THAs and 54 TKAs), all due to logistical reasons, namely patient living alone or with insufficient support at home;
-
134 with a hospital stay of one or more nights (62 THAs and 72 TKAs): 44 due to medical reasons (22 THAs and 22 TKAs) such as severe cardiovascular or systemic comorbidities (notably unstable diabetes and chronic respiratory disease), and 90 due to logistical reasons (40 THAs and 50 TKAs), mainly due to unavailability of space at a rehabilitation centre (n = 59), as well as patient refusal (n = 9), surgery performed during the afternoon (n = 6), patient living more than two hours away from hospital (n = 8) or living alone (n = 3), and reason unspecified (n = 5).
For each patient, the length of stay (LOS) at hospital, discharge destination (home or rehabilitation centre), and 90-day complications and revisions were recorded.
Statistical analysis
Descriptive statistics were used to summarize the data. The Shapiro–Wilk tests were used to assess the normality of distributions. For non-Gaussian quantitative data, differences between groups were evaluated using Wilcoxon’s rank sum tests (Mann–Whitney’s U test). For non-Gaussian categorical data, differences between groups were evaluated using Fisher’s exact tests. Uni- and multivariable logistic regression analyses were performed to determine whether failure of scheduled SDD to home was associated with 15 independent pre-operative variables: operated joint (hip vs knee), age, sex, BMI, ASA score, medical comorbidities (cardiovascular, respiratory, diabetes or renal), allergies (medicinal, metallic, dietary or other), anticoagulant regimen and smoking habits. P values < 0.05 were considered statistically significant. Statistical analyses were performed using R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
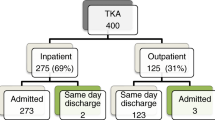
From the study cohort of 1100 primary TJAs, 860 (78.2%) were scheduled for ambulatory surgery, though SDD to home was effectively achieved for only 819 (74.5%) (Fig. 1). It is worth noting that, of the 240 (21.8%) TJAs that were not scheduled for ambulatory surgery due to medical or logistical reasons, SDD to a rehabilitation center was nonetheless achieved for 103 (9.3%) of the original 106 (9.6%) (Table 1).
Of the 860 TJAs scheduled for ambulatory surgery, 25 (2.9%) had complications that were treated conservatively, while nine (1.0%) required re-operation without implant removal and 13 (1.5%) required revision (Table 2). By contrast, of the 240 patients that were not scheduled for ambulatory surgery, four (1.7%) had complications that were treated conservatively, while only two (0.8%) required reoperation without implant removal, and only one (0.4%) required revision. Neither the difference in complication rate (p = 0.289), reoperation rate (p = 0.769), nor revision rate (p = 0.181) was statistically significant.
Compared to the 819 TJAs that had SDD to home, the 41 that failed SDD to home and spent one or more nights at hospital had slightly higher age (68 vs 67 years, p < 0.001), BMI (28 vs 27, p < 0.001), and proportion of THAs (75.6% vs 60.9%, p = 0.007) (Table 3). The reasons for failure of scheduled SDD to home were dizziness/nausea due to hypotension or intolerance to pain killers (n = 14), inadequate pain control (n = 10), cardiovascular incidents (n = 7), transfusion required (n = 3), urinary retention (n = 3), neuromuscular deficit (n = 3), and operation time longer than expected (n = 1).
Comparing THA versus TKA, the proportion of patients scheduled for ambulatory surgery among the study cohort was higher for THA (82.3% vs 72.4%, p < 0.001), but the rate of failure of scheduled SDD to home was lower for TKA (4.8% vs 2.2%, p = 0.061) (Table 1). Among those scheduled for ambulatory surgery, THA patients had significantly lower age, BMI, ASA score and proportions of women, primary OA, and diabetes, but more smokers, compared to TKA patients (Table 2). There were however no significant differences between THAs and TKAs regarding rates of complications (p = 0.279), re-operations (p = 0.706), or revisions (p = 0.254).
Univariable logistic regression revealed that failure of scheduled SDD to home was only greater for women (OR 1.96; p = 0.045) and patients with medicinal allergies (OR 2.12; p = 0.035). Multivariable logistic regression confirmed that failure of scheduled SDD to home was more than twice greater for women (OR 2.59; p = 0.011) as well as for THA compared to TKA (OR 2.41; p = 0.023) (Table 4).
Discussion
The main findings of the present study are that, with appropriate patient education, selection, and preparation, up to 74.5% of unselected primary lower limb TJAs were operated in ambulatory settings with SDD to home, without compromising their risks of complications, re-operations, or revisions. This success rate is a result of collaborative teamwork between anesthesiologists, surgeons, nurses, and physiotherapists, who ensure adequate pre-operative logistics and post-operative pain management. It is worth noting that a further 9.3% achieved SDD to a rehabilitation centre, implying that 83.8% of the study cohort did not require overnight hospital stay. Furthermore, multivariable analysis revealed that failure of scheduled SDD to home is twice more likely for women and for THA (compared to men and TKA), though there were no significant differences between THAs and TKAs regarding rates of complications, re-operations, or revisions. The present findings therefore confirm the first hypothesis that the majority of TJAs could be performed in ambulatory settings, but refute the second hypothesis that factors which hinder SDD to home or increase complications do not differ among THA and TKA.
In the present series of lower limb TJAs, the overall rate of failure of scheduled SDD to home was 3.7%, which compares favourably to a recent systematic review on the safety of outpatient arthroplasty by Jaibaji et al.[14], which reported failure of SDD to home in 0.5 to 24%. It is important to note that the studies included by Jaibaji et al.[14] were on average much smaller cohorts of selected patients, most of them with cutoffs of age, BMI, and ASA score. The same systematic review specified that the most frequent reasons were nausea/dizziness, inadequate pain control, hypotension, and urinary retention. Our data corroborate these findings, as the most common reasons for failure of scheduled SDD to home were also dizziness/nausea (n = 14), pain (n = 10), cardiovascular incidents (n = 7), and urinary retention (n = 3), as well as transfusion required (n = 3), neuromuscular deficit (n = 3), and operation time longer than expected (n = 1).
In the present series, complications treated conservatively occurred in 2.9% of ambulatory TJAs vs 1.7% of non-ambulatory TJAs (p = 0.289), re-operations were required in 1.0% of ambulatory TJAs vs 0.8% of non-ambulatory TJAs (p = 0.769), while revisions were required in 1.5% of ambulatory TJAs vs 0.4% of non-ambulatory TJAs (p = 0.325). The most common reasons for reoperation and revision were sepsis, periprosthetic fractures, and hip dislocation. The systematic review of Jaibaji et al.[14] reported 90-day readmission rate of 0.9 to 11.4% and 90-day re-operation rates of 0.8 to 4%. In another recent study, Liu et al.[15] concluded that SDD after TKA and THA was associated with higher odds of cardiac/pulmonary complications compared with patients who had an overnight stay in hospital, and concluded that the overall burden of complications is relatively low but a measured approach is advisable when recommending SDD > until future studies can confirm or challenge our findings.
The present series revealed that failure of scheduled SDD to home is twice more likely for women and for THA (compared to men and TKA), but that rates of complications, re-operations, or revisions did not differ among THA and TKA. Our findings are in contrast with a recent meta-analysis of Shah et al. [1], who concluded that length of stay in hospital increased with age, female gender, BMI > 30, non-White race, American Society of Anesthesiologists > 2, Charlson Comorbidity Index > 0, and pre-operative haemoglobin < 130 g/L. In another study focused on psychological aspects, March et al.[16] concluded that poor mental health could increase hospital length of stay after TKA, but neither the size nor the clinical importance of this effect could be determined from their data.
Ambulatory surgery can save costs of hospital stay to both patients and insurers, whether public or private, but it is important to note that it incurs extra costs to clinics and hospitals for patient education and logistical preparation [17]. The benefits of ambulatory surgery include early mobilization and quicker return to normal living conditions [5, 18], which should improve patient physical and mental health. The economic and health benefits of ambulatory TJA should also be weighed against the risks of unexpected hospital readmissions, especially to emergency departments as previous studies reported that up to 10% of patients are readmitted within 90 days of TJA [19].
In the present series, the proportion of patients allocated for ambulatory surgery was greater for THA than TKA procedures (respectively, 82% and 72%), possibly because THA is historically perceived as simpler and less complicated than TKA [2], and because ambulatory THA started a few years earlier than ambulatory TKA at our center. The rate of failure of scheduled SDD to home was however twice greater for THA than TKA (respectively, 4.8% and 2.2%), suggesting that patient allocation to ambulatory surgery was more prudent for TKA than for THA. In effect, THA is a more invasive operation than TKA, as it involves greater blood loss and muscle damage, both of which could lead to hypotension and subsequent dizziness/nausea, unexpected pain, and cardiovascular incidents. While hypotension due to blood loss or intolerance to medication is more difficult to predict, pain management could be enhanced, though increasing analgesic dosage must be done with caution as it can increase side effects. Our multivariable analysis also confirmed that women have twice the odds of failure of scheduled SDD to home, which is consistent with the findings of Shah et al.[1]. It remains unclear whether this is because women are more likely to have nausea/dizziness, pain, or cardiovascular incidents, or if gender roles in this age group.
It is worth noting that even if previous published studies demonstrated the safety and feasibility of ambulatory lower limb TJA, certain limitation of infrastructure limitations and societal preconceptions can still hinder its implementation. The main examples are the proportions of patients that could have had SDD to rehabilitation centre but stayed one or more nights at hospital because of unavailability of space at a rehabilitation centre, as well as patients that were kept in hospital simply because they refused SDD to home or rehabilitation. Moreover, with the aging population and cultural trends, the proportion of patient living alone or with insufficient support at home is likely to increase, and the healthcare system should anticipate such barriers, to enable safe SDD of TJA patients (e.g., availability of doctor in emergency situations, having sufficient home support for wound care, and monitoring haemoglobin levels on the second day).
The present study has a number of limitations that must be considered when interpreting its findings. First, its retrospective design does not allow confirmation of cause and effect relationships between allocation to ambulatory surgery and failure of scheduled SDD to home. Second, the authors did not quantify post-operative consumption of opioids and other medication, to ascertain that the benefits of returning to home are not offset by drawbacks of taking more pain killers. Third, the authors did not collect patient-reported outcomes nor subjective satisfaction, which would have helped confirm the benefits of early mobilization and quicker return to normal living conditions. Nevertheless, the strengths of this study include its sizeable cohort of unselected patients, with sufficient demographic and preoperative data, which enabled multivariable analysis of independent factor associated with failure of scheduled SDD to home.
Conclusion
With appropriate patient education and logistical preparation, up to 75% of unselected primary lower limb TJAs were operated in ambulatory settings with SDD to home, without compromising their risks of complications, re-operations, or revisions. A further 9% achieved SDD to a rehabilitation centre, implying that 84% of the study cohort did not require overnight hospital stay. The present study therefore suggests that, through synergies between anesthesiologists, surgeons, nurses, and physiotherapists, ambulatory surgery is feasible and safe in the majority of unselected lower limb TJAs, but that prudent allocation is important to ensure adequate preoperative logistics and post-operative pain management.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The custom code used for the current study is available from the corresponding author on reasonable request.
References
Shah A, Memon M, Kay J, Wood TJ, Tushinski DM, Khanna V (2019) Preoperative patient factors affecting length of stay following total knee arthroplasty: a systematic review and meta-analysis. The Journal of arthroplasty 34:2124-2165. e2121. https://doi.org/10.1016/j.arth.2019.04.048
Larsen JR, Skovgaard B, Pryno T, Bendikas L, Mikkelsen LR, Laursen M, Hoybye MT, Mikkelsen S, Jorgensen LB (2017) Feasibility of day-case total hip arthroplasty: a single-centre observational study. Hip Int 27:60–65. https://doi.org/10.5301/hipint.5000421
Petersen PB, Kehlet H, Jørgensen CC (2020) Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci Rep 10:21233. https://doi.org/10.1038/s41598-020-77127-6
Pollock M, Somerville L, Firth A, Lanting B (2016) Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev 4. https://doi.org/10.2106/JBJS.RVW.16.00002
Moyer R, Ikert K, Long K, Marsh J (2017) The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 5:e2. https://doi.org/10.2106/JBJS.RVW.17.00015
Harsten A, Kehlet H, Ljung P, Toksvig-Larsen S (2015) Total intravenous general anaesthesia vs. spinal anaesthesia for total hip arthroplasty: a randomised, controlled trial. Acta Anaesthesiol Scand 59:298–309. https://doi.org/10.1111/aas.12456
Harsten A, Kehlet H, Toksvig-Larsen S (2013) Recovery after total intravenous general anaesthesia or spinal anaesthesia for total knee arthroplasty: a randomized trial. Br J Anaesth 111:391–399. https://doi.org/10.1093/bja/aet104
Starks I, Wainwright TW, Lewis J, Lloyd J, Middleton RG (2014) Older patients have the most to gain from orthopaedic enhanced recovery programmes. Age Ageing 43:642–648. https://doi.org/10.1093/ageing/afu014
Koksal I, Tahta M, Simsek ME, Dogan M, Bozkurt M (2015) Efficacy of rapid recovery protocol for total knee arthroplasty: a retrospective study. Acta Orthop Traumatol Turc 49:382–386. https://doi.org/10.3944/AOTT.2015.14.0353
Yanik JM, Bedard NA, Hanley JM, Otero JE, Callaghan JJ, Marsh JL (2018) Rapid recovery total joint arthroplasty is safe, efficient, and cost-effective in the veterans administration setting. J Arthroplasty 33:3138–3142. https://doi.org/10.1016/j.arth.2018.07.004
Jørgensen CC, Gromov K, Petersen PB, Kehlet H (2020) Influence of day of surgery and prediction of LOS > 2 days after fast-track hip and knee replacement. Acta orthopaedica:1–6. https://doi.org/10.1080/17453674.2020.1844946
Gillis ME, Dobransky J, Dervin GF (2019) Defining growth potential and barriers to same day discharge total knee arthroplasty. Int Orthop 43:1387–1393. https://doi.org/10.1007/s00264-018-4100-y
Paredes O, Nunez R, Klaber I (2018) Successful initial experience with a novel outpatient total hip arthroplasty program in a public health system in Chile. Int Orthop 42:1783–1787. https://doi.org/10.1007/s00264-018-3870-6
Jaibaji M, Volpin A, Haddad FS, Konan S (2020) Is outpatient arthroplasty safe? A systematic review. J Arthroplasty 35:1941–1949. https://doi.org/10.1016/j.arth.2020.02.022
Liu J, Elkassabany N, Poeran J, Gonzalez Della Valle A, Kim DH, Maalouf D, Memtsoudis S (2019) Association between same day discharge total knee and total hip arthroplasty and risks of cardiac/pulmonary complications and readmission: a population-based observational study. BMJ Open 9:e031260. https://doi.org/10.1136/bmjopen-2019-031260
March MK, Harmer AR, Dennis S (2018) Does psychological health influence hospital length of stay following total knee arthroplasty? A systematic review. Arch Phys Med Rehabil 99:2583–2594. https://doi.org/10.1016/j.apmr.2018.03.020
Büttner M, Mayer AM, Büchler B, Betz U, Drees P, Susanne S (2020) Economic analyses of fast-track total hip and knee arthroplasty: a systematic review. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie 30:67–74. https://doi.org/10.1007/s00590-019-02540-1
Deng QF, Gu HY, Peng WY, Zhang Q, Huang ZD, Zhang C, Yu YX (2018) Impact of enhanced recovery after surgery on postoperative recovery after joint arthroplasty: results from a systematic review and meta-analysis. Postgrad Med J 94:678–693. https://doi.org/10.1136/postgradmedj-2018-136166
Maldonado-Rodriguez N, Ekhtiari S, Khan MM, Ravi B, Gandhi R, Veillette C, Leroux T (2020) Emergency department presentation after total hip and knee arthroplasty: a systematic review. J Arthroplasty 35(3038–3045):e3031. https://doi.org/10.1016/j.arth.2020.05.022
Acknowledgements
The authors are grateful to ELSAN for funding study design, statistical analysis, and manuscript preparation and to LENSYS for their software Direct Consult for data collection and management. The authors would also like to thank Mrs. Aude Hibon for her support with project management.
Author information
Authors and Affiliations
Contributions
NV: study design, data collection, manuscript editing.
BB: study design, data collection, manuscript editing.
PR: study design, data collection, manuscript editing.
PL: study design, data collection, manuscript editing.
MS: study design, literature review, manuscript writing.
LN: literature review, statistical analysis, manuscript writing.
JM: study design, data collection, manuscript editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Given that the study was performed using a pre-existing database, approval of the institutional review board was not required. All patients provided informed consent for the use of their data for research and publications.
Consent for publication
All patients gave written consent for the use of their data and images for research and publication purposes.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Verdier, N., Boutaud, B., Ragot, P. et al. Same-day discharge to home is feasible and safe in up to 75% of unselected total hip and knee arthroplasty. International Orthopaedics (SICOT) 46, 1019–1027 (2022). https://doi.org/10.1007/s00264-022-05348-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05348-7