Abstract
Purpose
It is unclear whether the minimally invasive navigation-assisted (MINA) or conventional (CONv) approach for primary total knee arthroplasty (TKA) leads to better clinical and radiographic outcomes. This meta-analysis compared the clinical and radiographic outcomes of the MINA and CONv approaches after primary TKA. It was hypothesized that there was no difference in clinical and radiographic outcomes between the two surgical approaches for primary TKA.
Methods
This meta-analysis reviewed all studies that compared surgical time, incision length, flexion range of motion (ROM), Knee Society Score (
KSS), coronal mechanical axis (CMA), and coronal femoral component angle (CFCA) with various measurement tools, from direct interview to plain radiography, between the MINA and CONv approaches.
Results
Five studies met the inclusion/exclusion criteria for the meta-analysis. The findings of this study suggest that surgical time (95 % CI −18.51 to 39.09; n.s.), KSS (95 % CI −8.55 to 30.84; n.s.), CMA (95 % CI −1.01 to 0.54; n.s.), and CFCA (95 % CI −0.91 to 2.97; n.s.) were similar between the two surgical approaches, whereas incision length (95 % CI −5.18 to −3.69; P < 0.001) was significantly shorter in the MINA approach and flexion ROM (95 % CI 14.26–19.01; P < 0.001) was significantly greater in the MINA approach.
Conclusions
There were no significant differences in clinical and radiographic outcomes, including surgical time, KSS, CMA, and CFCA, in patients who underwent MINA and CONv approach for primary TKA, but the MINA approach resulted in a slightly shorter incision length and increased flexion ROM than the CONv approach. Therefore, if particular attention has to be paid to patient’s selection with appropriate counselling and surgeon’s experience, MINA approach can provide early clinical benefit when compared with CONv approach. Besides, orthopaedic surgeons need to master the MINA and CONv approaches because both approaches have similar clinical and radiographic outcomes.
Level of evidence
Therapeutic study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The conventional (CONv) approach for primary total knee arthroplasty (TKA) reportedly yields excellent long-term outcomes [3, 16]. Despite the widespread use of the CONv approach, this technique may result in a significantly decreased extensor mechanism caused by extensive surgical exposure of the operative region, delaying functional recovery and rehabilitation. Various minimally invasive approaches, including mini-medial parapatellar, midvastus, subvastus, and quadriceps-sparing approaches, have been developed to avoid these complications [4, 10, 17, 26]. Studies have shown that minimally invasive approaches lead to less pain perioperatively and earlier improvement of range of motion (ROM) than the CONv approach [1, 4, 21]. However, they also have disadvantages, including difficulties restoring the leg axis and an increased risk of component malalignment due to reduced visualization of critical anatomic landmarks [7, 24]. By combining navigation-assisted and minimally invasive techniques, accurate component and limb alignment can be achieved without compromising surgical access [6, 11, 20, 22, 28]. However, such studies included only a small sample size, which can lead to reducing statistical power, difficulty in detecting a statistical difference, and less precision. To date, few studies have compared clinical and radiographic outcomes directly between the MINA and CONv approaches in primary TKA. Additionally, no similar systematic reviews or meta-analysis on this subject have been published with conclusive results. It is unclear which surgical approach achieves better clinical and radiographic outcomes.
This meta-analysis compared clinical and radiographic outcomes in patients treated with the MINA or CONv approach for primary TKA. It was hypothesized that there was no difference in clinical and radiographic outcomes between the two surgical approaches for primary TKA.
Materials and methods
Data and literature search
This study was based on the Cochrane Review Methods [14]. Multiple comprehensive databases, including MEDLINE (1 January 1976 to 30 June 2015), EMBASE (1 January 1985 to 30 June 2015), Cochrane Library (1 January 1987 to 30 June 2015), and KoreaMed (1 June 1958 to 30 June 2015), were searched for studies that compared clinical and radiographic outcomes of the MINA and CONv approaches for primary TKA within relevant randomized controlled trials (RCTs) or quasi-randomized controlled trials (qRCTs). CENTRAL (Cochrane Central Register of Controlled Trials) including some Regional Library of Medicine with several different language databases was searched. But because CENTRAL did not include Korean database, we searched Korean database separately. Moreover, additional MEDLINE and EMBASE searching were performed due to 2- to 5-month or 1- to 2-year time lag between indexing of MEDLINE or EMBASE records and inclusion in CENTRAL, respectively. Searches were not restricted by language or year of publication. Search terms used in the title, abstract, and keywords fields included (‘minimally invasive surgical procedures’ [Mesh] OR ‘surgery, computer-assisted’ [Mesh] OR ‘arthroplasty, replacement, knee’ [Mesh] OR ‘total knee arthroplasty’ [tiab] OR ‘total knee replacement’ [tiab]) AND ‘minimally invasive surgery’ [tiab] OR ‘computer-assisted surgery’ [tiab] OR ‘navigation-assisted surgery’ [tiab] OR ‘less invasive’ [tiab]. After the initial electronic search, we also performed a hand search for articles that were potentially missed by the electronic search.
Study selection
From the title and abstract, two reviewers independently selected relevant studies for full review. Each reviewer sorted one database, which in turn was validated by the other reviewer. The full text copy of the article was reviewed if the abstract did not provide enough data to make a decision. Studies were included in the meta-analysis if they (1) were prospective RCTs or qRCTs. A quasi-randomized study utilizes a quasi-random method of allocating participants to different interventions, for instance allocation by date of birth or hospital record number or alternation [2]. (2) Included patients treated with the MINA and CONv approaches for primary TKA. A minimally invasive approach was defined as an approach with a skin incision of <14 cm and termed as a minimally invasive approach by the authors. Otherwise, it was defined as conventional approach. (3) Reported direct comparisons for at least one parameter related to surgical outcomes, including surgical time, incision length, flexion ROM, Knee Society Score (KSS), coronal mechanical axis (CMA), and coronal femoral component angle (CFCA). The CMA was defined as the angle subtended by a line drawn from the centre of the femoral head to the centre of the knee and a line drawn from the centre of the knee to the centre of the talus on a standing AP lower limb radiograph. A negative value denotes valgus angulation, whereas a positive value denotes varus angulation. The CFCA was defined as the angle between the MA of the femur and the transcondylar line of the femoral component. A value >90° denotes varus angulation, whereas a value <90° denotes valgus angulation. Other inclusion criteria were that the study (4) fully reported clinical and radiographic outcomes, including means and standard deviations and sample numbers, and (5) used adequate statistical methods to compare the amount and proportion of clinical and radiographic outcomes between the MINA and CONv approaches.
Data extraction
Two reviewers independently recorded data from each study using a predefined data extraction form. Disagreement between the reviewers was resolved by consensus or by discussion with a third investigator when a consensus was not reached. Variables recorded included those associated with surgical outcomes, such as surgical time, incision length, flexion ROM, KSS, CMA, and CFCA. Sample size and the means and standard deviations of surgical outcomes in each group were also recorded. If these variables were not mentioned in the articles, the study authors were contacted to retrieve further information.
Assessment of methodological quality
Two reviewers independently assessed the methodological quality of each study using the risk of bias table, including rating of the randomization procedure; allocation concealment; blinding of patients, surgeons, and outcome assessors; selective outcome reporting; and incomplete outcome data, as recommended by the Cochrane Bias Methods Group. An independent judgement by the two first authors of high, low, or unclear risk of bias was made. Additionally, modified Jadad scale was applied to evaluate randomization, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse reactions, and statistical analysis. High quality is expressed by scores of 4–8, whereas low quality is shown by scores of 0–3 [25]. Any unresolved differences between reviewers were resolved by consensus or by consultation with a third investigator. Publication bias was not assessable in these trials. Tests for funnel plot asymmetry are generally implemented only when at least ten studies are included in the meta-analysis [14]. As our analysis included only five studies, tests for asymmetry were not implemented as they would be unable to differentiate chance from asymmetry.
Data synthesis and analysis
The main outcomes of the meta-analysis included clinical and radiographic comparisons between the two surgical approaches for primary TKA. We analysed continuous outcomes, including surgical time, incision length, flexion ROM, KSS, CMA, and CFCA, using the weighted mean difference (WMD) to combine trials that measured the same outcome and used the same scale. Statistical heterogeneity among included studies was determined by estimating the proportion of between-study inconsistencies due to actual differences between studies, rather than differences due to random error or chance, using the Q statistics and I 2 test. A P > 0.05 and/or I 2 < 50 % indicated that there was no significant heterogeneity, so a fixed effect model was used to calculate the pooled effect size. Otherwise, the random effect model was adopted. All statistical analyses were performed with RevMan version 5.2 static software.
Results
Study identification and study characteristics
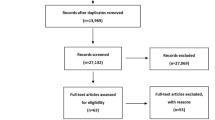
The details of study identification, inclusion, and exclusion are summarized (Fig. 1). An electronic search yielded 453 studies in PubMed (MEDLINE), 339 studies in EMBASE, 4 studies in the Cochrane Library, and 353 studies in KoreaMed. Five additional publications were identified through manual searching. This eventually amounted to five studies included in the meta-analysis [8, 22, 27, 28, 31]. Not all randomized studies are of Level I evidence.
Study characteristics and patient populations
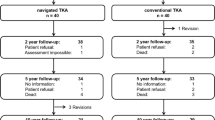
All five studies (four RCTs and one qRCT) compared clinical and radiographic outcomes in patients treated with the MINA or CONv approaches for primary TKA (Table 1).
Methodological quality assessment of the included studies
Randomization, allocation concealment, and blinding of the patients and surgeon were performed in three studies (60 %) included in this meta-analysis, while four RCTs (80 %) reported blinding of the outcome assessor. Table 2 summarizes the risk of bias and quality for the five studies included in the meta-analysis.
Clinical outcomes
Of the five studies, two reported surgical time. In these studies, 79 subjects were operated on with the MINA approach and 83 with the CONv approach. The pooled data showed that the surgical time was 10.29 min longer with the MINA approach than the CONv approach, but this difference was not statistically significant (95 % CI −18.51 to 39.09; n.s.; I 2 = 0 %, Fig. 2). Of the five studies, two reported incision length. In these studies, 79 subjects were operated on with the MINA approach and 83 with the CONv approach. The pooled mean difference in intraoperative incision length was −4.43 (95 % CI −5.18 to −3.69; P < 0.001; I 2 = 0 %, Fig. 3), indicating that the intraoperative incision length was significantly shorter with the MINA approach than the CONv approach. Of the five studies, three reported flexion ROM. In these studies, 138 subjects were operated on with the MINA approach and 143 with the CONv approach. The pooled mean difference in post-operative flexion ROM was 16.64 (95 % CI 14.26–19.01; P < 0.001; I 2 = 0 %, Fig. 4), indicating that post-operative flexion ROM was significantly greater with the MINA approach than the CONv approach. In terms of post-operative KSS, two studies compared 72 subjects who underwent the MINA approach and 70 subjects who underwent the CONv approach. The pooled data showed that the mean difference in the post-operative KSS was 11.15 point higher with the MINA approach than the CONv approach, but this difference was not statistically significant (95 % CI −8.55 to 30.84; n.s.; I 2 = 98 %, Fig. 5).
Results of aggregate analysis for comparison of incision length according to different surgical approaches. Abbreviations: MINA, minimally invasive navigation-assisted; CONv, conventional; Chi2, chi-square test; CI, confidence interval; IV, inverse variance; SD, standard deviation; I2, i-square test
Results of aggregate analysis for comparison of postoperative flexion range of motion (ROM) according to different surgical approaches. Abbreviations: MINA, minimally invasive navigation-assisted; CONv, conventional; Chi2, chi-square test; CI, confidence interval; IV, inverse variance; SD, standard deviation; I2, i-square test
Results of aggregate analysis for comparison of postoperative knee surgery score (KSS) according to different surgical approaches. Abbreviations: MINA, minimally invasive navigation-assisted; CONv, conventional; Chi2, chi-square test; CI, confidence interval; IV, inverse variance; SD, standard deviation; I2, i-square test
Radiographic outcomes
All five studies reported the CMA. A total of 220 subjects were operated on with the MINA approach and 229 subjects with the CONv approach. The pooled mean difference in the post-operative CMA was similar between the two approaches (95 % CI 1.01–0.54; n.s.; I 2 = 64 %, Fig. 6). In terms of post-operative CFCA, three studies compared 126 subjects who were treated with the MINA approach and 133 subjects who were treated with the CONv approach. The pooled mean difference in the post-operative CFCA was similar between the MINA and CONv approaches (95 % CI −0.91 to 2.97; n.s.; I 2 = 95 %, Fig. 7).
Results of aggregate analysis for comparison of postoperative coronal mechanical axis (CMA) according to different surgical approaches. Abbreviations: MINA, minimally invasive navigation-assisted; CONv, conventional; Chi2, chi-square test; CI, confidence interval; IV, inverse variance; SD, standard deviation; I2, i-square test
Results of aggregate analysis for comparison of postoperative coronal femoral component angle (CFCA) according to different surgical approaches. Abbreviations: MINA, minimally invasive navigation-assisted; CONv, conventional; Chi2, chi-square test; CI, confidence interval; IV, inverse variance; SD, standard deviation; I2, i-square test
Discussion
The principal findings from this meta-analysis were that there were no significant differences in clinical and radiographic outcomes, including surgical time, KSS, CMA, and CFCA, in patients who underwent MINA and CONv approach for primary TKA, but the MINA approach resulted in a slightly shorter incision length and increased flexion ROM than the CONv approach.
Obtaining restoration of the leg axis and correct component alignment in minimally invasive techniques for primary TKA is quite important to enable satisfactory long-term clinical outcomes [5]. The current meta-analysis showed that the MINA approach may not be associated with a higher rate of component malalignment due to poor restoration of the leg axis. As expected, these better radiographic results may be due in part to combining navigation-assisted techniques, which are associated with fewer technical errors in alignment, with minimally invasive techniques, even with limited visualization of critical anatomic landmarks.
Although navigation-assisted systems can successfully reduce the number of alignment outliers, navigation requires a longer surgical time and has a learning curve [13, 18, 23, 30]. It was found that the two approaches did not differ significantly in surgical time, regardless of the navigation system used or length of follow-up; however, there was a trend for the MINA approach to have a longer surgical time than the CONv approach. The surgical time may have been similar between the two approaches because all surgeons in the included studies were highly experienced and had used both the MINA and CONv approaches extensively, so they were likely beyond their learning curves. Other factors may be due to less hesitation of most surgeons with real-time monitoring during the intraoperative use of a navigation-assisted system as well as CONv approach including longer incision length may require an increased incidence of suture time.
This meta-analysis also showed a significantly shorter incision length with the MINA approach than the CONv approach (12.4 cm in MINA vs. 17.55 cm in CONv), suggesting that the smaller incision and limited knee arthrotomy of minimally invasive approaches can contribute to less post-operative pain and faster restoration of the extensor mechanism. This could explain the earlier gains in flexion ROM during the early post-operative period reported in previous studies [15], although greater tension on the incision margins caused by limited visualization may increase the risk of wound-healing problems [19]. However, none of the studies included in this meta-analysis reported any wound-healing problems with the MINA approach. Rather, this complication, including incisional skin slough that did not require surgical treatment, happened with the CONv approach.
There have been recent studies showing improved flexion ROM in the early post-operative period, which disappeared as early as 1 week to 3 months after surgery [2, 19]. Contrary to our expectations, patients with MINA approach in current meta-analysis appear to maintain improved flexion ROM even at 1 year after surgery. There are two possible explanations for that: first, quadriceps muscle strength in MINA approach could be persistently higher than that in CONv approach. These results may be due to differences in the preservation of the extensor mechanism between the two approaches. This possibility is supported by the results of one study in that CONv approach could reduce up to one-third in quadriceps strength calculated isokinetically through 2 years of follow-up [29]; second, MINA approach with the drilling of multiple bicortical pins was not sufficiently intense to cause the risk of haematoma over the thigh and post-operative stiffness related to pain, resulting in better ROM early and even at 1 year after surgery [12, 31].
This study had several limitations. Firstly, although the number of included in current meta-analysis was relatively small, we performed comprehensive and sensitive searches through electronic databases to minimize possibilities of publication bias. Additionally, all the five studies were in our inclusion of only Level I and II trials and four studies were graded with high quality scores. This means that methodological heterogeneity defined as differences between-study conducts including study design, study quality, and analysis is very low. Only, when there appeared to be clinical heterogeneity such as post-operative KSS, CMA, and CFCA in current meta-analysis, we used a random effects model to control for this heterogeneity. Also, the differences in outcome variables may be due to subjective differences caused by observer’s outcome measures. Therefore, it was recognized that the meta-analysis can be implemented. Secondly, long-term results which may affect an implant survival and long-term complications were not evaluated comparing the two approaches. However, it is widely appreciated that a follow-up of 3 months or greater was covered the crucial time when the benefits of the minimally invasive approach [9]. Thirdly, the heterogeneity of the included studies could also be explained by slight differences in other factors affecting surgical outcomes, such as the use of a wide variety of implants and navigation systems, and variability in the use of minimally invasive techniques with the lack of pain management standardization. Finally, adequate information could not be obtained on the clinical and radiographic outcomes of the included studies with the exception of CMA, which may affect the possible sources of heterogeneity owing to the limited data reported in original paper and large errors in the calculated standard deviation from missing standard deviation even though we should look carefully for statistics that allow calculation or estimation of the standard deviation. Therefore, more high quality and well-designed RCTs are needed in the near future.
Conclusions
There were no significant differences in clinical and radiographic outcomes, including surgical time, KSS, CMA, and CFCA, in patients who underwent MINA and CONv approach for primary TKA, but the MINA approach resulted in a slightly shorter incision length and increased flexion ROM than the CONv approach. Therefore, if particular attention has to be paid to patient’s selection with appropriate counselling and surgeon’s experience, MINA approach can provide early clinical benefit when compared with CONv approach.
References
Alan RK, Tria AJ Jr (2006) Quadriceps-sparing total knee arthroplasty using the posterior stabilized TKA design. J Knee Surg 19:71–76
Alcelik I, Sukeik M, Pollock R et al (2012) Comparison of the minimally invasive and standard medial parapatellar approaches for primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:2502–2512
Buechel FF Sr (2002) Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res 404:40–50
Chen AF, Alan RK, Redziniak DE et al (2006) Quadriceps sparing total knee replacement: the initial experience with results at two to four years. J Bone Joint Surg Br 88:1448–1453
Chin PL, Yang KY, Yeo SJ, Lo NN (2007) Randomized controlled trial comparing the radiologic outcomes of conventional and minimally invasive techniques for total knee arthroplasty. J Arthroplasty 22:800–806
Confalonieri N, Manzotti A, Pullen C, Ragone V (2007) Mini-incision versus mini-incision and computer-assisted surgery in total knee replacement: a radiological prospective randomised study. Knee 14:443–447
Dalury DF, Dennis DA (2005) Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res 440:77–81
Dutton AQ, Yeo SJ, Yang KY, Lo NN, Chia KU, Chong HC (2008) Computer-assisted minimally invasive total knee arthroplasty compared with standard total knee arthroplasty. J Bone Joint Surg Am 90:2–9
Gandhi R, Smith H, Lefaivre KA, Davey JR, Mahomed NN (2011) Complications after minimally invasive total knee arthroplasty as compared with traditional incision techniques: a meta-analysis. J Arthroplasty 26:29–35
Haas SB, Manitta MA, Burdick P (2006) Minimally invasive total knee arthroplasty: the mini midvastus approach. Clin Orthop Relat Res 452:112–116
Hart R, Janecek M, Cizmar I, Stipcak V, Kucera B, Filan P (2006) Minimally invasive and navigated implantation for total knee arthroplasty: X-ray analysis and early clinical results. Orthopade 35:552–557
Harvey IA, Barry K, Johnson R, Elloy MA (1993) Factors that affect the range of movements of total knee arthroplasty. J Bone Joint Surg 75B:950–955
Hernández-Vaquero D, Suárez-Vázquez A (2007) Complications of fixed infrared emitters in computer-assisted total knee arthroplasties. BMC Musculoskelet Disord 8:71
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration available from http://www.cochrane-handbook.org
Huang HT, Su JY, Chang JK, Chen CH, Wang GJ (2007) The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: report of a 2-year follow-up. J Arthroplasty 22:1007–1012
Keating EM, Meding JB, Faris PM et al (2002) Long-term followup of nonmodular total knee replacements. Clin Orthop Relat Res 404:34–39
Kim YH, Kim JS, Kim DY (2007) Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Joint Surg Br 89:467–470
Kim YH, Kim JS, Choi Y, Kwon OR (2009) Computer-assisted surgical navigation does not improve the alignment and orientation of the components in total knee arthroplasty. J Bone Joint Surg Am 91:14–19
Kolisek FR, Bonutti PM, Hozack WJ, Purtill J, Sharkey PF, Zelicof SB, Ragland PS, Kester M, Mont MA, Rothman RH (2007) Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty 22:8–13
Lee DH, Choi J, Hha KW, Kim HJ, Han SB (2011) No difference in early functional outcomes for mini-midvastus and limited medial parapatellar approaches in navigation-assisted total knee arthroplasty: a prospective randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 19:66–73
Li C, Zeng Y, Shen B, Kang P, Yang J, Zhou Z, Pei F (2015) A meta-analysis of minimally invasive and conventional medial parapatella approaches for primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1971–1985
Lüring C, Beckmann J, Haibock P, Perlick L, Grifka J, Tingart M (2008) Minimal invasive and computer assisted total knee replacement compared with the conventional technique: a prospective, randomised trial. Knee Surg Sports Traumatol Arthrosc 16:928–934
Macule-Beneyto F, Hernández-Vaquero D, Segur-Vilata JM, Colomina-Rodriguez R, Hinarejos-Gomez P, Carcia-Forcada I, Seral-Garcia B (2006) Navigation in total knee arthroplasty. A multicenter study. Int Orthop 30:536–540
Nestor BJ, Toulson CE, Backus SI (2010) Mini-midvastus vs standard medial parapatellar approach: a prospective, randomized, double-blinded study in patients undergoing bilateral total knee arthroplasty. J Arthroplasty 25(5–11):e1
Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord 12:232–236
Pagnano MW, Meneghini RM, Trousdale RT (2006) Anatomy of the Extensor Mechanism in Reference to Quadriceps-sparing TKA. Clin Orthop Relat Res 452:102–105
Seon JK, Song EK (2005) Functional impact of navigation-assisted minimally invasive total knee arthroplasty. Orthopedics 28:1251
Seon JK, Song EK (2006) Navigation-assisted less invasive total knee arthroplasty compared with conventional total knee arthroplasty: a randomized prospective trial. J Arthroplasty 21:777–782
Silva M, Shepherd EF, Jackson WO, Pratt JA, McClung CD, Schmalzried TP (2003) Knee strength after total knee arthroplasty. J Arthroplasty 18:605–611
Weber P, Crispin A, Schmidutz F, Utzschneider S, Pietschmann MF, Jansson V, Müller PE (2013) Improved accuracy in computer-assisted unicondylar knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21:2453–2461
Zhang Z, Gu B, Zhu W, Zhu L, Li Q, Du Y (2014) Minimally invasive and computer-assisted total knee arthroplasty versus conventional technique: a prospective, randomized study. Eur J Orthop Surg Traumatol 24:1475–1479
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, YS., Kim, HJ., Ko, YR. et al. Minimally invasive navigation-assisted versus conventional total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 24, 3425–3432 (2016). https://doi.org/10.1007/s00167-016-4016-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4016-2