Abstract
Introduction
The aim of this study was to describe clinical and radiological long-term results of an arthroscopic partial meniscectomy associated with an outside-in decompressive needling of the cyst for lateral parameniscal cyst.
Methods
Eighteen patients with symptomatic parameniscal cysts treated between April 2002 and September 2009 were retrospectively included in the study. All patients underwent arthroscopic partial meniscectomy (preserving peripheral rim) and needling of the cyst using a 20-gauge needle. Pre- and post-operative IKDC, Tegner, and Lysholm scores were used to evaluate clinical results. Radiological results were obtained from pre- and post-operative radiographies and post-operative MRI scans. Both supine and weight bearing MRI examinations were performed. Kellgren-Lawrence and WORMS scales were used to evaluate osteoarthritis development of the knee.
Results
The mean follow-up period was 11.6 ± 2.6 years (range 7–15). Horizontal lesions were found in 56% of patients. All patients fully recovered. Mean Lysholm scores passed from mean pre-operative value 52 ± 16.9 to post-operative 85 ± 11.9 (P < 0.01) and mean IKDC scale score changed from 49.5 ± 14.7 to 67 ± 23.5 (P < 0.01). Mean Tegner scores did not change significantly. Post-operative radiographies showed a Kellgren-Lawrence scale grade 0 in six patients (33%), a grade I in eight (44%), a grade II in three (17%), and a grade III in one patient (6%). No patients were found with a Kellgren-Lawrence scale grade IV. No significant differences with pre-operative radiographies were found (chi-square = 1.867; df = 3; P = 0.60) in osteoarthritis development of the knee. Reported WORMS scores had an average of 12.4 ± 5.1. No recurrence of any cysts was observed.
Discussion
Different treatments for lateral meniscal cysts have been proposed, but proper management of the cyst is still controversial. The results of this study suggest that the outside-in needling of the cyst associated with partial meniscectomy is a highly effective, simple, and repeatable technique. Excellent clinical outcomes were reported at a mean follow-up of 11.6 ± 2.6 years (range 7–15). Imaging evaluation showed no significant evolution to osteoarthritis of the knee.
Conclusions
Partial arthroscopic meniscectomy associated with percutaneous decompressive needling of the cyst wall under arthroscopic visualization showed positive clinical and radiological long-term results. Neither traditional radiographies nor innovative standing MRIs showed findings of osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ebner et al. [1] first described meniscal cysts 100 years ago. Nevertheless, pathogenesis and treatment of such cysts remain uncertain. Meniscal cysts are relatively uncommon, and the lateral meniscus is involved more often than medial meniscus (ratio 3:1 to 10:1) [2,3,4]. Different theories about the etiology of meniscal cysts have been proposed [4]. Embryological abnormality, infection, trauma, myxoid degeneration, and frying of the meniscus have been suggested to explain cyst origin [5, 6]. One of the most accepted theories is that meniscal cysts originate by a tear on the meniscal surface [7]. However, other authors reported the presence of meniscal cysts without an associated lesion of meniscal surface. A horizontal cleavage lesion was documented in those cases [8].
Cysts are palpable in the 40–60% of cases [3]. Sometimes they may be totally asymptomatic, especially if an associated meniscal tear is not present. However, MRI is often required for both helping diagnosis of cyst and associated menisci lesions and for choosing the proper treatment. A typical meniscal cyst appears on MRI as a fluid mass that shows fluid signal intensity on both T1- and T2-weighted sequences. Cysts are usually located close to a horizontal cleavage tear, and diagnosis is confirmed by the connection between the cyst and meniscal tear. Sometimes internal septa can be present [9].
Since the spread of the arthroscopy, several types of conservative treatments have been proposed. Partial meniscectomy is the worldwide-accepted treatment for its utility in reducing osteoarthritis development of the knee caused by total meniscectomy. Nevertheless, proper management of the cyst is still controversial. Positive results were reported by Tudisco [10] whose method involved external decompression of the cyst with a curette and a motorized instrument introduced percutaneously. Good results were shown also with an arthroscopic inside technique proposed by Howe [11]. Furthermore, fluid aspiration, open cystectomy, intra-articular decompression, and outside-in techniques are other available options [12,13,14,15,16]. Our hypothesis is that outside-in decompressive needling of the cyst, associated with partial meniscectomy, firstly proposed by Puddu et al. in 1992 [17], is an effective and repeatable technique. Moreover, the effect of an isolated partial meniscectomy on the development osteoarthritis of the knee could be assessed by the evaluation of patients treated with this surgical technique as their meniscal cysts originated in an otherwise healthy knee and subjects with other injuries of the knee were excluded. The aim of this study was to assess clinical and radiological long-term results of arthroscopic isolated partial meniscectomy and percutaneous decompressive needling for treatment of lateral meniscal cysts.
Methods
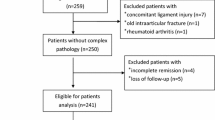
Twenty patients who underwent a knee arthroscopy for a lateral meniscal cyst from April 2002 to September 2009 were retrospectively evaluated. All cases were treated by the same surgeon with experience in knee arthroscopy. Inclusion criteria were presence of a symptomatic lateral meniscal cyst with radiological confirmation by MRI. Two patients with associated lesions (anterior cruciate ligament and/or medial meniscus injuries) were excluded. Eighteen patients were enrolled in the study. All patients gave written informed consent prior to participation in the study, which was approved by the Institutional Ethics Committee.
All patients complained of pain in the lateral joint line of the knee with a palpable cyst on the lateral side, often associated with meniscal clicking, catching, or knee effusion. Four patients (22%) reported a previous acute injury of the knee; no other cases were able to recall a traumatic event. Demographic data are shown in Table 1.
Surgical technique
The knee is in a figure of four position, and standard anteromedial and anterolateral portals were used. In all cases a tear of the lateral meniscus was reported. All meniscal tears were carefully removed by a partial meniscectomy with preservation of the external rim, and cysts were decompressed by a percutaneous needling using a 20-gauge needle, under direct arthroscpic visualization (Fig. 1). When the cyst ruptured, a clear mucinous fluid seeped from the cyst cavity. Throughout flexion and extension movements of the knee, the cysts were totally decompressed till the fluid leakage stopped. A final examination of the meniscous was carefully done. Full weight bearing was immediately permitted. Recovery of full range of motion, isometric quadriceps exercises, active leg extension, and stretching of the thigh flexor muscles were encouraged.
Clinical and radiological evaluation
Pre- and post-operative IKDC, Tegner, and Lysholm scores were used to evaluate clinical results. Radiological results were obtained from pre- and post-operative radiographies and MRI scans at final follow-up. Kellgren-Lawrence scale (grading from 0 to IV) was used to evaluate weight-bearing radiographies in antero-posterior and latero-lateral views of the knee. Post-operative MRI examinations were performed with a G-scan Esaote 0.3 Tesla scanner (ESAOTE, Genoa, Italy), in both supine and standing patient placements. The following imaging sequences were performed in weight-bearing scans: coronal X-BONE T2 and axial FSE T2-weighted. These sequences were performed in supine scans: sagittal Spin-Echo T1, coronal Gradient Echo STIR, and axial FSE T2-weighted. The Whole-Organ Magnetic Resonance Score (WORMS, ranging from 0 to 332) was used to evaluate osteoarthritis of the knee. WORMS scoring is calculated by assessment of 14 independent articular features: cartilage signal and morphology (range 0–84); subarticular bone marrow abnormality (range 0–45); subarticular cysts (range 0–45); subarticular bone attrition (range 0–42); marginal osteophytes (range 0–98); medial and lateral meniscal integrity (range 0–12); anterior and posterior cruciate ligament integrity, medial and lateral collateral ligament integrity (range 0–3); synovitis (range 0–3); and loose bodies and periarticular cysts/bursae [18]. The first five of these features were evaluated in 15 different regions of the knee, subdivided by anatomical landmarks in extended position. (Fig. 2) All pre-operative examinations and imaging analyses were performed by the senior author and an independent board-certified orthopaedic radiologist.
Statistical analysis
Mean (standard deviation) and median (range) values are presented when applicable. Statistical analyses were performed using SPSS 19.0 software (IBM). T test and chi-square test were used to assed clinical and radiological results respectively. Radiological categorical variables were expressed as percentage. P value < 0.05 was considered statistically significant. To assess the inter and intra-observer reliability, the intraclass coefficient (ICC) was calculated for the total WORMS and for Kellgren-Lawrence scores.
Results
None of the patients was lost at final evaluation. The mean follow-up was 11.6 ± 2.6 years (range 7–15). Ten patient cases involved the right knee while eight involved the left. The patient population included 13 males and five females, with a mean age at surgery of 40 ± 5.1 years (range 15–60) (Table 1). The following types of lesions were identified: 13 horizontal lesions (56%); two radial lesions (11%); four complex lesions (22%); and two discoid associated lesions (11%). Three patients presented more than a single lesion (Fig. 3).
During follow-up, no complications or recurrences of the cyst were reported. No readmissions or subsequent surgery was performed, nor were there reports of pain, catching, or instability. All patients reported being satisfied about clinical outcomes. The mean Lysholm score changed from 52 ± 16.9 to 85 ± 11.9 (P < 0.01) and the mean IKDC score from 49.5 ± 14.7 to 67 ± 23.5 (P < 0.01) (Fig. 4). The mean Tegner score did not change, but physical activity was stopped by two (11%) of 18 patients.
Pre-operative X-rays showed Kellgren-Lawrence scale grade 0 in nine patients (50%), grade I in seven (39%), and grade II in two (11%). No patients were found with a Kellgren-Lawrence grade of III or IV. Radiographies showed a post-operative Kellgren-Lawrence scale of grade 0 in six patients (33%), grade I in eight (44%), grade II in three (17%), and grade III in one patient (6%). No patients were found with a Kellgren-Lawrence scale of grade IV (Fig. 5). No significant differences between pre- and post-operative X-rays were collected (chi-square = 1.867; df = 3; P = 0.60). The ICC correlations calculated for the inter- and intra-observer reliability of the Kellgren-Lawrence score were 0.94 and 0.91 respectively. In all patients both supine and weight-bearing MRI showed no recurrence of the cyst. The reported WORMS mean score was 12.4 ± 5.1 (range 6–23), confirming the absence of degeneration of the knee. The ICC correlations calculated for the inter and intra-observer reliability of the WORMS score were 0.89 and 0.91 respectively.
Discussion
To the best our knowledge, no other studies with such a long-term follow-up are present in literature. The results of this study suggest that the outside-in needling of the cyst associated with partial meniscectomy is a highly effective, simple, and repeatable technique. Excellent clinical outcomes were reported at a mean follow-up of 11.6 ± 2.6 years (range 7–15). All patients, but two, gained a return to previous physical activity. Only two patients abandoned physical activity for other reason than clinical unsatisfaction. Radiographies showed no significant osteoarthritis of the knee. Supine and standing MRI additionally found no signs of degeneration or recurrence of the cysts.
Different theories about the etiology of meniscal cysts have been proposed [4,5,6]. One of the most accepted theories is that meniscal cysts originate by a tear on the meniscal surface. Howe at al. described the typical mechanism, where external rotation of the knee produces high stress forces on lateral meniscus which is able to damage its surface [11]. Due to a one-way valve effect of the flap, a unidirectional flow of synovial fluid from the intra-articular space to peri-articular soft tissues is generated [19]. However, other authors reported the presence of meniscal cysts without an associated lesion of meniscal surface [8]. A horizontal cleavage lesion was documented in those cases. It is thought to originate by a myxoid intra-meniscal degeneration with internal meniscus delamination [5]. A recent MRI study confirmed this theory by showing that no tear on the meniscal surface was detected by expert radiologists in 42.2% patients with a meniscal cyst [20]. Sarimo et al. [21] proposed that both trauma and intra-meniscal degeneration or a combination of both could lead to the fraying of the meniscus, even if a tear on the articular surface is not present. The delamination creates an internal horizontal cleavage tear in which synovial fluid can enter and build until a cyst is formed.
In our study, 14 patients (78%) did not report a traumatic injury of the knee. Prevalence of horizontal tears (56%) found in this study population supports the degenerative theory about cyst origin as previously reported by Barrie [4] and Glasgow [14]. The method of open meniscectomy and cystectomy, proposed for the first time in 1929 by Phenister [12], was abandoned with the introduction of arthroscopy. Arthroscopic conservative approaches for meniscal lesions are accepted worldwide as the optimal approach. By preserving a peripheral rim or suturing the lesion when possible, cartilage and bone lesions are prevented and progression to osteoarthritis is hindered. Proper treatment of cysts remains controversial and many techniques can be executed with positive results.
Recently, El Assel et al. [21] compared results of arthroscopic partial meniscectomy followed by open cystectomy or intra-articular decompression through the tear (22 patients) [22]. No significant differences between the two techniques were reported after an average follow-up period of 58 months. This result was confirmed by Sarimo et al. who compared open cystectomy and intra-articular decompression. No differences were found between two groups after an average of 33 months of follow-up.
A simple percutaneous aspiration of the cyst and injection of methylprednisolone acetate (40 mg) and bupivacaine 0.5% (1 ml) was performed in 18 patients by MacMahon et al. [15]. While this method avoided surgery and reduced the risk of long-term knee osteoarthritis, treatment failed in 33% of patients. Recurrence of symptoms or the cyst was found in five cases after an average ten months of follow-up. It suggests that treatment of meniscal tears is required to ensure positive results at a mid-term follow-up.
Glagow et al. [14] treated 69 patients with arthroscopic resection of the meniscal tear and arthroscopic decompression of the cyst by creating a hole between horizontal tear and cyst. “Good” or “excellent” results were reported in 89% of cases after an average of 34 months of follow-up. However, in this study “good” results included patients with minimal recurrence of symptoms. Furthermore, two limitations for considering the reliability of the results include the absence of a radiological evaluation and inconsistent follow-up times, which ranged from seven to 71 months.
In a recent study eight patients were treated with an arthroscopic technique [11] by the creation of a 5-mm channel through the capsule adjacent the cyst. Thus, pressure between knee and cyst was equalized and decompression of the cyst was possible. No recurrence of cysts was noted after an average follow-up of 39 months, but a larger number of patients are required to accurately define the efficacy of this technique.
A combined technique in which horizontal or radial lesions of the meniscus, or both, were arthroscopically treated, leaving a stable peripheral rim, was suggested by Tudisco et al. [10]. The cyst was decompressed from the outside-in through use of a curette and a motorized instrument introduced percutaneously. Nineteen patients were treated, and results were reported as “excellent” in eight patients, “good” in nine, and “fair” in two patients after an average of 3.3 years of follow-up. However, in this study nine of 19 patients had a very large cyst which would facilitate cyst decompression without damaging nearby tissues. Furthermore, a post-operative CT scan showed good remodeling of meniscus in ten patients. In our study a standing MRI scan was used because it was more reliable in assessing bone and soft-tissue pathology/degeneration. A summary of the results reported by various studies is shown in Table 2.
In our study the arthroscopic treatment first proposed by Puddu in 1992 [17] was used. The treatment involved a partial meniscectomy, which was careful to leave a stable peripheral rim of meniscus, followed by decompression of the cyst through percutaneous needling under arthroscopic visualization using a 20-gauge needle. Currently, no studies have been published with as long of a follow-up with the same technique as the present study.
At a long-term follow-up of 11.6 ± 2.6 years, patients showed a high level of satisfaction. No patients complained of a clinical recurrence of the cyst. The Lysholm scale score changed from 52 ± 16.9 to 85 ± 11.9 (P < 0.01) and the mean IKDC scale score passed from 49.5 ± 14.7 to 67 ± 23.5 (P < 0.01) (Fig. 4). Tegner scale score did not change, but physical activity was stopped by two patients for other reasons not correlated to the treated knee.
The most interesting data of our study is the effect of a partial isolated meniscectomy in the development of osteoarthritis in an otherwise intact knee. Our study population represents a perfect pool for this aim thanks to the exclusion criteria adopted.
Post-operative weight-bearing radiographies showed no significant osteoarthritis of the knee. A grade 0 of Kellgren Lawrence scale was reported in six patients (33%), a grade I in eight (44%), a grade II in three (17%), and a grade III in one patient (6%), with no patients presenting a grade IV (Fig. 5). Comparing with pre-operative radiographies, no significant changes were found (chi-square = 1.867; df = 3; P = 0.60), demonstrating that partial isolated meniscectomy is a safe surgical technique not associated with consistent degenerative changes in the knee. Due to the absence of other studies with the same follow-up, it is difficult to make critical comparisons and considerations.
Moreover, our study deviates from other studies in its presentation of post-operative supine and weight-bearing MRIs of the knee. Weight-bearing MRI of the knee recently proved to be a new, effective instrument in diagnosing conditions of the knee including early osteoarthritis, meniscal tear stability, or patellofemoral kinematics [23, 24]. Furthermore, the WORMS scale proved to be a valid approach to evaluating the full spectrum of knee structure and the severity of lesions related to osteoarthritis [25]. At the same follow-up, the WORMS mean value was 12.4 ± 5.1 (range 6–23). Even if no other similar studies are present in literature and no controlateral knee has been studied at MRI, our results seem to confirm the good clinical and radiological outcomes in the study population treated with this surgical technique.
Limitations of the study included the number of patients admitted to the study and the absence of comparison to other surgical treatments; given the long-term follow-up and innovative radiological technique, however, the decreased power generated by low enrolment was likely mitigated. The use of a 0.3 Tesla MRI is another limitation of the study. More powerful Tesla scanners may better investigate changes of the articular environment in osteoarthritis. However, the weight-bearing position represents a new interesting approach in evaluation of osteoarthritis of the knee, able to likely compensate this limitation. Furthermore, not only at the time of the study but also nowadays, not many studies with a powerful weight-bearing MRI scanners are present in literature.
This study had two strengths: the long-term follow-up period and the use of weight-bearing MRI for radiological evaluation.
Conclusion
Partial arthroscopic meniscectomy associated with percutaneous decompressive needling of the cyst wall under arthroscopic visualization showed positive clinical and radiological long-term results with no recurrence of the cyst. Horizontal lesions were found in the most of patients, which supports a degenerative model of cyst origin. Neither traditional radiographies nor innovative standing MRIs showed findings of osteoarthritis.
References
Ebner A (1904) Einfall von ganglionamkniegelenks-meniskus. MuenchererMed Wochenschr 51:1737–1739
Hulet C, Schiltz D, Locker B, Beguin J, Vielpeau C (1998) Lateral meniscal cyst. Retrospective studey of 105 cysts treated with arthroscopy with 5 year follow-up. Rev Chir Orthop Reparatrice Appar Mot 84(6):531–538
Campbell SE, Sanders TG, Morrison WB (2001) MR imaging of meniscal cysts: incidence, location, and clinical significance. AJR Am J Roentgenol Aug 177(2):409–413
Barrie HJ (1979) The pathogenesis and significance of meniscal cyst. J Bone Joint Surg (Br) 61-B:184–189
Ferrer-Roca O, Vilalta C (1980) Lesions of the meniscus. Part II: Horizontal cleavages and lateral cysts. Clin Orthop Relat Res (146):301–307
Ferrer-Roca O, Vilalta C (1980) Lesions of the meniscus. Part I: Macroscopic and histologic findings. Clin Orthop Relat Res (146):289–300
Crowell MS, Westrick RB, Fogarty BT (2013) Cysts of the elateral meniscus. Int J Sports Phys Ther 8(3):340–348
Reagan WD, McConkey JP, Loomer RL et al (1989) Cysts of the lateral meniscus: arthroscopy versus arthroscopy plus open cystectomy. Arthroscopy 5:274–281
Tyson LL, Daughters TC Jr, Ryu RK, Crues JV III (1995) MRI appearance of meniscal cyst. Skelet Radiol 24(6):421–424
Tudisco C, Meo A, Blasucci C, Ippolito E (2000) Arthroscopic treatment of lateral meniscal cysts using an outside-in technique. Am J Seports Med 28(5):683–686
Howe TS, Koh JS (2007) Arthroscopic internal marsupiaelization of meniscal cysts. Knee 14(5):408–410
Phemister D (1923) Cysts of the external semilunar cartilage of the knee. J Am e Assoc 80:593–595
Flynn M, Kelly JP (1976) Local excision of cyst of lateral meniscus of knee without recurrence. J Bone Joint Surg (Br) 58-B:88–89
Glasgow MM, Allen PW, Blakeway C (1993) Arthroscopic treatment of cysts of the lateral meniscus. J Bone Joint SurgBr 75(2):299–302
Macmahon PJ, Brennan DD, Duke D, Forde S, Eustace SJ (2007) Ultrasound-guided percutaneous drainage of meniscal cysts: preliminary clinical experience. ClinRadiol 62(7):683–687
Passler JM, Hofer HP, Peicha G, Wildburger R (1993) Arthroscopic treatment of meniscal cysts. J.Bone Joint Surg Br 75(2):303–304
Cipolla M, Cerullo G, Puddu G (1992) Microvasculature of the human medial meniscus: operative findings. Arthroscopy. 8(4):522–525
Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, Kothari M, Lu Y, Fye K, Zhao S, Genant HK (2004) Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage 12(3):177–190
Parisien JS (1990) Arthroscopic treatment of cysts of the menisci. A preliminary report ClinOrthop 257:154–158
Anderson JJ, Connor GF, Helms CA (2010) New observations on meniscal cysts. SkeletalRadiol 39(12):1187–1191
Sarimo J, Rainio P, Rantanen J, Orava S (2002) Comparison of two procedures for meniscal cysts. A report of 35 patients with a mean follow-up of 33 months. Am J Sports Med 30(5):704–707
El-Assal M, Mostafa M, Abdel-Aal A, El-Shafee M (2003) Arthroscopy alone or in association with open cystectomy:in treatment of lateral meniscal cysts. Knee Surg Sports Traumatol Arthrosc 11(1):30–32
Barile A, Conti L, Lanni G, Calvisi V, Masciocchi C (2013) Evaluation of medial meniscus tears and meniscal stability: weight-bearing MRI vs arthroscopy. Eur J Radiol 82:633–639
Bruno F, Barile A, Arrigoni F, Laporta A, Russo A, Carotti M, Splendiani A, Di Cesare E, Masciocchi C (2018) Weight-bearing MRI of the knee: a review of advantages and limits. Acta Biomed 89(1-S):78–88
Wegrzyn J, D’Apuzzo MR, Amrami KK, Larson DR, Kaufman KR (2012) Could Whole-Organ Magnetic Resonance Imaging Score (WORMS) components predict pain in knee osteoarthritis? Motion Analysis Laboratory, Mayo Clinic, Rochester, MN, 2 Radiology, Mayo Clinic, Rochester, MN, 3 Biostatistics, Mayo Clinic, Rochester
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients gave written informed consent prior to participation in the study, which was approved by the Institutional Ethics Committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iorio, R., Mazza, D., Drogo, P. et al. Lateral meniscal cysts: long-term clinical and radiological results of a partial meniscectomy and percutaneous decompressive needling. International Orthopaedics (SICOT) 44, 487–493 (2020). https://doi.org/10.1007/s00264-019-04446-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04446-3