Abstract
Purpose
To verify if indirect radiographic signs of first metatarsal pronation, determined by the head round sign, correspond to weight-bearing computed tomography (WBCT) measurements.
Methods
In this case–control retrospective study, we analyzed 26 hallux valgus (HV) feet and 20 controls through conventional radiograph (CR) and WBCT images. Two blinded orthopaedic foot and ankle surgeons performed the measurements. Pronation classification (head roundness), head diameter (HD), traditional HV angles, arthritis, sesamoid positioning, and first metatarsal rotation angle (MRA) (alpha angle) were evaluated. Comparisons were performed by Student’s T-test and a multivariate regression was executed. P-values less than 0.05 were considered significant.
Results
Mean values were higher in HV patients than controls when evaluating MRA (11.51 [9.42–13.60] to 4.23 [1.84–6.62], 95%CI), HD (22.35 [21.52–23.18] to 21.01 [20.07–21.96]), and sesamoid rotation angle (SRA) (26.72 [24.09–29.34] to 4.56 [1.63–7.50]). The MRA had a low influence in head roundness classification (R2: 0.15). Changes in the pronation classification were explained chiefly by the sesamoid station (SS) (R2: 0.37), where stations 4 to 7 were found to be strong predictors of roundness classifications 2 and 3.
Conclusion
Indirect signs of metatarsal pronation, determined by the head round sign, correlate weakly with the alpha angle measured in WBCT. The presence of arthritis and sesamoids displacement might modify the perception of first head roundness. The influence of MRA in the classification was low, where SS from 4 to 7 was strong predictors of a higher pronation classification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Indirect radiographic findings in plain weight-bearing conventional radiographs (CR) are commonly used for the assessment and treatment of many foot and ankle disorders, especially hallux valgus (HV) [1,2,3]. The shape of the first metatarsal head in the anteroposterior CR was proposed as a parameter for ray rotation in the coronal plane [4,5,6]. Pronation degree is estimated from the indirect evaluation of the lateral head round sign, which gives an estimated range of probable rotation in the first metatarsal [4, 7]. An irregular lateral head shape would indicate 10 to 19° of pronation, a rounded 20 to 29°, and a circular head of 30 to 39° of first metatarsal pronation [4]. The projected rotation could be applied to surgical techniques in hallux valgus, from osteotomies to modified fusions, in an attempt to maximize corrections and functional results [8, 9].
On the other hand, the amount of first metatarsal rotation, its physiologic, and pathologic values are still a matter of debate [6, 10, 11]. Since many of these findings were performed utilizing non-weight-bearing devices or CR, the results may not reflect the accurate representation of the normal and abnormal ray [3, 12]. Weight-bearing computed tomography (WBCT) may better estimate the natural rotation of the structures due to its intrinsic three-dimensional interpretation capability [13]. A recent investigation in a population with no deformity, showed mean pronation values of 2.1 and 6.1° [14]. Many methods to assess metatarsal rotation were described, but the alpha angle remained the most utilized measurement technique [15].
Distal metatarsal articular angle (DMAA), a traditional HV measure, quantifies head articulation valgus deviation in relation to the first ray axis [16]. Also used as an argument for different procedures through the last few decades, this angle was very debated due to CR measurement errors and positioning [17]. Because of the current discussion surrounding rotation, it regained attention as a potential indirect sign of ray pronation [18]. Sesamoid positioning in conventional CR has also been portrayed as a suitable parameter for deformity severity and soft tissue imbalance [12, 19]. Different authors include sesamoid location and arthritic changes to the HV treatment algorithm, using indirect findings [19, 20].
Most of these parameters were subjectively described and based on a single radiographic visualization. The absence of validation is also a limitation to these criteria. Several authors showed how foot positioning, metatarsal inclination, and arthritis could jeopardize readings [7, 21]. The primary objective of this study was to demonstrate if first metatarsal rotation measured by the alpha angle in WBCT images correlates with it the pronation classification, determined by the roundness of the head in CR. Secondarily, other direct and indirect HV parameters will be tested as confounding factors. We hypothesized that alpha angle values would not reliably reflect an indirect classification for rotation, and other variables would contribute to miscalculation.
Methods
Design
This retrospective case–control study was approved by the institution’s IRB, observing the Health Insurance Portability and Accountability Act (HIPAA) and the Declaration of Helsinki requirements.
Hallux valgus patients treated at a single institution between January 2017 and November 2020 were studied. Subjects included were 18 years of age or older with a clinical and radiological diagnosis hallux valgus. The presence of pain at the medial aspect of the metatarsophalangeal joint, lateral hallux deviation, intermetatarsal angle above 9°, and hallux valgus angle over 15° was considered for inclusion. For a baseline assessment of their foot, each patient underwent a WBCT and a full CR assessment as the standard of care. Recurrent cases were not excluded. Individuals sustaining progressive collapsing foot deformity (PCFD), cavovarus, and congenital diseases were not included in this series.
Control patients were selected from the institution database in the same period mentioned above. Adults (> 18 years old) that underwent CR and WBCT as the standard of care for different diseases (Table 1) were considered. Hallux valgus angle under 15° was required for this group. Individuals were also excluded if they had any forefoot complaint (current and prior), signs of any deformity, or arthritis (hindfoot, midfoot, and forefoot) noticeable during imaging assessment.
Subjects
A total of 26 hallux valgus feet (50% left, 50% right) from 19 patients (89% female; 11% male) were included, with a median age of 53.79 years (range 18–92; SD 8.09) and a median BMI of 29.60 (SD 5.50). A total of 20 control feet (35% left, 65% right) from 16 patients (50% male, 50% female) were incorporated, with a median age of 38.18 years (range 17–71; SD 16.37) and a median BMI of 30.98 (SD 8.29).
Imaging acquisitions
WBCT scans were performed with a cone-beam CT extremity scanner (PedCAT; CurveBeam, LLC, Warrington, PA, USA). Patients were instructed to stand upright with their feet pointing forward approximately shoulder-width apart and instructed to distribute weight evenly on both lower extremities.
A complete set of conventional bilateral weight-bearing foot radiographs was performed, including anteroposterior, lateral, and oblique views.
Radiographic measurements
Two fellowship-trained orthopedic foot and ankle surgeons with more than 10 years of experience executed all the evaluations and angle measurements. Anteroposterior weight-bearing radiographs (Vue PACS™, Carestream, USA) were used to classify the metatarsal pronation according to Wagner et al., grade metatarsophalangeal (MTP) arthritis, calculate the hallux valgus angle (HVA), the intermetatarsal angle (IMA), the distal metatarsal articular angle (DMAA), the interphalangeal angle (IPA), and the sesamoid station (SS) [22].
Metatarsal pronation was classified according to the metatarsal head roundness on a scale from zero to three, zero being a sharp head, one an irregular head, two a rounded head, and three a circular head [4]. Metatarsal arthritis was rated according to the radiographical domain of the Coughlin-Shurnas classification [23]. The sesamoid station was defined according to Hardy-Clapham [19].
WBCT measurements
Raw multiplanar nonidentified data was converted into sagittal, coronal, and axial plane images and evaluated using dedicated software (CubeVue™, CurveBeam, LLC, Warrington, PA, USA). The same fellowship-trained orthopaedic foot and ankle surgeons performed all the WBCT measurements.
In the axial plane, HVA, IMA, DMAA, IPA, and SS were recorded [4, 13, 19, 22,23,24]. Sesamoid coronal position (SP), sesamoid rotation angle (SRA), head diameter (HD), glenosesamoid arthritis (GSA), and first metatarsal alpha rotation angle (MRA) were measured in the coronal plane [12, 20, 22]. In the sagittal plane, the first metatarsal declination angle (MDA) was performed [25].
The metatarsal and phalanx axis was established in the axial plane, and angular measurements were performed using the Cobb method [13, 26]. The most medial and the most lateral articular voxel of the metatarsal head were used to establish the DDMA.
SP was ascertained by using the Smith method and GSA according to the Stanmore classification [20]. SRA and MRA were also assessed in the coronal plane using its published methods [12, 13]. The diameter of the first metatarsal head was calculated using the coronal image of the head that contained its largest segment, considering local anatomy and possible plantar osteophytes.
Statistical analysis
Inter-rater reliabilities for continuous data were performed using interclass correlations coefficients (ICC) and categorical data using Cohen’s Kappa. For each measurement, data were evaluated for normality using the Shapiro–Wilk test, and descriptive statistics were obtained (mean, median, interquartile range (IQR), 95% confidence interval values). For each angle, we used the one-way ANOVA for analysis and the paired Student’s T-test for comparisons of each pair. A multivariate regression analysis was executed to evaluate which of the measurements influenced the rotation classification, and a partition prediction model was constructed to find how the variables contributed to the grading system. P-values of ≤ 0.05 were considered significant.
Results
Reliabilities utilizing ICC were over 0.70 and Kappa over 0.50 for WBCT and CR readings (Tables 2 and 3). HV patients were older than controls (p = 0.01) but similar regarding BMI (p = 0.85).
When comparing WBCT and CR measurements, considering HV, similarity was found between for HVA (p = 0.79), IMA (p = 0.39), SS (p = 0.40), and IPA (p = 0.09). A significant difference was found for DMAA (p < 0.01), where CR evaluation had higher mean values (diff 13.43, SE 1.99, 9.43–17.43, 95%CI). The full comparison among methods can be found in the Supplementary Material.
Comparison between groups showed mean higher values for MRA (p < 0.01) in HV patients (11.51; 9.42–13.60, 95%CI) than controls (4.23; 1.84–6.62, 95%CI) (Fig. 1). Mean HD was higher (p = 0.01) in HV (22.35; 21.52–23.18, 95% CI) than controls (21.01; 20.07–21.96, 95%CI) and mean SRA was also higher (p < 0.01) in HV (26.72; 24.09–29.34, 95%CI) than controls (4.56; 1.63–7.50, 95%CI). Pronation classification using head roundness was also different among controls and HV patients (Fig. 1). MTP arthritis and SA were also graded higher in the HV group (p < 0.01). Differences among groups for other traditional hallux valgus angles are depicted in the Supplementary Material.
MRA was poorly correlated to HVA, IMA, and DMAA (values below 0.39) but moderately with SRA (0.61). DMAA in CR was correlated strongly with HVA (0.88) and moderately with SRA (0.57). SRA was moderately correlated with HVA (0.70) and IMA (0.60) (Supplementary Material).
Changes in the pronation classification, determined by head roundness, were explained only by SS, MRA, and MTP arthritis (p < 0.02; R2: 0.42) (Table 4). The influence was mainly due to the SS (R2: 0.37), where stations 4 to 7 were strong predictors of roundness classification 2 and 3 (85% probability). The MRA had a low influence on the pronation classification (R2: 0.16).
Discussion
The present study tested the correlation between a subjective parameter of metatarsal rotation, established by the roundness of the head in CR, and a direct metatarsal rotation measure, the alpha angle, using WBCT. We demonstrated a low influence of the MRA on the proposed pronation classification (R2: 0.16), which was chiefly justified by the sesamoid position on the axial plane (sesamoid station). We also showed significant differences between controls and patients with HV when considering variables that could confound indirect rotational evaluation through CR, such as MTP arthritis and SA. The findings confirm our main hypotheses.
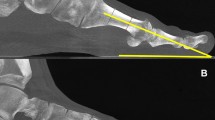
The rotation of the first metatarsal has been long described as a component in the three-dimensional HV deformity [5, 10]. Although known to be present, rotation was never given such importance until the work by Okuda et al., which showed that the roundness of the head in the post-operative radiographs was a predictor of recurrence [1]. The authors divided the shape of the lateral head into angular, intermediate, and round, finding that the latter format, an indirect sign of a metatarsal rotated, was more associated with HV reappearance [8]. The concept of head lateral roundness was later tested by Yamaguchi et al. using digitally reconstructed radiographs from conventional computed tomography subjects [7]. The authors showed a positive “round” lateral head as pronation and plantarflexion occurred at the first ray [7]. Wagner et al. used the rotational characteristic of this indirect sign to propose a proximal metatarsal osteotomy to correct HV in axial and coronal planes [4, 27]. The correction is based on a range of expected pronation based in a sharp (0°), irregular (10–19°), rounded (20–29°), or circular (30–39°) head. Although intuitive, the actual amount of rotation seen with each head roundness was never confirmed. Our study has shown that most of the indirect determination of the metatarsal shape is based on the position of the sesamoid in the axial plane, what could be explained by the two-dimensional feature of the CR and the superposition of images, allowing the sesamoids to be confused with the lateral head condyle (Fig. 2). MDA, demonstrated by Yamaguchi et al. as an important factor that would change the perception of the head shape, was not found by our study to interfere in the pronation classification [7].
Grade 2 (rounded) head roundness on conventional radiographs (A) not justified by rotation of the metatarsal on coronal weight-bearing CT (B). Three-dimension reconstruction on weight-bearing CT (C) allows a better visualization of the lateral sesamoid invading the webspace, causing confusion on the evaluation of the head shape
The modest effect of the MRA on the pronation classification also supports the concept that much of this indirect parameter can be blurred by other structures, head osteophytes, glenosesamoid arthritis, or MTP arthritis. Ono et al. showed a high occurrence of sesamoid-metatarsal arthritis in patients with HV, with a higher incidence (77%) in patients with a rounded metatarsal head, advising caution when predicting pronation in patients with degenerative findings [21]. We also found a significant difference between HV patients and controls in WBCT assessment of HD when considering osteophytes in the measurement. This lateral bone formation, sometimes very subtle and difficult to be identified in CR, can easily modify the lateral head shape (Fig. 3). Such minimal and inconspicuous arthritic findings in this joint are usually not covered by the current classifications systems [20, 28].
Many attempts in determining the actual first metatarsal rotation have been described both in an HV and a healthy population. Radiographic assessment of this component was unreliable due to the difficulty in measuring bone references and the bias caused by MTP dorsiflexion, necessary to the CR be performed [29, 30]. Kim et al., using simulated WBCT, were able to describe the alpha angle and place deformities in four different patterns [12]. Using the difference (and the 95% confidence interval) between controls and HV patients, the authors established a 15.8° threshold for normal pronation, with values above that being considered pathologic [12]. Campbell et al., using three-dimensional models, found mean pronation of 19.1° in controls and 27.3° in HV patients [31]. Applying WBCT in a population with no deformities, Steadman et al. used two different methods for measuring the first metatarsal rotation, the alpha angle (described by Kim et al.), and the metatarsal rotational angle (described by Saltzman et al.) [5, 12, 14]. The authors described a mean of 6.1° and 2.1° in pronation, respectively. These findings might support the use of Saltzman’s method since it does not rely on the visualization of the dorsal aspect of the metatarsal to be obtained [14, 32]. Our results, using the alpha angle, approached the values observed by Steadman et al. for controls (mean MRA: 4.23°) and did not reach the values obtained by Campbell et al. and Kim et al. for HV patients (mean MRA: 11.51°) [12, 14, 31]. Our smaller sample might be the reason for a lower MRA in the HV population, but still, the values are far from what was proposed by Wagner et al. and when considering staging of the pronation degree of the deformity [4].
Additional interesting secondary findings were observed in our study. Axial aspects of the deformity (HVA, IMA, IPA) were similarly measured by WBCT and CR, which corroborates Mahmoud et al. [13]. When considering three-dimensional aspects of the HV, such as DMAA and SS, the imaging methods showed disparity, demonstrating the difficulties in using these indirect parameters of the CR with consistency. DMAA, stated by some authors as another indirect sign of metatarsal rotation, had statistically lower values in WBCT and did not show influence in the pronation classification nor correlation with the MRA [18, 33].
The clinical importance of our findings resides mainly on the caution of using conventional radiographs to determine first metatarsal rotation. Based on what was found, we recommend using WBCT measurements to determine preoperative and postoperative pronation or supination. Adoption of a de-rotational osteotomy to correct this component is still a matter of debate and investigation. It is not known if specific procedures can impact rotation and the power of each technique on that. No prospective studies were yet performed testing these hypotheses using a well-established measuring method.
The present study has several limitations that must be considered. An accurate linear evolution of HV could not be evaluated due to the retrospective nature of this study. Although we had statistically significant differences and correlations, no previous sample calculation or power analysis was performed. This deficiency undermines the study’s capability to place a substantial number of subjects in each of the classification grades. No functional assessment was performed, making it unfeasible to relate symptoms to imaging findings. We also used a parameter to assess rotation that might be outdated in future years with the advent of bone segmentation [15, 34]. Finally, the use of the WBCT is still not widely accessible, which decreases the study’s reproducibility.
Conclusion
Overall, we found that metatarsal rotation cannot be reliably predicted through head roundness. Sesamoid subluxation and arthritis alter the first metatarsal head shape and diameter, blurring the evaluation. Sesamoid stations from 4 to 7 were strong predictors of higher pronation classifications. First metatarsal rotation (alpha angle) values in WBCT did not influence the classification strongly nor were correlated to HV measurements.
References
Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H (2007) The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am 89:2163–2172. https://doi.org/10.2106/JBJS.F.01455
Wagner E, Wagner P (2020) Metatarsal pronation in hallux valgus deformity: a review. J Am Acad Orthop Surg Glob Res Rev 4(6):e20.00091. https://doi.org/10.5435/JAAOSGlobal-D-20-00091
Cruz EP, Wagner FV, Henning C, Sanhudo JAV, Pagnussato F, Galia CR (2019) Does hallux valgus exhibit a deformity inherent to the first metatarsal bone? J Foot Ankle Surg 58:1210–1214. https://doi.org/10.1053/j.jfas.2018.09.031
Wagner P, Wagner E (2018) Is the rotational deformity important in our decision-making process for correction of hallux valgus deformity? Foot Ankle Clin 23:205–217. https://doi.org/10.1016/j.fcl.2018.01.009
Saltzman CL, Brandser EA, Anderson CM, Berbaum KS, Brown TD (1996) Coronal plane rotation of the first metatarsal. Foot Ankle Int 17:157–161. https://doi.org/10.1177/107110079601700307
Mortier JP, Bernard JL, Maestro M (2012) Axial rotation of the first metatarsal head in a normal population and hallux valgus patients. Orthop Traumatol Surg Res 98:677–683. https://doi.org/10.1016/j.otsr.2012.05.005
Yamaguchi S, Sasho T, Endo J, Yamamoto Y, Akagi R, Sato Y, Takahashi K (2015) Shape of the lateral edge of the first metatarsal head changes depending on the rotation and inclination of the first metatarsal: a study using digitally reconstructed radiographs. J Orthop Sci 20:868–874. https://doi.org/10.1007/s00776-015-0749-x
Prado M, Baumfeld T, Nery C, Mendes A, Baumfeld D (2020) Rotational biplanar Chevron osteotomy. Foot Ankle Surg 26:473–476. https://doi.org/10.1016/j.fas.2019.05.011
Dayton P, Feilmeier M (2017) Comparison of tibial sesamoid position on anteroposterior and axial radiographs before and after triplane tarsal metatarsal joint arthrodesis. J Foot Ankle Surg 56:1041–1046. https://doi.org/10.1053/j.jfas.2017.05.006
Talbot KD, Saltzman CL (1997) Hallucal rotation: a method of measurement and relationship to bunion deformity. Foot Ankle Int 18:550–556. https://doi.org/10.1177/107110079701800904
Steadman J, Barg A, Saltzman CL (2021) First metatarsal rotation in hallux valgus deformity. Foot Ankle Int 42:510–522. https://doi.org/10.1177/1071100721997149
Kim Y, Kim JS, Young KW, Naraghi R, Cho HK, Lee SY (2015) A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int 36:944–952. https://doi.org/10.1177/1071100715576994
Mahmoud K, Metikala S, Mehta SD, Fryhofer GW, Farber DC, Prat D (2021) The role of weightbearing computed tomography scan in hallux valgus. Foot Ankle Int 42:287–293. https://doi.org/10.1177/1071100720962398
Steadman J, Bakshi N, Arena C, Leake R, Barg A, Saltzman CL (2021) Normative distribution of first metatarsal axial rotation. Foot Ankle Int. https://doi.org/10.1177/10711007211001015
Conti MS, Patel TJ, Caolo KC, Amadio JM, Miller MC, Costigliola SV, Ellis SJ, Conti SF (2021) Correlation of different methods of measuring pronation of the first metatarsal on weightbearing CT scans. Foot Ankle Int. https://doi.org/10.1177/10711007211003090
Bolzinger M, Thevenin-Lemoine C, Gallini A, Gauzy JS (2021) Abnormalities in distal first metatarsal joint surface orientation: Distal Metatarsal Articular Angle and Distal Metatarsal-2 Articular Angle. Orthop Traumatol Surg Res 22:102938. https://doi.org/10.1016/j.otsr.2021.102938
Lee KM, Ahn S, Chung CY, Sung KH, Park MS (2012) Reliability and relationship of radiographic measurements in hallux valgus. Clin Orthop Relat Res 470:2613–2621. https://doi.org/10.1007/s11999-012-2368-6
Cakmak G, Kanatlı U, Kılınç B, Yetkin H (2013) The effect of pronation and inclination on the measurement of the hallucal distal metatarsal articular set angle. Acta Orthop Traumatol Turc 47:354–358. https://doi.org/10.3944/aott.2013.2669
Hardy RH, Clapham JC (1951) Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br 33-b:376–391. https://doi.org/10.1302/0301-620x.33b3.376
Welck MJ, Singh D, Cullen N, Goldberg A (2018) Evaluation of the 1st metatarso-sesamoid joint using standing CT - the Stanmore classification. Foot Ankle Surg 24:314–319. https://doi.org/10.1016/j.fas.2017.03.005
Ono Y, Yamaguchi S, Sadamasu A, Kimura S, Watanabe S, Akagi R, Sasho T, Ohtori S (2020) The shape of the first metatarsal head and its association with the presence of sesamoid-metatarsal joint osteoarthritis and the pronation angle. J Orthop Sci 25:658–663. https://doi.org/10.1016/j.jos.2019.06.013
Coughlin MJ, Saltzman CL, Nunley JA 2nd (2002) Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int 23:68–74. https://doi.org/10.1177/107110070202300114
Coughlin MJ, Shurnas PS (2003) Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int 24:731–743. https://doi.org/10.1177/107110070302401002
Van Deventer SJ, Strydom A, Saragas NP, Ferrao PNF (2020) Morphology of the first metatarsal head as a risk factor for hallux valgus interphalangeus. Foot Ankle Surg 26:105–109. https://doi.org/10.1016/j.fas.2018.12.004
Cheung ZB, Myerson MS, Tracey J, Vulcano E (2018) Weightbearing CT scan assessment of foot alignment in patients with hallux rigidus. Foot Ankle Int 39:67–74. https://doi.org/10.1177/1071100717732549
Apostle KL, Coleman NW, Sangeorzan BJ (2014) Subtalar joint axis in patients with symptomatic peritalar subluxation compared to normal controls. Foot Ankle Int 35:1153–1158. https://doi.org/10.1177/1071100714546549
Wagner P, Wagner E (2019) The use of a triplanar metatarsal rotational osteotomy to correct hallux valgus deformities. JBJS Essent Surg Tech 9(4):e43 1-2. https://doi.org/10.2106/JBJS.ST.19.00010
Choi JY, Ahn HC, Baek HS, Park JH, Suh JS (2019) Factors influencing medial sesamoid arthritis in patients with hallux valgus deformity: magnetic resonance imaging evaluation. Foot Ankle Surg 25:612–617. https://doi.org/10.1016/j.fas.2018.06.003
Eustace S, O’Byrne J, Stack J, Stephens MM (1993) Radiographic features that enable assessment of first metatarsal rotation: the role of pronation in hallux valgus. Skeletal Radiol 22:153–156. https://doi.org/10.1007/BF00206143
Yildirim Y, C¸Abukoglu C, Erol B, Esemenli T, (2005) Effect of metatarsophalangeal joint position on the reliability of the tangential sesamoid view in determining sesamoid position. Foot Ankle Int 26:247–250. https://doi.org/10.1177/107110070502600311
Campbell B, Miller MC, Williams L, Conti SF (2018) Pilot study of a 3-dimensional method for analysis of pronation of the first metatarsal of hallux valgus patients. Foot Ankle Int 39:1449–1456. https://doi.org/10.1177/1071100718793391
Najefi AA, Zaveri A, Alsafi MK, Malhotra K, Patel S, Cullen N, Welck M (2021) The Assessment of First Metatarsal Rotation in the Normal Adult Population Using Weightbearing Computed Tomography. Foot Ankle Int 13:10711007211015187. https://doi.org/10.1177/10711007211015187
Robinson AH, Cullen NP, Chhaya NC, Sri-Ram K, Lynch A (2006) Variation of the distal metatarsal articular angle with axial rotation and inclination of the first metatarsal. Foot Ankle Int 27:1036–1040. https://doi.org/10.1177/107110070602701207
Dibbern KN, Li S, Vivtcharenko V, Auch E, Lintz F, Ellis SJ, Femino JE, de Cesar Netto C (2021) Three-Dimensional Distance and Coverage Maps in the Assessment of Peritalar Subluxation in Progressive Collapsing Foot Deformity. Foot Ankle Int 42(6):757–767. https://doi.org/10.1177/1071100720983227
Author information
Authors and Affiliations
Contributions
Nacime Salomão Barbachan Mansur: had full access to all the data in the study and takes responsibility for the integrity and accuracy of the data analysis, literature revision, study design, writing, paper submissions, and data collecting.
Matthieu Lalevee: co-supervisor, writing, data collecting, and paper submission.
Eli Schmidt: literature revision, writing.
Kevin Dibbern: literature revision, writing.
Pablo Wagner: literature revision, writing.
Emilio Wagner: literature revision, writing.
Caio Nery: literature revision, writing.
Cesar de Cesar Netto: supervisor, literature revision, writing, study design, and paper submissions.
Each author contributed to the refinement of the study protocol and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics and means of dissemination
University Ethics Committee approved this research under the number 202012422 in accordance with the Declaration of Helsinki.
Competing interests
Nacime Salomao Barbachan Mansur, MD, PhD (Brazil): Brazilian Foot and Ankle Society: Board or committee member. Pablo Wagner, MD (Chile); DePuy, A Johnson & Johnson Company: other financial or material support Elsevier: Editorial or governing board paragon28: IP royalties. Emilio Wagner, MD: Arthrex, Inc: Paid consultant DePuy, A Johnson & Johnson Company: Other financial or material support; Research support Paragon28: IP royalties Promedon Chile: Other financial or material support. Caio Augusto de Souza Nery, MD, PhD (Brazil): Arthrex: Paid presenter or speaker. Cesar De Cesar Netto, MD, PhD (Iowa City, IA): American Orthopaedic Foot and Ankle Society: Board or committee member CurveBeam: Paid consultant; Stock or stock Options Foot and Ankle International: Editorial or governing board Nextremity: Paid consultant Ossio: Paid consultant Paragon 28: IP royalties; Paid consultant Weightbearing CT International Study Group: Board or committee member Zimmer: Paid consultant. The other authors have nothing to disclose.
Disclaimer
The cited companies did not finance the study or participate in any phase of its conduction. The implants used in this study were from several companies as the surgeries were performed at a public hospital.
Data sharing
According to the ICMJE data sharing police, core records will be shared through Mendeley Data and available upon request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III, Retrospective Diagnostic Study
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mansur, N.S.B., Lalevee, M., Schmidt, E. et al. Correlation between indirect radiographic parameters of first metatarsal rotation in hallux valgus and values on weight-bearing computed tomography. International Orthopaedics (SICOT) 45, 3111–3118 (2021). https://doi.org/10.1007/s00264-021-05136-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05136-9