Abstract
Background
Periprosthetic femur fractures (PPFF) distal to a femoral stem are traditionally treated with open reduction and internal fixation (ORIF) with plate and screws. To our knowledge, no studies exist comparing outcomes following ORIF vs retrograde intramedullary nails (RIMN) for this injury.
Methods
This is a retrospective comparison of PPFFs distal to a femoral stem treated by ORIF (n = 17) vs RIMN (n = 13). The primary outcome was unplanned re-operation.
Results
There was no difference in unplanned re-operation (17.6 vs 23.1%, p > 0.99), infection, nonunion, refracture, and alignment between groups. The RIMN group had shorter surgical time (89 vs 157 min, p < 0.01), less blood loss (137 vs 291 ml, p = 0.03), and greater obesity.
Conclusion
RIMN is a potential option for operative fixation of PPFF distal to a femoral stem worthy of additional study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic femur fractures (PPFF) are a growing epidemic worldwide, with some authors estimating that the incidence of such injuries may reach 5% by 20 years after primary total hip arthroplasty (THA) [1,2,3,4]. As a result of increased THA and total knee arthroplasty (TKA) procedures over time and the expanded indications to sicker and older patients, the burden of periprosthetic femur fractures is expected to steadily rise.
Traditionally, fractures distal to a femoral stem have been treated with open reduction and internal fixation with a plate and screw construct overlapping the stem. This has also been the standard fixation method for interprosthetic fractures between THA and TKA prostheses. Previous biomechanical studies have supported this method of fixation citing evidence that a distal locking plate bypassing a prosthetic stem requires a greater fracture force to break the femur below the stem compared with other fixation constructs [5,6,7,8]. To our knowledge, there are no clinical studies comparing outcomes in patients with periprosthetic femur fractures distal to a femoral stem treated with different implants.
At our institution, distal periprosthetic and interprosthetic femur fractures are routinely treated with locked plate constructs and retrograde nails. Consequently, we sought to compare clinical and patient-reported outcomes (PROs) in patients treated with nails versus plates for interprosthetic and periprosthetic femur fractures below a femoral stem. We hypothesized that the retrograde nail group would have a similar rate of early re-operation to the plate group in the treatment of these fractures.
Materials and methods
After obtaining institutional review board approval, a retrospective medical chart and radiograph review was performed on patients treated between January 1, 2013, and June 30, 2018. Query of a billing database and radiograph review identified 246 operatively repaired periprosthetic femur fractures (PPFF) in patients older than 17 years of age. Of these patients, 42 patients had Vancouver type C or interprosthetic fractures. Ten patients with less than 90-day follow-up were excluded from the analysis.
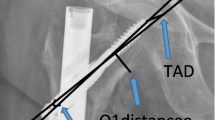
The fracture distance (FD) was measured from the distal tip of the THA stem to the level of the fracture and measured in millimeters. Additionally, the distance between the proximal tip of the retrograde nail and the position of second-most proximal interlock hole in the vast majority of retrograde femoral nail designs was recorded, and this was qualified as the interlock distance (ID) (Fig. 1). The majority of nail designs have an ID of 40 mm or greater, and to ensure a sufficiently comparable cohort amenable to either plating or intramedullary nailing, we studied fractures with a FD of 40 mm or greater. This gave the surgeon the option to place two proximal interlock screws through the nail if the retrograde nailing option was chosen. Two patients with PPFF within 40 mm of the femoral stem were excluded.
a The interlock distance (ID) from the proximal tip of the retrograde nail to the second-most proximal interlock screw for most nail designs is at least 40 mm. b The fracture distance (FD) was determined for each fracture as the distance between the distal tip of the THA stem and the level of the fracture. Fractures with a FD < 40 mm were excluded from the study
Demographics and injury characteristics were collected including age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) score, pre-operative ambulatory status, mechanism of injury, concomitant injuries, Gustilo-Anderson open fracture type, and unified classification type [9]. Resource utilization and surgical details, such as hospital length of stay, time from admission to surgery, length of surgery, disposition after discharge, type of implant used, post-operative weight-bearing status, estimated blood loss (EBL), and change in haemoglobin (Hgb) preoperatively to 24 hours after surgery, were recorded. Underlying medical comorbidities were assessed via the Charlson comorbidity index (CCI). The CCI is a common validated metric for estimating future mortality and is a weighted sum tally of existing patient diseases [10].
The primary outcomes were unplanned re-operation for deep infection (requiring surgical debridement), nonunion, and refracture. PROs were collected for all patients using the visual analog scale (VAS) and Patient-Reported Outcomes Measurement Information System (PROMIS) instrument. Specifically, the short forms physical function (PF) and pain interference (PI) were recorded [11, 12]. Radiographic analysis included initial post-operative coronal and sagittal alignment and final follow-up alignment. Malalignment in the coronal plane was considered to be greater than a 5° deviation from the normal anatomic lateral distal femoral angle (aLDFA) of 81° [13]. Similarly, malalignment in the sagittal plane was considered to be greater than a 5° deviation from the normal anatomic posterior distal femoral angle (PDFA) of 83° [13]. To the authors’ knowledge, there is no commonly accepted method to measure sagittal alignment in the setting of TKA prostheses. “Sagittal deviation” was recorded for patients with a knee prosthesis, defined by the angle formed by the axis of the proximal femoral shaft segment and the anterior flange of the prosthesis. Zero degrees were considered normal and a 5° deviation was deemed “malaligned.”
Continuous variables are reported as mean ± standard deviation and compared using Student’s t test. Fisher’s exact test was used to compare categorical variables. Statistical significance was set as p ≤ 0.05.
Results
There were 30 patients in the study group, 17 patients in the plate group, and 13 in the retrograde intramedullary nail (RIMN) group. Mean clinical follow-up in the plate group was 437 days compared with 367 days (p = 0.59) in the RIMN group. The plate group was ten years older on average than the nail group (77 vs 67 years, p = 0.04). There were more females in the RIMN group, and the average BMI for patients in the RIMN group was higher than the plate group (34 vs. 27, p = 0.05) (Table 1). There was no difference in post-operative weight-bearing between both groups, although there was a trend towards more patients prescribed full weight-bearing in the RIMN group (6 (46%) vs. 3 (18%), p = 0.05). The post-operative change in Hgb was similar for both groups (1.8 vs 1.3 units, p = 0.34); however, the operatively reported EBL was on average higher for the plate group compared with the RIMN group (291 vs 137 ml, p = 0.03). The average time from admission to surgery and the overall length of stay did not differ between the two groups. Surgical duration was 68 minutes shorter in RIMN group compared with the plate group (157 vs 89 minutes, p < 0.01) (Table 1). There were seven interprosthetic fractures in the plate group (41%) and five in the nail group (38%).
There were three re-operations in the plate group and 3 in the RIMN group (Table 2). There was one deep infection requiring debridement in the plate group and none in the RIMN group. The infected fracture communicated with both the THA and TKA prostheses and was ultimately eradicated following debridement and revision arthroplasty. There were two re-operations for nonunion in the plate group and 1 in the RIMN group, all of whom underwent revision fixation with autologous bone graft. Additionally, there was one patient in the plate group who had a CT established nonunion that was treated non-operatively due to advanced age and low functional demand. There was one refracture in the RIMN group and none in the plate group. This refracture occurred 82 days after the original surgery after a ground-level fall and was revised with plate fixation. Additionally, one patient in the RIMN group complained of mid-thigh pain nine months post-operatively and underwent supplemental prophylactic plate fixation despite no radiographic abnormality. This patient was a lung transplant patient on numerous immunosuppressive agents and the treating surgeon proceeded with supplemental plate fixation to help diminish the patient’s thigh pain. There were two deaths in the plate group and five in the RIMN group (p = 0.19) (Table 2).
Initial post-operative coronal and sagittal malalignment did not differ between the plate and RIMN groups, respectively (coronal malalignment 0/17 vs. 0/13, p > 0.99; sagittal malalignment 3/17 vs. 2/13, p > 0.99). At final follow-up, coronal and sagittal malunion was also similar for the plate and RIMN groups, respectively (coronal malunion 2/17 vs. 1/13, p > 0.99; sagittal malunion 3/17 vs. 2/13, p > 0.99) (Table 2).
There was no difference in PROs between the plate and RIMN groups: mean PROMIS PF 32.9 vs. 32.0, p = 0.87; mean PROMIS PI 58.1 vs. 57.1, p = 0.63, respectively. There was also no difference in VAS at final follow-up between groups (Table 2).
Discussion
Periprosthetic and interprosthetic fractures are becoming increasingly problematic due to an aging population and growing incidence of total hip and knee arthroplasty. A clinical dilemma exists in the treatment of fractures distal to a femoral stem. Retrograde femoral nails have shown comparable clinical outcomes to fixed-angle plate devices in the treatment of supracondylar femur fractures [14]. However, in the setting of a THA femoral stem, several authors have suggested that a retrograde femoral nail should be avoided [5, 6, 8]. We have routinely used RIMN to treat periprosthetic femur fractures distal to the tip of the femoral stem, as well as interprosthetic fractures between stemless TKA and THA femoral implants (Figs. 2 and 3). This investigation found similar outcomes and complication profiles following plate or nail fixation for this injury and less surgical time and potentially less blood loss with nailing.
Multiple authors have cautioned against the use of RIMN below a THA stem primarily based on biomechanical analyses [5, 6, 8]. Rupprecht et al. harvested 48 cadaveric femurs, implanted both THA and TKA prostheses, and conducted a four-point bending test until fracture [5]. The authors found that the insertion of a femoral stem decreases femoral stiffness by approximately 33% and that ipsilateral retrograde nailing reduces the force to failure even further [5]. In a similar study, Lehmann et al. showed that a cadaveric femur with a hip prosthesis and a retrograde femoral nail exhibited 20% lower fracture strength in comparison with a femur with THA stem only [8]. In a subsequent study, Lehmann et al. tested 30 cadaveric femurs with five different methods of fixation [6]. For the group with femurs instrumented with a hip prosthesis and an intramedullary nail, the fracture strength was the smallest among all groups (F = 3875 N ± 229 N, p = 0.01). The authors warned their readers that the use of a retrograde nail results in the highest stress riser in the femur with an existing hip prosthesis, leading to a risk for an interprosthetic fracture between the two intramedullary implants [6]. To our knowledge, these biomechanical investigations have not been extrapolated to the clinical arena, and there are no published clinical studies on this injury comparing different methods of fixation.
The concept of femoral stress risers at or near surgical implants is well documented [2,3,4, 15]. A stress-riser fracture develops when stress in an object is higher than in the surrounding material. In a sawbone analysis, Zhou et al. demonstrated that cortical perforations, nondisplaced fracture lines, bone cuts, and changes in hardness at the tip of an implant or cement are biomechanical stress risers [16]. It is conceivable that the transition zone between intramedullary implants and cortical bone is the area most at risk for fractures, especially in osteoporotic bone. In the case of a retrograde femoral nail, fractures can occur around the proximal end, typically where the interlocking screws are placed [6]. Although the precise criteria for defining a femoral stress riser are unknown, some have associated a smaller gap size between femoral implants, the length and stability of intramedullary stems, the cortical width of the femur, and implant selection as contributing factors [17, 18]. In a study looking at effect of implant overlap in the mechanical properties of the femur, Harris et al. noted that gapped implants failed at lower loads and strains than femurs with “kissing” and overlapped implants [18]. In contrast, Iesaka et al., using a composite sawbone femur model and strain-gauge testing, demonstrated that gap size did not affect the level of stress on the femur [19]. The authors noted that cortical thickness had a negative effect on stress distribution. In other words, peak stresses increased as bone cortical thickness decreased [19]. Although the sample size in our study is small and the rate of re-operation was similar between the groups, there was one refracture in the RIMN group. This was the result of a ground-level fall 82 days post-operatively and occurred at the interface between the hip stem and proximal tip of the nail. The fracture was revised with plate fixation and healed uneventfully. It is our practice to leave as small of a gap as possible between the distal THA stem and proximal tip of the nail, allowing near contact of the implants. The patient in the nailing cohort that underwent prophylactic plate fixation for mid-thigh pain in fact had a satisfactory THA stem-nail gap with “kissing” implants. The patient underwent prophylactic plating at the treating surgeon’s discretion to help minimize pain as she was a lung transplant patient on numerous immunosuppressive therapies.
Several authors advocate for plate fixation of periprosthetic and interprosthetic distal femur fractures [5, 6, 8, 17, 20, 21, 23]. In biomechanical studies, plate fixation of an interprosthetic fracture has demonstrated fracture strength similar to femurs with femoral prostheses only [8]. Plates offer the theoretical advantage of spanning the entire interprosthetic zone, effectively eliminating the remaining stress riser zones in between stiff implants [17]. In another biomechanical analysis, Dennis et al. demonstrated that plated synthetic femurs fixed with unicortical screws proximally and bicortical screws distally were most stable in axial compression, lateral bending, and torsional loading [21]. If a RIMN is chosen as the primary fixation method, some have advocated for supplementing this with a lateral locked plate to minimize the stress concentration between the hip prosthesis and proximal nail tip [22, 23]. However, there are certain disadvantages to plate fixation of periprosthetic and interprosthetic fractures. In a biomechanical analysis, Kampshoff et al. showed that bicortical screws placed through a cement mantle initiated cracks around the screw holes when using a standard drill bit [24]. Others have also expressed apprehension about plate and screw fixation in periprosthetic hip fractures, citing concerns for cement fragmentation and subsequent failure of the prosthesis [21, 25, 26]. This is a notable advantage of retrograde nailing below a hip prosthesis, as none of the interlocking screws violate the cement mantle above. Interestingly, some of the same authors who advocate plating also report successfully treating supracondylar femur fractures in the presence of an ipsilateral hip prosthesis with a RIMN, citing advantages of earlier mobilization, faster functional recovery, and rapid weight-bearing [8].
Our findings demonstrated no difference in sagittal deviation between the plate and RIMN groups, both immediately post-operatively and at final follow-up. We acknowledge that measuring sagittal alignment after a TKA can be challenging, so sagittal deviation was measured at both time intervals to assess alignment in both groups. The number of patients with sagittal malalignment > 5° was not different between the plate and RIMN groups at final follow-up. Although other studies have reported a higher rate of sagittal plane deformity with RIMN through a femoral TKA component compared with plating since the starting point is often forced posteriorly, our study found no difference between groups [27, 28]. Furthermore, Pelfort et al. found no long-term clinical significance of extension deformity malunion in the distal femur [27].There was no difference in coronal malalignment between the plate and RIMN groups immediately post-operatively. Although our study showed no difference among the groups, it is conceivable that the metaphyseal fit of a short retrograde intramedullary nail could contribute to some degree of coronal deformity or motion. This has previously been termed the “bell-clapper effect” [29]. The presence of a capacious metaphyseal segment in the distal femur may benefit from additional blocking screws that serve as “goalposts” around the retrograde nail effectively narrowing the canal. These screws provide additional stability to the metaphyseal segment and ultimately help prevent coronal deformity [29, 30] (Fig. 4). Our findings corroborate previous reports demonstrating no difference between plate fixation and RIMN in the fixation of periprosthetic distal femur fractures in either the sagittal or coronal planes at final follow-up [31].
Morbid obesity is a known risk factor for infection and complications [32, 33]. Less invasive surgical techniques are often attractive in this challenging patient population. The average patient in this study was considered “obese” as the mean BMI was 30.3 (s.d. 9.4). Nine of the 30 patients had a BMI > 35.0, consistent with “severe obesity.” Despite more obese patients in the RIMN group, we did not observe a higher rate of complications. RIMN may be appealing for this fracture in the setting of obesity.
This investigation has numerous limitations. The retrospective study design may invite selection bias. Although this is the largest case series to date, the sample size is small. Additionally, the average follow-up in the RIMN group was just over one year (367 days) with a minimum of 90-day follow-up. Longer follow-up may elucidate differences between the groups. Finally, we acknowledge that the measurement of sagittal deformity after a TKA is controversial and there may be more optimal means of measuring sagittal malalignment compared with the currently employed method of sagittal deviation.
To our knowledge, this is the first clinical study to compare RIMN versus plating in the setting of interprosthetic and periprosthetic femur fractures below a femoral stem. Previous studies in this arena have either been sawbone or cadaveric analyses with unknown clinical relevance. Based on our data, RIMN is a potentially viable option in the treatment of periprosthetic and interprosthetic femur fractures below a femoral component worthy of further study. Our results in a small cohort of patients show no differences in inpatient complications, reoperation rates, mortality, final radiographic healing, alignment, and PROs between the RIMN and plate groups. RIMN offers potential advantages of shorter surgery time and less EBL and may be an attractive option in the obese patient.
References
Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ (2016) Epidemiology of periprosthetic fracture of the femur in 32,644 primary total hip arthroplasties: a 40-year experience. Bone Joint J 98-B:461–467
Cook RE, Jenkins PJ, Walmsley PJ, Patton JT, Robinson CM (2008) Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res 466:1652–1656
Lindahl H (2007) Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury 38:651–654
Della Rocca GJ, Leung KS, Pape HC (2011) Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma 25(suppl 2):S66–S70
Rupprecht M, Schlickewei C, Fensky F, Morlock M, Püschel K, Rueger JM, Lehmann W (2015) Periprosthetic and interimplant femoral fractures: biomechanical analysis. Unfallchirurg 118(12):1025–1032
Lehmann W, Rupprecht M, Nuechtern J, Melzner D, Sellenschloh K, Kolb J, Fensky F, Hoffmann M, Püschel K, Morlock M, Rueger JM (2012) What is the risk of stress risers for interprosthetic fractures of the femur? A biomechanical analysis. Int Orthop 36(12):2441–2446
Rupprecht M, Sellenschloh K, Grossterlinden L, Püschel K, Morlock M, Amling M, Rueger JM, Lehmann W (2011) Biomechanical evaluation for mechanisms of periprosthetic femoral fractures. J Trauma 70(4):E62–E66
Lehmann W, Rupprecht M, Hellmers N, Sellenschloh K, Briem D, Püschel K, Amling M, Morlock M, Rueger JM (2010) Biomechanical evaluation of peri- and interprosthetic fractures of the femur. J Trauma 68(6):1459–1463
Unified Classification System for Periprosthetic Fractures (UCPF) (2018) J Orthop Trauma 32:S141–S144
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Brodke DJ, Saltzman CL, Brodke DS (2016) PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg 24(11):744–749
Jildeh TR, Lizzio VA, Meta F, Fidai MS, Kaat AJ, Makhni EC (2018) The correlation between PROMIS pain interference and VAS pain in ambulatory orthopedic patients. Orthopedics 41(6):e813–e819
Paley D (2002) Principles of Deformity Correction, 1st edn. Springer-Verlag Berlin Heidelberg, New York, pp 1–18
Helfet DL, Lorich DG (1998) Retrograde intramedullary nailing of supracondylar femoral fractures. Clin Orthop 350:80–84
Della Rocca GJ (2013) Periprosthetic fractures about the knee – an overview. J Knee Surg 26(1):3–7
Zhou S, Jung S, Hwang J (2019) Mechanical analysis of femoral stress-riser fractures. Clin Biomech 63:10–15
Mamczak CN, Gardner MJ, Bolhofner B, Borrelli J Jr, Streubel PN, Ricci WM (2010) Interprosthetic femoral fractures. J Orthop Trauma 24(12):740–744
Harris T, Ruth JT, Szivek J, Haywood B (2003) The effect of implant overlap on the mechanical properties of the femur. J Trauma 54(5):930–935
Iesaka K, Kummer FJ, DiCesare PE (2005) Stress risers between two ipsilateral intramedullary stems: a finite-element and biomechanical analysis. J Arthroplasty 20(3):386–391
Stoffel K, Sommer C, Kalampoki V, Blumenthal A, Joeris A (2016) The influence of the operation technique and implant used in the treatment of periprosthetic hip and interprosthetic femur fractures: a systematic literature review of 1571 cases. Arch Orthop Trauma Surg 136(4):553–561
Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE (2000) Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty 15(4):523–528
Hussain MS, Dailey SK, Avilucea FR (2018) Stable fixation and immediate weight-bearing after combined retrograde intramedullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures. J Orthop Trauma 32(6):e237–e240
Rozell JC, Delagrammaticas D, Schwarzkopf R (2019) Interprosthetic femoral fractures: management challenges. Orthop Res Rev 11:119–128
Kampshoff J, Stoffel KK, Yates PJ, Erhardt JB, Kuster MS (2010) The treatment of periprosthetic fractures with locking plates: effect of drill and screw type on cement mantles: a biomechanical analysis. Arch Orthop Trauma Surg 130(5):627–632
Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA (2006) Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma 20(2):89–93
Schmotzer H, Tchejeyan GH, Dall DM (1996) Surgical management of intra- and postoperative fractures of the femur about the tip of the stem in total hip arthroplasty. J Arthroplasty 11(6):709–717
Pelfort X, Torres-Claramunt R, Hinarejos P, Leal J, Gil-Gonzalez S, Puig L (2013) Extension malunion of the femoral component after retrograde nailing: no sequelae at 6 years. J Orthop Trauma 27(3):158–161
Service BC, Kang W, Turnbull N, Langford J, Haidukewych G, Koval KJ (2015) Influence of femoral component design on retrograde femoral nail starting point. J Orthop Trauma 29(10):e380–e384
Auston D, Donohue D, Stoops K, Cox J, Diaz M, Santoni B, Mir H (2018) Long segment blocking screws increase the stability of retrograde nail fixation in geriatric supracondylar femur fractures: eliminating the “bell-clapper effect.”. J Orthop Trauma 32(11):559–564
Virkus WW, Kempton LB, Sorkin AT, Gaski GE (2018) Intramedullary nailing of periarticular fractures. J Am Acad Orthop Surg 26(18):629–639
Matlovich NF, Langting BA, Vasarhelyi EM, Naudie DD, McCalden RW, Howard JL (2017) Outcomes of surgical management of supracondylar periprosthetic femur fractures. J Arthroplasty 32(1):189–192
Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D (2012) The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am 94(20):1839–1844
Jeschke E, Citak M, Günster C, Halder AM, Heller KD, Malzahn J, Niethard FU, Schräder P, Zacher J, Gehrke T (2018) Obesity increases the risk of postoperative complications and revision rates following primary total hip arthroplasty: an analysis of 131,576 total hip arthroplasty cases. J Arthroplasty 33(7):2287–2292
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Investigation performed at Indiana University Methodist Hospital in Indianapolis, Indiana
Rights and permissions
About this article
Cite this article
Richard, R.D., Natoli, R.M., Sorkin, A.T. et al. Retrograde intramedullary nailing below a hip arthroplasty prosthesis: a viable fixation option for periprosthetic and interprosthetic femur fractures. International Orthopaedics (SICOT) 44, 2283–2289 (2020). https://doi.org/10.1007/s00264-020-04734-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04734-3