Abstract
Introduction
Avascular necrosis (AVN) after femoral neck fracture (FNF) is a rare and severe paediatric condition, but only few studies described its prognosis and risk factors. The present study aimed to evaluate the outcomes and independent factors for poor prognosis of AVN after FNF in children and adolescents.
Method
This retrospective study included children and adolescents with AVN after FNF who received conservative treatment (CT group) or non-vascularized bone grafting (NVBG group) between 2000 and 2018. The primary outcomes were the risk of hip arthritis (Tönnis grade) and hip deformity risk (Stulberg classification). All patients were followed for at least two years to assess AVN progression.
Results
Study included 81 patients. In the CT group, 23/43 patients (53.4%) developed hip arthritis, and 24/43 patients (55.8%) showed hip deformity. In the NVBG group, 23/38 patients (60.5%) developed hip arthritis, and 34/38 patients (89.5%) had a hip deformity. The multivariable analysis indicated that NVBG surgery had no significant effect on the outcomes. Post-treatment femoral head collapse (P = 0.05, OR = 3.80, 95% CI = 1.01–14.29) and post-treatment hip subluxation (P = 0.01, OR = 2.85, 95% CI = 2.31–129.56) were independent risk factors for severe hip arthritis. Post-treatment femoral head collapse (P < 0.01, OR = 7.64, 95% CI = 3.23–18.04) and pre-treatment hip subluxation (P = 0.02, OR = 7.33, 95% CI = 1.44–37.41) were independent risk factors for severe hip deformity.
Conclusion
Neither CT nor NVBG have demonstrated superiority regarding long-term outcomes in patients with AVN after FNF. Upon the disease progression to severe collapse with subluxation and severe arthritis, further hip preservation attempts could be futile.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoral neck fracture (FNF) in children and adolescents is mostly caused by high-energy trauma and has an incidence of less than 1% [1, 2]. Due to the immature blood supply, FNF can result in extensive avascular necrosis (AVN) of the proximal femur [1, 2]. Extensive AVN involving the entire femur head is the most common pattern [3], representing 51.7–80.8% of the cases and often leading to the poorest outcomes [1, 2, 4, 5]. Conservative management of AVN includes physical therapy, restricted weight-bearing, discontinuation of steroids, pain control, and targeted pharmacological interventions [6,7,8,9,10,11,12]. Invasive management includes core decompression, bone grafts, biological and/or cellular therapies, osteotomy, and reconstruction [6, 13,14,15].
Upon admittance most children and adolescents with AVN after FNF show various degrees of collapse or deformity of the femoral head as well as hip subluxation [1, 2]. The short-term prognosis of such patients is poor, and progress to severe hip degeneration is not uncommon. Due to the rarity of AVN after FNF, only a few studies have compared the conservative or surgical treatments in children and adolescents with AVN after FNF, with conflicting results [16,17,18].
Based on the above, this retrospective study aimed to examine the specific characteristics and prognosis of children and adolescents with AVN after FNF, examine whether non-vascularized bone grafting can improve the short-term (arthritis) and long-term (deformity) outcomes, and investigate the independent factors for poor prognosis in children and adolescents with AVN after FNF.
Material and methods
Study design
This retrospective study used a database of out- and inpatient clinical and radiographic information. The study was approved by the ethics committee of the hospital. The requirement for individual consent was waived by the committee.
The diagnosis of AVN was based on the Japanese Investigation Committee (JIC) classification system [19] and the Association Research Circulation Osseous staging system [20]. The inclusion criteria were (1) < 16 years of age when trauma-induced FNF occurred, (2) no history of corticosteroid use or alcohol abuse, (3) treated conservatively or surgically, (4) followed until skeletal maturity, and (5) follow-up of ≥ two years. The exclusion criteria were (1) other complications of FNF (such as nonunion or infection) or other diseases (such as dysplasia of the hip joint or rheumatoid arthritis), (2) epiphysiolysis capitis femoris, (3) missing clinical and radiographic data, or (4) history of treatments at other hospitals.
The decision to perform surgery was made according to the presence of progressive femoral head collapse. Patients without progressive femoral head collapse received conservative treatments (CT group), while patients with progressive femoral head collapse underwent non-vascularized bone grafting (NVBG group).
Examinations
Radiographic assessment was performed with standard anteroposterior and frog-lateral radiographs. Magnetic resonance imaging (MRI) was not used routinely due to the distorted images resulting from internal metal fixation. The AVN stage (I/II/III) was determined according to the Association Research Circulation Osseous (ARCO) staging system [20]. The degree of collapse was also evaluated by the concentric circle method on anteroposterior and lateral radiographs using ImageJ (1.52a, National Institutes of Health, Bethesda, MD, USA) [21]. Pre- and post-treatment hip subluxation was defined as a break in Shenton’s line [22].
The Japanese Investigation Committee (JIC) classification system [19] was used to describe necrotic lesions and femoral head collapse, according to the following criteria: for type C, the necrotic lesions occupy more than the medial two-thirds of the weight-bearing portion; for type C2, lesions extend laterally to the acetabular edge and show a higher risk of collapse than type C1 lesions [19]. In this study, all lesions were type A, B, C1, or C2.
Management
As per routine practice at the authors’ center, conservative management was suggested to patients in the pre-collapse or mild collapse stage. The decision to perform surgery was made in cases of progressive femoral head collapse. Non-vascularized bone grafting was used to reconstruct the collapsed femoral head using the Phemister [23] technique in six cases, lightbulb [24] technique in six cases, and trapdoor [25, 26] technique in 26 cases. Combined containment surgeries, such as extensive pelvic osteotomy [27] or Chiari pelvic osteotomy [28], were performed in 13 and two cases, respectively, and aimed at rectifying the hip joint subluxation. After surgery, restricted weight-bearing was maintained with the use of crutches during the first six months. For the following 6 months, partial weight-bearing using one crutch was recommended. Then, full weight-bearing was allowed when the patients were free of hip pain. Anti-osteoporosis drugs were not used because of the unknown complications and safety in children and adolescents. Symptomatic treatments consisted of nonsteroidal anti-inflammatory drugs (NSAIDs) or analgesics, as needed. Conservative treatment only consisted of pain relief, restricted weight-bearing (6 months bilateral, 6 months unilateral, for the same duration as in surgery patients), and physical treatment, within the first two years after diagnosis of AVN.
Outcomes
The outcomes were evaluated using the Tönnis grade [29] and the Stulberg classification [30]. Tönnis grade 0 indicated the absence of degenerative changes; grade 1, mild joint-space narrowing, mild sclerosis evidenced by the widening of the sclerotic zone, and small marginal osteophytes; grade 2, moderate joint-space narrowing, moderate sclerosis of the femoral head or acetabulum, and the presence of small subchondral cysts within the femoral head or acetabulum; grade 3, severe joint-space narrowing (< 1 mm) or obliteration of the joint space and evidence of large subchondral cysts on the femoral head or acetabulum. The Stulberg classification [30] was used to describe the femoral head’s shape at skeletal maturity and to predict the long-term outcome. Class I/II hips still maintain a spherical femoral head. Class III hips have an ovoid femoral head. Class IV/V hips demonstrated a flattened femoral head.
The secondary outcome was the progression of the femoral head collapse [30]. The assessments of radiographic factors and outcomes were conducted by two specialists in paediatric joint surgery (Z.L. and Q.W.).
Follow-up
AVN progression was assessed during the follow-up. The occurrence and progression of collapse were determined by direct radiography with the hip joint in the orthotopic and frog positions. The patients were required to return to the outpatient department for imaging follow-up every three to four months for one year after surgery, every six months in the second year, and then yearly until skeletal maturity.
Statistical analysis
The continuous variables were evaluated using the Kolmogorov–Smirnov test. Those with a normal distribution are presented as means ± standard deviation and were analyzed using Student’s t test; otherwise, there are presented as medians (interquartile ranges (IQR)) and were analyzed using the Mann–Whitney U test. Categorical data are presented as n (%) and were analyzed using Fisher’s exact test or the chi-square test. Binary logistic regression models were used to examine the potential variables associated with poor prognosis. The univariable analyses were conducted using the input mode, and the multivariable analysis was performed using the forward condition. P values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS 22.0 (IBM, Armonk, NY, USA).
Results
Characteristics of patients
Between January 2000 and January 2018, 115 children and adolescents with AVN after FNF were treated at the authors’ hospital, and of them 81 were included into the study (Table 1). There were 54 boys and 27 girls, with a mean age at the time of FNF being 13.3 ± 1.9 years old (ranged from 6 to 16 years). All patients were diagnosed with AVN 13.7 ± 10.2 months after FNF. The mean follow-up time was 56.8 ± 38.4 months. Forty-three patients received conservative treatment (CT group), with a mean follow-up of 57.0 ± 40.0 months. Thirty-eight patients underwent NVBG, including 23 who underwent NVBG only and 15 who underwent NVBG with additional containment surgery. The last follow-up was at 56.7 ± 37.1 months after surgery. No significant difference of age, follow-up duration, sex, and pathogenic site was found between the two groups (P > 0.05). More patients were symptomatic in NVBG group (69.0%) than those in CT group (31.0%) (P < 0.01).
Prognosis of children and adolescents with AVN after FNF
Upon admission, 24 patients were in the pre-collapse stage (ARCO stage II), and 19 patients had progressed to the collapse stage (12 with stage IIIA, three with IIIB, and four with IIIC) in the CT group. Among the patients in the collapse stage, four had hip subluxation. During follow-up, 21 of the 43 patients in the CT group displayed a progression of the femoral head collapse, and 28 of 43 cases were in the collapse stage. Among the patients in the collapse stage, 11 had hip subluxation after treatment (Fig. 1 and Table 1).
A 13-year-old girl with a left femoral neck fracture in the conservative treatment group. A Pre-operative anteroposterior radiograph in December 2006. B Avascular necrosis (JIC C2, ARCO II) was diagnosed in June 2008. C–D Anteroposterior radiograph at 14 months of follow-up after conservative treatment, showing the development of severe collapse (> 4 mm) and severe degenerative changes (Tönnis grade 3)
Among the patients in the CT group, 55.8% showed various degrees of hip deformity. At skeletal maturity, 19 patients were defined as Stulberg type I/II, 13 type III, and 11 type IV/V. Finally, 53.5% of the patients in the CT group manifested various degrees of hip arthritis. At the last follow-up, 13, 9, and one patients were Tönnis grades I, II, and III, respectively (Fig. 1 and Table 1).
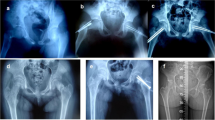
Among the patients who underwent surgery (NVBG group), only one patient was still in the pre-collapse stage (ARCO stage II), and 37 patients were in the collapse stage (eight in stage IIIA, seven in IIIB, and 22 in stage IIIC). The ARCO stage in NVBG group before treatment, and the JIC classification were significantly different from those in CT group (P < 0.01). Among the patients in the collapse stage, 23 had hip subluxation. The proportion of patients with hip subluxation in NVBG group before treatment was significantly higher than that in CT group (P < 0.01). During follow-up, 14 of those treated surgically had a progression of femoral head collapse, and 37 of 38 cases were in the collapse stage. Among the patients in the collapse stage, seven had hip subluxation (Fig. 2 and Table 1). There was no significant difference in hip subluxation, severe hip deformity, and severe hip arthritis after treatment between CT group and NVBG group (P > 0.05). No intraoperative complications were observed. After treatment, one patient had a superficial incision infection, but it did not appear to affect the clinical or radiographic evaluations.
A boy with left avascular necrosis after femoral neck fracture in the non-vascularized bone grafting (NVBG) group. A Pre-operative anteroposterior radiograph showing a femoral neck fracture in April 2012. B Avascular necrosis (collapse accompanied by hip subluxation) was diagnosed in January 2013. C–D Anteroposterior radiograph at 6 months of follow-up after NVBG showing the development of a collapse. The hip subluxation was not rectified. E–F Anteroposterior radiograph at 3 years of follow-up after NVBG showing a flattened femoral head, severe collapse (> 4 mm), and severe hip arthritis (Tönnis grade 3)
Risk factors for poor prognosis in children and adolescents with AVN after FNF
Non-vascularized bone grafting (NVBG) procedure has not decreased the risk of severe hip deformity at skeletal maturity. At skeletal maturity, four patients were Stulberg type I/II, 19 type III, and 15 type IV/V. After controlling for potentially confounding variables such as sex, age, side, symptom, JIC classification, pre- and post-treatment hip subluxation, and pre- and post-treatment degree of femoral head collapse, the multivariable analysis indicated that NVBG (irrespective of additional containment surgery) did not affect the occurrence of severe hip deformity (type IV/V) and arthritis (grade II/III) (Tables 2 and 3).
The independent risk factors of poor prognosis (severe hip deformity and hip arthritis) were identified through multivariable analysis. Specifically, the occurrence of a severe hip deformity was independently associated with a higher degree of post-treatment femoral head collapse (P < 0.01, OR = 7.64, 95% CI = 3.23–18.04) and pre-treatment hip subluxation (P = 0.02, OR = 7.33, 95% CI = 1.44–37.41). The risk of severe hip arthritis was independently associated with a higher degree of post-treatment femoral head collapse (P = 0.05, OR = 3.80, 95% CI = 1.01–14.29) and post-treatment hip subluxation (P = 0.01, OR = 2.85, 95% CI = 2.31–129.56). Age, sex, side, symptom, treatments, and JIC classification were not associated with poor prognosis (P > 0.05).
Discussion
As the most important finding, the present study accessed a high risk of rapid progression of hip arthritis and hip deformity during follow-up in children and adolescents with AVN after FNF. The results are still insufficient to confirm the superiority of one therapeutic strategy over the other (between CT and NVBG), since the surgical or conservative methods have not significantly affected the prognostic indexes in this study. Multivariable analysis showed that the degree of femoral head collapse after treatment was a risk factor for severe hip arthritis and hip deformity, and the technique of bone grafting was not a significant factor for better outcomes, despite the reports that trapdoor technique has more benefits in the reconstruction of a collapsed head compared to the Phemister and lightbulb techniques [25, 26]. Additionally, these surgical strategies such as extensive pelvic osteotomy or Chiari pelvic osteotomy, aimed at rectifying hip subluxation, did not result in a better prognosis compared with CT. Delayed intervention and insufficient rectification of hip subluxation might contribute to the failure of hip preservation.
Nevertheless, the results suggested potential strategies for hip preservation in children and adolescents with AVN after FNF. Based on the multivariable analysis, the femoral head’s post-treatment degree was the independent risk factor of both hip deformity and arthritis. In addition, pre- and post-treatment hip subluxation was independently associated with the incidence of hip deformity and arthritis. Once the femoral head collapse progressed to hip subluxation, hip deformity was inevitable, regardless of whether it was operated on or not. Therefore, reconstructing femoral head collapse and rectifying hip subluxation as much as possible might help improve both short- and long-term prognosis. On the other hand, when the disease progresses to severe collapse with subluxation and severe arthritis, further hip preservation attempts might be futile.
AVN after FNF shows a strong tendency to become a complex pathological condition, including severe deformity and hip subluxation. It can rapidly degenerate the collapsed areas’ cartilage due to the unstable hip joint and poor containment at the advanced stage. Femoral head collapse, hip deformity, and subluxation can also be found in paediatric AVN of other such as Legg-Calve-Perthes disease [30], sickle cell disease [31], slipped capital femoral epiphysis [32], congenital hip dysplasia [32], or aneurysmal bone cyst [33]. However, a collapsed femoral head is usually remodeled, and the degree of hip deformity is relatively mild, with the secondary osteoarthritis occurring later, in the middle to old aged individuals.
The high risk of progressive femoral head collapse is the deciding factor for poor prognosis in children and adolescents with AVN after FNF. With the progressing collapse, the hip congruency and adequate acetabular coverage can be lost. Instead, incongruency or even lateral subluxation of the hip joint appears. Hip subluxation induces abnormally distributed stress on the femoral head and exacerbates the influence of stress on necrotic lesions [34], which rapidly accelerates the collapse of the femoral head and cartilage destruction.
Among other factors, influencing prognosis, poor containment, and acetabular coverage also tend to interfere with femoral head repair and remodeling in paediatric osteonecrosis, as observed in Perthes disease [30], as well as in our study, where hip subluxation was considered to be the key factor for the progression of AVN after FNF. Another aspect that needed to be investigated in the future studies is a doctor-patient relationship, which is essential for this group of patients. Recent reports indicate that using most novel methods, such as customized 3D printed models, helps towards a more efficient communication and a better understanding of the treatment’s outcomes [35].
This study has several limitations. Firstly, due to the retrospective nature, various biases were introduced, including selection bias, loss to follow-up, and missing data. Among the patients who underwent NVBG, different surgical techniques were used, and the indication for additional containment surgery was unclear in many patients. Secondly, clinical and functional outcomes could not be fully compared due to the late diagnosis leading to inhomogeneity between groups in ARCO staging. However, treatment choice was based on the extent and location of necrosis, which helped to correct selection bias to some degree. Finally, based on our previous clinical experience, hip preservation therapy was our first choice, because arthroplasty is generally not recommended for children [36, 37] and could be used only for patients with hip preservation therapy failure, severe arthritis, and severely limited function due to severe subluxation. It also carries a high likelihood for revision surgery during the lifespan, and whether or not children and adolescents with AVN after FNF benefit from arthroplasty should be further investigated.
In conclusion, children and adolescents with AVN after FNF have a poor prognosis, manifesting as a high risk of hip arthritis and deformity. The optimal method of hip preservation remains unclear for such a population. The degree of femoral head collapse after treatment is a risk factor for deformity and arthritis. When the disease progresses to severe collapse with subluxation and severe arthritis, further hip preservation attempts could be futile.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Palocaren T (2018) Femoral neck fractures in children: a review. Indian J Orthop 52(5):501–506. https://doi.org/10.4103/ortho.IJOrtho_404_17
Akkari M, Santili C, Akel E, Angelim R (2015) Femoral neck fracture in children: treatment and complications. Rev Assoc Med Bras 61(1):5–7. https://doi.org/10.1590/1806-9282.61.01.005
Ratliff AH (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44 B:528–542
Stone JD, Hill MK, Pan Z, Novais EN (2015) Open reduction of pediatric femoral neck fractures reduces osteonecrosis risk. Orthopedics 38(11):e983-990. https://doi.org/10.3928/01477447-20151020-06
Inan U, Kose N, Omeroglu H (2009) Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop 3(4):259–264. https://doi.org/10.1007/s11832-009-0180-y
Barney J, Piuzzi NS, Akhondi H (2020) Femoral head avascular necrosis. StatPearls Publishin, Treasure Island (FL)
Classen T, Becker A, Landgraeber S et al (2016) Long-term clinical results after iloprost treatment for bone marrow edema and avascular necrosis. Orthop Rev (Pavia) 8(1):6150. https://doi.org/10.4081/or.2016.6150
Pritchett JW (2001) Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop Relat Res 386:173–178. https://doi.org/10.1097/00003086-200105000-00022
Glueck CJ, Freiberg RA, Sieve L, Wang P (2005) Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res 435:164–170. https://doi.org/10.1097/01.blo.0000157539.67567.03
Lai KA, Shen WJ, Yang CY, Shao CJ, Hsu JT, Lin RM (2005) The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg Am 87(10):2155–2159. https://doi.org/10.2106/JBJS.D.02959
Agarwala S, Shah S, Joshi VR (2009) The use of alendronate in the treatment of avascular necrosis of the femoral head: follow-up to eight years. J Bone Joint Surg Br 91(8):1013–1018. https://doi.org/10.1302/0301-620X.91B8.21518
Immonen I, Friberg K, Gronhagen-Riska C, von Willebrand E, Fyhrquist F (1986) Angiotensin-converting enzyme in sarcoid and chalazion granulomas of the conjunctiva. Acta Ophthalmol (Copenh) 64(5):519–521. https://doi.org/10.1111/j.1755-3768.1986.tb06965.x
Piuzzi NS, Chahla J, Schrock JB et al (2017) Evidence for the use of cell-based therapy for the treatment of osteonecrosis of the femoral head: a systematic review of the literature. J Arthroplasty 32(5):1698–1708. https://doi.org/10.1016/j.arth.2016.12.049
Lespasio MJ, Sodhi N, Mont MA (2019) Osteonecrosis of the hip: a primer. Perm J 23:18–100. https://doi.org/10.7812/TPP/18-100
Kim YH, Kim JS, Park JW, Joo JH (2011) Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head: a concise follow-up, at an average of seventeen years, of a previous report. J Bone Joint Surg Am 93(19):1806–1810. https://doi.org/10.2106/JBJS.J.01312
Gao F, Sun W, Guo W, Wang B, Cheng L, Li Z (2016) Combined with bone marrow-derived cells and rhBMP-2 for osteonecrosis after femoral neck fractures in children and adolescents: a case series. Sci Rep 6:30730. https://doi.org/10.1038/srep30730
Pisuitthanakan S, Premprabha T (2012) Intravenous bisphosphonate therapy for children who have a traumatic fracture neck of femur and osteonecrosis: a case report. J Med Assoc Thai 95(2):275–278
Bartonicek J, Vavra J, Bartoska R, Havranek P (2012) Operative treatment of avascular necrosis of the femoral head after proximal femur fractures in adolescents. Int Orthop 36(1):149–157. https://doi.org/10.1007/s00264-011-1272-0
Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K (2002) The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci 7(5):601–605. https://doi.org/10.1007/s007760200108
Sultan AA, Mohamed N, Samuel LT et al (2019) Classification systems of hip osteonecrosis: an updated review. Int Orthop 43(5):1089–1095. https://doi.org/10.1007/s00264-018-4018-4
Kubo Y, Motomura G, Ikemura S et al (2018) The effect of the anterior boundary of necrotic lesion on the occurrence of collapse in osteonecrosis of the femoral head. Int Orthop 42(7):1449–1455. https://doi.org/10.1007/s00264-018-3836-8
Rhee PC, Woodcock JA, Clohisy JC et al (2011) The Shenton line in the diagnosis of acetabular dysplasia in the skeletally mature patient. J Bone Joint Surg Am 93(Suppl 2):35–39. https://doi.org/10.2106/jbjs.J.01717
Wei BF, Ge XH (2011) Treatment of osteonecrosis of the femoral head with core decompression and bone grafting. Hip Int 21(2):206–210. https://doi.org/10.5301/HIP.2011.6525
Yildiz C, Erdem Y, Koca K (2018) Lightbulb technique for the treatment of osteonecrosis of the femoral head. Hip Int 28(3):272–277. https://doi.org/10.5301/hipint.5000576
Mont MA, Einhorn TA, Sponseller PD, Hungerford DS (1998) The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br 80(1):56–62. https://doi.org/10.1302/0301-620x.80b1.7989
Ko JY, Meyers MH, Wenger DR (1995) “Trapdoor” procedure for osteonecrosis with segmental collapse of the femoral head in teenagers. J Pediatr Orthop 15(1):7–15. https://doi.org/10.1097/01241398-199501000-00003
Millis MB, Ahearn MC, Hall JE (1990) Transiliac leg lengthening: experiences with a modified Salter osteotomy. Orthopade 19(5):283–291
Gangloff S, Onimus M (1994) Chiari pelvic osteotomy: technique and indications. J Pediatr Orthop B 3(1):68–75
Kovalenko B, Bremjit P, Fernando N (2018) Classifications in brief: Tonnis classification of hip osteoarthritis. Clin Orthop Relat Res 476(8):1680–1684. https://doi.org/10.1097/01.blo.0000534679.75870.5f
Stulberg SD, Cooperman DR, Wallensten R (1981) The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am 63(7):1095–1108
Mallet C, Abitan A, Vidal C et al (2018) Management of osteonecrosis of the femoral head in children with sickle cell disease: results of conservative and operative treatments at skeletal maturity. J Child Orthop 12(1):47–54. https://doi.org/10.1302/1863-2548.12.170141
Castañeda P, Ponce C, Villareal G, Vidal C (2013) The natural history of osteoarthritis after a slipped capital femoral epiphysis/the pistol grip deformity. J Pediatr Orthop 33(Suppl 1):S76-82. https://doi.org/10.1097/BPO.0b013e318277174c
Ulici A, Florea DC, Carp M, Ladaru A, Tevanov I (2018) Treatment of the aneurysmal bone cyst by percutaneous intracystic sclerotherapy using ethanol ninety five percent in children. Int Orthop 42(6):1413–1419. https://doi.org/10.1007/s00264-018-3841-y
Rab GT (2005) Theoretical study of subluxation in early Legg-Calve-Perthes disease. J Pediatr Orthop 25(6):728–733. https://doi.org/10.1097/01.bpo.0000184649.88733.fc
Tevanov I, Liciu E, Chirila MO, Dusca A, Ulici A (2017) The use of 3D printing in improving patient-doctor relationship and malpractice prevention. Rom J Leg Med 25(3):279–282. https://doi.org/10.4323/rjlm.2017.279NOTINPUBMED
Patel NK, Luff T, Whittingham-Jones P, Gooding CR, Hashemi-Nejad A (2012) Total hip arthroplasty in teenagers: an alternative to hip arthrodesis. Hip Int 22(6):621–627. https://doi.org/10.5301/HIP.2012.10352
Wilson AE, O’Malley MJ (2020) Total hip arthroplasty in adolescents and young adults. Oper Tech Orthop 30(1):100785. https://doi.org/10.1016/j.oto.2020.100785
Acknowledgements
The authors would like to thank all study participants who were enrolled in this study.
Funding
This study was supported by Youth Program of National Natural Science Foundation of China (81904226).
Author information
Authors and Affiliations
Contributions
Ziqi Li and Zhikun Zhuang carried out the studies, participated in collecting data, and drafted the manuscript. Zhinan Hong and Leilei Chen performed the statistical analysis and participated in its design. Wei He and Qiushi Wei participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The study was approved by the ethics committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine. The requirement for individual consent was waived by the committee.
Consent to participate
All participants provided written informed consent.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Z., Zhuang, Z., Hong, Z. et al. Avascular necrosis after femoral neck fracture in children and adolescents: poor prognosis and risk factors. International Orthopaedics (SICOT) 45, 2899–2907 (2021). https://doi.org/10.1007/s00264-021-05210-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05210-2