Abstract
Purpose
Incorrect positioning of components during total knee arthroplasty (TKA) increases the risk of pain, instability, and early revision. The purpose of this study was to compare 3D planning-assisted and a conventional system for TKA positioning. We hypothesized that the use of three-dimensional CT-scan planning and custom cutting guides would increase the accuracy of component positioning.
Methods
A randomized, controlled, prospective study of two groups was performed. In one group, patient-specific custom cutting guides (PSCG) were used for component positioning based on 3D CT-scan planning. In the control group, TKA was performed with a conventional ancillary system. The components’ positioning angles were measured on 3D reconstructions. The main evaluation criterion was the percentage of outliers outside of a target zone of ± 3° for the coronal positioning of the femoral component.
Results
Eighty patients were included. The percentage of outliers for the femoral component was significantly lower in the 3D-guided group (1 patient) compared to the control group (7 patients p = 0.02). The coronal femoral angle was restored with greater accuracy in the 3D-assisted group (− 0.1° ± 1.4°) compared to the control group (1.6° ± 2.5°). Surgery was significantly shorter in the 3D group. The clinical outcomes were better in the 3D group at the two year follow-up with fewer failures and a lower standard deviation in IKS scores.
Conclusion
The use of a 3D planning and custom guides can improve TKA component positioning by increasing the accuracy of implants alignment and reducing the percentage of outliers. The same benefit was not demonstrated for the global knee alignment and the clinical scores with no indisputable clinical advantage for the PSCG.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malalignment after total knee arthroplasty (TKA) has been shown to play a role in several complications including pain and a higher rate of revision [1,2,3]. Conventional 2D planning–based systems are still the most frequently used techniques for component positioning. Although the average reported rates of knee alignment are satisfactory, 8 to 46% of patients may have an alignment that is outside the conventional − 3°/+ 3° range [4,5,6]. The mean accuracy (percentage of patients within ± 3°) of component positioning in the literature with conventional ancillary systems is 85% (77–96%) for the femoral prosthesis and 96% (90–98%) for the tibial plateau [4, 5, 7,8,9,10,11] suggesting that the weak point of conventional ancillary systems concerns the femoral component alignment. This lack of accuracy can be critical because the mean rotation axis may not be restored resulting in stiffness or pain.
Patient-specific custom guides (PSCG) have been developed to improve the accuracy and reproducibility of 3D-component positioning. Results of these guides vary, with some studies showing no improvement in knee alignment [9]. However, PSCG designs and techniques differ, with some using MRI and others CT, with poorer results for the MRI-based guides [9, 12]. The bone segmentation used to generate the 3D surface models plays a major role in the accuracy of these techniques.
Although Franceschi et al. [13] recently showed that a specific PSCG associating tripod support and an anterior cortical marker was highly reliable and accurate, there are no comparative randomized controlled studies confirming the efficacy of this system. The goal was to compare the accuracy of knee reconstruction with 3D planning and with conventional 2D planning–assisted TKA. We hypothesized that the use of preoperative 3D planning with CT-scan and this PSCG system would increase the accuracy of knee reconstruction during TKA.
Material and methods
Subjects
A prospective, randomized, controlled study was performed from January 2012 to December 2014. The study protocol and consent forms were approved by the local ethics committee. The trial was registered at the ANSM registry with the BRC identification number 2015-A01841-48. Consort guidelines were added as additional material.
Criteria for inclusion in the study were patients who underwent primary TKA by anteromedial approach with the same surgeon using a cemented postero-stabilized prosthesis (FIRST®, Symbios, Yverdon, Switzerland). Exclusion criterion was revision knee surgery. Patients were randomized by the clinical research department using a systematic sampling method, including blocked randomization with a block size of four. Two patients in each block were assigned to procedure-1 (2D planning with a conventional ancillary system) and two were assigned to procedure-2 (CT-scan-based 3D planning with PSCG) (Fig. 1). All patients provided informed consent to participate in the study. The senior surgeon had more experience with the conventional technique. This study included his learning curve with the 3D planning and the PSCG.
Three-dimensional pre-operative planning
CT-scan-based 3D planning and simulation surgery with Knee-Plan® (Symbios, Switzerland) software [13] was performed in each patient to analyze the 3D knee anatomy and to plan component size and position.
The real 3D positions of the hip, knee, and ankle rotation centers were determined to determine the mechanical axis of the femur and the tibia. Spheres were used to identify the centre of the femoral head (H). Then, the centre of the knee (K) was considered to be the intersection between the Blumensaat line and the Whitside line. Finally, the middle of the talus dome was used as the centre of the ankle (A) (Fig. 2).
The knee rotation axis was determined by the line joining the lateral epicondyle (El) to the medial epicondyle (Em), and we used the surgical bi-epicondylar axis. In order to measure the tibia rotation, the centres of the two tibial plateaus were determined on the axial view passing 10 mm under the lateral plateau, then the antero-posterior axis was defined as the orthogonal to the line joining these two centres. Two Cartesian referentials were determined. First, the femoral frame was defined as the plane passing through the femoral mechanical axis (H-K) and parallel to the bi-epicondylar line (El-Em) (Fig. 3). The tibial frame was defined as the plane passing through the tibial mechanical axis (K-A) and orthogonal to the line joining the centres of the pre-spinal and the retro-spinal surfaces of the tibia (Fig. 4).
The guidelines for 3D planning included (1) a tibial cut orthogonal to the tibial mechanical axis, (2) restoration of tibial rotation and slope, (3) restoration of the average knee rotation axis corresponding to the bi-epicondylar axis (El-Em) on both the axial and coronal planes.
Afterward, a fine tuning for tibial plateau positioning was performed during the 3D planning in order to avoid an oversizing with a risk of soft tissue impingement, especially on the postero-lateral side.
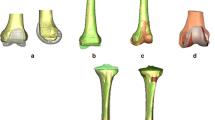
Component sizes and positions were determined to meet requirements and to place them in the capsular envelope. Components were controlled by 3D visualization to avoid oversizing and anterior femoral notching (Figs. 4 and 5). In this purpose, the sagittal alignment of the femoral component was adapted to minimize both of these two risks. This sagittal alignment was a compromise between the notch risk induced by a high femoral shield extension and a prosthesis-soft-tissue impingement risk induced by a high femoral shield flexion.
PSCG associating a tripod support and an anterior cortical marker was designed using the 3D-planning results and specific software (BoneSurfacer®, Symbios, SA). The 3D tibial custom-made cutting blocks indicated the tibial rotation angle and the tibial slope.
2D planning methodology
The conventional group did not undergo pre-operative CT scan. Planning in the 2D group was based on full leg standing radiographs. The centres of the femoral head (H), knee (K) and the ankle (A) were determined on the X-rays. Cuts were orthogonal to the mechanical axes. The angle between the distal femoral anatomical axis and the femoral mechanical axis was measured to guide the distal femoral cut during surgery using the conventional ancillary system that included an intramedullary guidance system for the femur and an extra-medullary device for the tibia. The femoral component was implanted aligned with the bi-epicondylar axis. However, this axis may be difficult to visualize at the time of surgery, especially in obese patients. In this case, the surgeon checked the alignment using a device that gives a 3° external rotation reference relatively to the bicondylar plane.
Post-operative evaluation (Fig. 6)
All patients underwent post-operative low dose CT scan three months after surgery to compare the final position to the planned position of the implants.
The following parameters were measured (Fig. 6): (1) α: the coronal femoral mechanical angle corresponding to the angle between the tangent to the distal condyles of the femoral shield and the HK mechanical axis measured on the coronal femoral plane; (2) β: the angle between the bi-epicondylar axis and the bicondylar plane measured on the axial plane; (3) γ: the sagittal tilt of the femoral component; (4) δ: the tibial mechanical angle corresponding to the angle between the tibial plateau and the KA mechanical axis measured on the coronal tibial plane; (5) ε: the tibial component rotation angle on the axial plane; (6) θ: the tibial slope.
To compare the planned components, position to the final position, we matched pre-operative and post-operative CT scans with KNEE-PLAN® software by aligning the bone landmarks (Fig. 7). Excellent agreement has been reported for the reproducibility of these angular measurements [13].
A matching of the pre-operative (green) and the post-operative (gray) CT-scan was performed by aligning anatomic landmarks of the femur and the tibia. The positioning angular parameters were measured in the same Cartesian referential. a Coronal reconstruction, b sagittal reconstruction, c axial view
Full leg radiographs were performed at 3 months follow-up in order to analyze the final HKA angles in all patients.
Evaluation criteria
The main evaluation criterion was the percentage of outliers for coronal femoral component alignment who were outside the − 3°/+ 3° range from the planned angular value. Secondary evaluation criteria included:
- 1.
Accuracy of restoration of component positioning angles and 3D knee alignment.
- 2.
The percentage of outliers for the components alignment and HKA angle who were outside the − 3°/+ 3° range.
- 3.
The operating time.
- 4.
The clinical outcomes at two years of follow-up using the International Knee Society score [14] (IKS).
One independent person not involved in the surgical procedures performed the radiographic measurements. He was blinded to the intervention and not a part of the surgical team.
Statistical analysis
According to the literature [4, 5, 7, 8, 10, 15], the mean rate of outliers for femoral component positioning is 15% (4 to 23%). The sample size was 37 patients per group based on an expected percentage of outliers of 15% in the 2D group and 5% in the 3D group with a power of 1-β = 0.80 and a type I error rate of α = 0.05. Forty patients were included in each group to take into account the risk of lost to follow-up patients.
The accuracy of both methods was analyzed by a two-group pair comparison of the planned and post-operative positioning angles. Means and variances of the component positions obtained with 3D planning were compared to those obtained with the conventional method. The accuracy of angle restoration between the planned position and the final position was expressed as the mean difference ± standard deviation. The Pearson coefficient (r) was used to evaluate the correlation between the planned and post-operative position angles. We then determined the percentage of components outside the target-zone (outliers ± 3° from the planned angular value) in each group. The percentage of outliers was compared between groups using a chi-square test. Statistical analysis was performed with JMP software (version 11; SAS Institute) (Table 3).
All the results were fully blinded in relation to the groups. All patients were blinded to the randomization results.
Results
Forty consecutive patients were included in each group (Fig. 1). There were no significant differences in the demographic data between the two groups except for gender (Table 1). Patients were a mean 67.7 ± 8.7 years old in the 3D group and 68.9 ± 9.2 in the conventional group. The mean body mass index was 29.7 ± 5.3 in the 3D group and 29.5 ± 4.5 in the conventional group. Aetiologies in the 3D group were primary osteoarthritis in 37 knees, rheumatoid polyarthritis in two knees, and osteonecrosis in one knee and primary osteoarthritis in 38 knees and rheumatoid polyarthritis in two knees in the conventional group. The mean pre-operative HKA angle was 178.5° ± 8° and 179.3° ± 8.8° in the 3D and conventional groups, respectively.
Main evaluation criteria
The percentage of outliers was significantly lower in the 3D group than in the conventional group for the femoral coronal angle α (1 vs 7 patients, p = 0.02) and the axial angle β (2 vs 8 patients, p = 0.04) (Table 3).
Accuracy of knee reconstruction
In the 3D-guided group, there was no significant difference between the mean planned and post-operative femoral component positioning angles on the coronal plane (α) (91° ± 1.4° vs 91° ± 1.7°, p = 0.8), axial plane (β) (89.8° ± 1.8° vs 90°, p = 0.5), or sagittal plane (γ) (94.4° ± 2.9° vs 95.3° ± 3.9°, p = 0.3), and strong correlations between these two values were found for both α (0.62, p = 0.0001) and β (0.62, p = 0.0001). On the other hand, in the conventional group, the mean postoperative femoral component coronal α angle was significantly higher (91.6 ± 2.5°) than the mean planned values (90°, p < 0.0001). Results are summarized in Tables 2 and 3.
The accuracy of restoration of the coronal femoral angle (α) was significantly better in the 3D-guided group (− 0.1° ± 1.4) than in the conventional group (1.6° ± 2.5°, p < 0.0001). The standard deviations of the femoral angles were significantly lower in the 3D group than in the conventional group on both the coronal (p = 0.0007) and the axial planes (p = 0.01) (Fig. 8).
There was no significant difference between the mean planned and post-operative tibial component positioning angles in the 3D group. On the other hand, in the 2D group, the final sagittal tibial angle θ was significantly higher (87.4° ± 2.8°) than the mean planned values (84.8° ± 2.8 °, p < 0.0004). The tibial standard deviations were significantly lower in the 3D group than in the conventional group on both the coronal (p = 0.04) and the sagittal planes (p = 0.01).
There was no significant difference between the mean planned and postoperative HKA angles in either group. There was no significant difference in the percentage of HKA outliers between the 3D group (four, 10%) and the conventional group (eight, 20%, p = 0.2).
Operating time
The operating time was significantly shorter in the 3D group (85.4 min ± 11.7) than in the conventional group (91 min ± 10.3, p = 0.03).
Clinical outcomes
At the two year follow-up, two patients had undergone revision TKA in the conventional group: one patient for early femoral component loosening and one for TKA malalignment with 7° valgus associated with pain in the medial collateral ligament. One patient in the conventional group underwent knee manipulation under general anaesthesia for stiffness 45 days after surgery. There were no revisions and no manipulations in the 3D group.
Although there was no significant difference in the IKS score between the 3D group (191.5° ± 20°) and the conventional group (184° ± 30.5°, p = 0.2) at the two year follow-up, the standard deviation was significantly lower in the 3D group (p = 0.01) (Fig. 9). At two years follow-up, there was no significant difference in the mean Flexion between the 3D group (122° ± 12°) and 2D group (118 ± 16°, p = 0.1).
Discussion
The main finding of this study was that our technique of 3D-planning-assisted TKA was more accurate than conventional 2D-planning-assisted TKA for the coronal and axial positioning of the femoral shield and the sagittal placement of the tibial component. This higher accuracy allowed a more accurate restoration of the mean flexion-extension rotation axis that is imposed by the femoral component position. However, there was no significant difference in global HKA coronal alignment, suggesting no indisputable clinical advantage for the PSCG with regard to the lower limb alignment.
The percentage of outliers was significantly lower in the 3D group than in the conventional group for femoral component positioning. Although there was no significant difference in the percentage of HKA outliers between the two groups, there was a tendency for less HKA outliers in the 3D group. Based on an expected percentage of HKA outliers of 20% in the 2D group and 10% in the 3D group, as we found, 195 patients would be needed in each group to determine a significant difference. A more powerful controlled study including more patients is needed to investigate a theoretical improvement in the outlier’s rate for global knee alignment.
Our results confirm certain previous studies that showed that the PSCG were more accurate than conventional ancillary systems for the femoral components’ positioning. Positioning of the femoral component was found to be more accurate with PSCG in a study by De Vloo et al. [16] with less variability in the accuracy of positioning for femoral flexion and tibial rotation. In the meta-analysis by Thienpont et al. [15], the use of a PSCG was shown to improve the accuracy of the femoral component and global alignment although the rate of outliers for the tibial component was increased.
Unlike some meta-analyses [15], most published studies [4, 7,8,9,10,11] have failed to show any improvement in global knee alignment with PSCG. However, most of them included small cohorts. Furthermore, these studies did not adapt the parameters of knee reconstruction to patient morphotypes. Indeed, most PSCG are designed with standard guidelines including orthogonal cuts and 3° of external axial rotation for the femur. However, these goals may be impossible to achieve during surgery because of ligament balancing. Moreover, very few studies assessed the actual 3D component positions by CT-scan and were only based on leg X-rays. Finally, the failure rate of most MRI-based PSG was higher and 16 to 22% of procedures were abandoned, confirming the central role of the technology used for bone segmentation [9, 12].
There was no significant difference in the mean IKS scores between the two groups. Nevertheless, the clinical outcomes at the two year follow-up were slightly better in the 3D group, with a significantly lower standard deviation in IKS scores. Furthermore, unlike the 3D group, two patients were revised in the 2D group. However, this clinical improvement remains questionable given the low number of patients and the lack of statistical power, especially since this technique generates additional costs.
Recently, Abane et al. [17] reported that the use of PSCG improves neither the alignment nor the clinical outcomes after TKA. Similar results were also found by Kosse et al. [18]. Anderl et al. [19] found that 3D-component positioning outliers were significantly lower in the PSI. Interestingly, clinical outcome was comparable between the two instrumentation groups, significantly inferior outcome was detected in the subgroup of HKA outliers suggesting that PSI helped in improving the outcomes following TKA.
This study has some strong points. It is a controlled comparative randomized trial with blinded analysis of results. None of the patients was lost to follow-up and 3D reconstruction was assessed in all patients.
Moreover, we matched the pre-operative and post-operative CT scans, reducing the risk of measurement errors related to knee position on X-rays.
Our paper also has certain limitations. In particular, all patients were operated upon by the same surgeon. Thus, it would be interesting to perform this study with different surgeons with different levels of expertise.
Another limitation was that no cases with severe bone deformity such as major intra-osseous deformity (Blount disease or fracture sequela) were found in this study. It would be interesting to perform a study to assess the value of the PSCGs in these difficult cases.
3D-planning-based TKA reduced the surgical time by 5.7 min, results which have also been reported by other authors [5, 15]. However, this is a minor reduction.
The 3D planning may help in adapting the implants’ positioning according to the knee morphotype. Indeed, many authors suggested the use of a kinematical alignment in order to improve the early clinical outcomes [20].
PSCG allowed a more accurate femoral component positioning. However, it is still unclear whether this accuracy may improve the long-term outcomes as suggested by the long-term follow-up studies of navigated TKA that failed to show clear clinical advantage for navigation despite its higher alignment accuracy comparatively to conventional techniques [21]. Other factors such as bone quality and fixation mode should be included at the time of the 3D planning.
Conclusion
The present technique of pre-operative CT-scan based 3D-planning combined with specific PSCG can improve component alignment in TKA by increasing the accuracy of component positioning and reducing the percentage of outliers for the femoral component. The same benefit was not found for global knee alignment. Better clinical outcomes were identified in the 3D group at the two year follow-up with fewer failures and a lower standard deviation for the IKS scores.
References
Baker PN, Petheram T, Avery PJ, Gregg PJ, Deehan DJ (2012) Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg Am 94:e126. https://doi.org/10.2106/JBJS.K.00791
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97:715–720. https://doi.org/10.2106/JBJS.M.01534
Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J (2012) Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1049–1056. https://doi.org/10.1007/s00167-011-1624-8
Boonen B, Schotanus MG, Kerens B, Hulsmans FJ, Tuinebreijer WE, Kort NP (2015) Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-015-3661-1
Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C (2013) A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J 95-B:354–359. https://doi.org/10.1302/0301-620X.95B3.29903
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 89:236–243. https://doi.org/10.2106/JBJS.F.00386
Hamilton WG, Parks NL (2014) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplast 29:1508–1509. https://doi.org/10.1016/j.arth.2014.01.029
Marimuthu K, Chen DB, Harris IA, Wheatley E, Bryant CJ, MacDessi SJ (2014) A multi-planar CT-based comparative analysis of patient-specific cutting guides with conventional instrumentation in total knee arthroplasty. J Arthroplast 29:1138–1142. https://doi.org/10.1016/j.arth.2013.12.019
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2014) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 472:263–271. https://doi.org/10.1007/s11999-013-2997-4
Woolson ST, Harris AH, Wagner DW, Giori NJ (2014) Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Joint Surg Am 96:366–372. https://doi.org/10.2106/JBJS.L.01722
Yau WP, Chiu KY, Zuo JL, Tang WM, Ng TP (2008) Computer navigation did not improve alignment in a lower-volume total knee practice. Clin Orthop Relat Res 466:935–945. https://doi.org/10.1007/s11999-008-0144-4
Roh YW, Kim TW, Lee S, Seong SC, Lee MC (2013) Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of one system. Clin Orthop Relat Res 471:3988–3995. https://doi.org/10.1007/s11999-013-3206-1
Franceschi JP, Sbihi A, Computer Assisted Orthopedic Surgery F (2014) 3D templating and patient-specific cutting guides (knee-plan) in total knee arthroplasty: postoperative CT-based assessment of implant positioning. Orthop Traumatol Surg Res 100:S281–S286. https://doi.org/10.1016/j.otsr.2014.04.003
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 13–14
Thienpont E, Schwab PE, Fennema P (2017) Efficacy of patient-specific instruments in total knee arthroplasty: a systematic review and meta-analysis. J Bone Joint Surg Am 99:521–530. https://doi.org/10.2106/JBJS.16.00496
De Vloo R, Pellikaan P, Dhollander A, Vander Sloten J (2017) Three-dimensional analysis of accuracy of component positioning in total knee arthroplasty with patient specific and conventional instruments: a randomized controlled trial. Knee 24:1469–1477. https://doi.org/10.1016/j.knee.2017.08.059
Abane L, Zaoui A, Anract P, Lefevre N, Herman S, Hamadouche M (2018) Can a single-use and patient-specific instrumentation be reliably used in primary total knee arthroplasty? A multicenter controlled study. J Arthroplast 33:2111–2118. https://doi.org/10.1016/j.arth.2018.02.038
Kosse NM, Heesterbeek PJC, Schimmel JJP, van Hellemondt GG, Wymenga AB, Defoort KC (2018) Stability and alignment do not improve by using patient-specific instrumentation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 26:1792–1799. https://doi.org/10.1007/s00167-017-4792-3
Anderl W, Pauzenberger L, Kolblinger R, Kiesselbach G, Brandl G, Laky B, Kriegleder B, Heuberer P, Schwameis E (2016) Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA. Knee Surg Sports Traumatol Arthrosc 24:102–111. https://doi.org/10.1007/s00167-014-3345-2
Keshmiri A, Maderbacher G, Baier C, Benditz A, Grifka J, Greimel F (2018) Kinematic alignment in total knee arthroplasty leads to a better restoration of patellar kinematics compared to mechanic alignment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5284-9
d'Amato M, Ensini A, Leardini A, Barbadoro P, Illuminati A, Belvedere C (2018) Conventional versus computer-assisted surgery in total knee arthroplasty: comparison at ten years follow-up. Int Orthop. https://doi.org/10.1007/s00264-018-4114-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Intellectual property rights: royalties from Symbios SA.
Ethical approval
The study was approved by the local ethical committee.
Informed consent
All of the patients provided informed consent to participate in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Therapeutic Level I.
Rights and permissions
About this article
Cite this article
Sariali, E., Kajetanek, C. & Catonné, Y. Comparison of custom cutting guides based on three-dimensional computerized CT-scan planning and a conventional ancillary system based on two-dimensional planning in total knee arthroplasty: a randomized controlled trial. International Orthopaedics (SICOT) 43, 2529–2538 (2019). https://doi.org/10.1007/s00264-019-04357-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04357-3