Abstract
Introduction
To determine whether the placement of an interscalene brachial plexus block (IBPB) with general anaesthesia before shoulder arthroscopy would be effective in establishing a clear visual field and in shortening the surgical procedure.
Method
This prospective randomized control trial study included 152 patients who had undergone arthroscopic rotator cuff repair. Group A received IBPB and group B did not receive IBPB. A visual clarity scale (VCS) was determined by arthroscopic visualization. The systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), duration of surgical procedure, VCS, and medication that was administered for haemodynamic stability were recorded. Results: The VCS was improved in group A at stages 2 and 3 of the surgical procedures (p < 0.05), but there were no significant difference at stages 1 (p = 0.288) and 4 (p = 0.062). SBP, DBP, and HR were higher in group B during surgery (p < 0.05). The administered analgesics were higher in group B (p = 0.003), but there were no differences in hypotensive agents (p = 0.287). No significant difference was observed for the duration of surgery (p = 0.704).
Conclusions
Pre-operative IBPB with general anaesthesia for arthroscopic rotator cuff repair was beneficial in maintaining haemodynamic stability and improving the VCS during surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A clear view of the operative field ensures successful shoulder arthroscopy [1]. Subacromial space arthroscopy is characterized by (1) the inability to use a tourniquet and (2) absence of a synovial lining to prevent fluid extravasation [2]. Epinephrine-mixed saline irrigation, infusion flow or pressure control systems, and hypotensive anaesthesia can achieve a bloodless operative field. Maintaining a pressure difference of < 49 mmHg between the patient’s systolic blood pressure (SBP) and the intra-articular pressure achieves a clear operative field [2]. Therefore, maintaining low BP and minimizing intra-operative haemodynamic changes are important for shoulder arthroscopy.
Painful stimuli cause sympathetic nervous system activation [3]. The degree of pain correlates with the increase in BP and vascular resistance [4]. Pre-emptive analgesia inhibits sympathetic nerve activity during arthroscopy and when maintained intra-operatively, reduces the physiological consequences of surgery-induced nociceptive transmission [5]. Sufficient quantities of analgesics administered before performing the skin incision desensitize the nervous system [6].
The shoulder is innervated by nerves from the cervical and the brachial plexuses via the C5–T1 nerve roots. Thus, a lower cervical plexus block via an interscalene approach is suitable for shoulder arthroscopy [7]. Interscalene brachial plexus block (IBPB) anaesthesia is popular in patients undergoing shoulder surgery [8] because it maintains haemodynamic stability by preventing excessive BP elevation and provides a clear operative field by achieving a balance between the intra-articular and the SBP.
We compared the efficacy of general anaesthesia alone and general anaesthesia concomitant with IBPB for arthroscopic surgery. We hypothesize that general anaesthesia concomitant with IBPB is more effective than general anaesthesia alone to reduce operative time and establish a clearer operative field.
Materials and methods
Patient selection
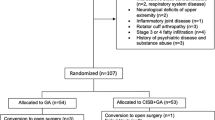
This prospective study recruited 152 patients who underwent arthroscopic rotator cuff repair between April 2012 and March 2014. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and/or National Research Committee and complied with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was performed following approval from our Institutional Review Board.
Inclusion criteria were patients who underwent rotator cuff repair for medium-sized tears. Tear sizes were evaluated using pre-operative shoulder magnetic resonance imaging and categorized into small (< 1 cm), medium (1–3 cm), large (3–5 cm), and massive (> 5 cm) based on the DeOrio and Cofield classification [9].
Exclusion criteria were patients who did not provide informed consent, those with hypertension, coagulopathy, a history of IBPB failure or cardiovascular disease, those using drugs that could affect their blood coagulation profile, and those with biceps pathology and “superior labral tear from anterior to posterior” lesions (conditions that could require additional procedures including biceps tenotomy, tenodesis, or labral stabilization) (Table 1). IBPB failure was defined as an immediate post-operative visual analogue scale (VAS) pain score > 4.
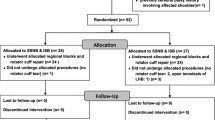
Patients were randomized into two groups: group A (n = 73) that received pre-operative IBPB before general anaesthesia and group B (n = 79) without pre-operative IBPB before general anaesthesia.
Interscalene brachial plexus block technique
Group A patients received the IBPB in the anaesthesia induction room. The IBPB was performed by a single expert anaesthesiologist. The patient was placed in the supine position with head rotated to the contralateral side, and the IBPB was performed using ultrasound guidance and nerve stimulation. The brachial plexus was identified using a nerve stimulator (Stimuplex-S, B. Braun Melsungen AG, Melsungen, Germany) connected to the proximal end of the inner metal needle of a plastic cannula (Stimuplex-A, 25G, B. Braun Melsungen). The initial current output of the nerve stimulator was 0.7 mA. A linear high frequency 6–13 MHz ultrasound probe (Sonosite M-turbo, SonoSite, Inc., Bothell, WA, USA) was used. Following contraction of the triceps muscle, the C5–6 nerve root or the superior trunk was identified, and 10 mL of 0.25% ropivacaine with 200 mcg of epinephrine was injected. Patients were transferred to the operating room for induction of general anaesthesia and surgery.
General anesthesia technique
Manual ventilation with O2 (6 L/min) via a facial mask was performed in all patients prior to the intravenous (IV) administration of the general anaesthetic. General anaesthesia was induced by the IV administration of thiopental (5 mg/kg) and rocuronium (1 mg/kg) followed by orotracheal intubation. Anaesthesia was maintained using a 1.5 minimal alveolar concentration of sevoflurane with 1 L/min each of O2 and nitrous oxide without any additional analgesics including opioids. Anaesthesia was maintained to achieve intra-operative bispectral index values of 40–60 throughout the procedure. Upon completion of the operation, reversal agents (IV glycopyrrolate and neostigmine) were administered prior to extubation [10].
Surgical technique
All operations were performed by a single shoulder arthroscopy specialist and one assistant who was blinded to the circumstances in which patients had received IBPB. Patients were placed in the lateral decubitus position with exposure of the affected shoulder. Epinephrine-mixed saline (1 mL of 1:1000 epinephrine/3000 mL of saline bag) was used for intra-articular irrigation. The irrigation fluid was infused via a pressure-controlled pump (Linvatec, Largo, FL, USA) set to a pressure of 50 mmHg. Arthroscopic examination of the glenohumeral joint was performed to identify any pathological lesions. After the glenohumeral joint procedure, we performed arthroscopic examination of the subacromial space. Subacromial decompression and acromioplasty were performed in all patients. The tear size, tendon quality, and delamination of the rotator cuff were assessed. Adhesiolysis was performed to release the retracted tendon for tendon mobilization, and the footprint of the greater tuberosity was decorticated. Two medial row anchors (4.5-mm Bio-Corkscrew suture anchor, Arthrex, Naples, FL, USA) were inserted at the medial edge of the footprint. A Scorpion suture passer (Arthrex, Naples, FL, USA) or a suture hook (Linvatec, Large, FL, USA) was used to pass thefibre wire through the tendon, close to the musculotendinous junction of the supraspinatus.
For standardization in surgical strategy, we only included reconstructions using the double-row technique. We concluded that the double-row technique is more reliable in terms of initial strength, stiffness, and strain over the footprint than a single-row technique and provides better repair [11]. Medial row knots were tied, and the retracted tendon was reduced into the footprint of the greater tuberosity. Lateral row anchors (3.5 mm and 4.5 mm, SwiveLock, Arthrex, Naples, FL, USA) were inserted 5–10 mm below the greater tuberosity after preparing the bone sockets [12].
Data collection
BP was measured on the contralateral extremity using an automatic BP cuff. The heart rate (HR) and an electrocardiogram were recorded. The SBP, diastolic blood pressure (DBP), and the HR were recorded every five minutes intra-operatively. The anaesthesiologist controlled BP using a combination of analgesics and hypotensive agents (2 μg/kg of fentanyl and 10 mg of esmolol, respectively). Medications were administered intra-operatively if the SBP was > 120 mmHg to control excessive bleeding. The frequency of administered medication was defined as the number of times the medication was administered.
The surgical procedure was performed in four stages: (1) the intra-articular soft tissue procedure, (2) acromioplasty, (3) greater tuberosity plasty with tendon preparation, and (4) tendon repair using a suture bridge. The duration of each stage and the amount of medication administered for haemodynamic stability were recorded.
During arthroscopy, the surgeon and the first assistant recorded the visual clarity scale (VCS). The VCS score was documented as the mean value of each operative stage and was evaluated by the operator and the first assistant at the end of each stage. The VCS score ranged from 1 (extremely poor conditions) to 5 (optimal conditions) (Table 2, Fig. 1). Each time the surgeon rated the VCS, the first assistant recorded the VCS score using the 5-point scale used by the surgeon.
Statistical analysis
Other than the number of patients, the sex ratio (%), the injured side, and the frequency of use of additional analgesics, all measured values were expressed as means, ranges, and standard deviations. All statistical analysis was performed using the SPSS software version 17.0 for Windows (SPSS, Inc., Chicago, IL). A chi-squared test or the Fisher exact test was performed for the sex ratio and the frequency of analgesic use. Changes in parameters (SBP, DBP, and HR) over time were assessed using a mixed effects linear regression model (linear mixed model) to evaluate within- and between-group differences. A p value < 0.05 was considered statistically significant.
Results
No statistically significant intergroup difference was observed in demographic factors (Table 3) and in the overall operative time or the time required for each operative stage (p = 0.704, Fig. 2).
The procedure of arthroscopic surgery was divided into total of four stages, and each of durations of surgery was evaluated against groups A and B. Stage 1, intra-articular soft tissue procedure; stage 2, acromioplasty; stage 3, greater tuberosity plasty and tendon preparation; stage 4, tendon repair with suture bridge. Total, total surgical procedure. †p = 0.704
BP and HR increased from the start of the surgical procedure and peaked five to ten minutes after the start of surgery, which corresponds to the beginning of the acromioplasty in both groups. Throughout the surgery, the mean SBP was significantly lower in group A. However, the mean DBP and HR were higher in group A (p < 0.05, Fig. 3).
Changes of systolic blood pressure (a), diastolic blood pressure (b), and heart rate (c) throughout the surgical procedures. Surgical procedure was divided into four stages and each change is recorded accordingly. (1) Intra-articular soft tissue procedure, (2) acromioplasty, (3) tendon mobilization and greater tuberosity plasty, and (4) tendon repair with suture bridge technique. The SBP, DBP, and HR sharply increased and peaked at 5~10 minutes after the start of surgery, which is the initial period of acromioplasty procedure. After the haemodynamic peak, the blood pressure and the heart rate were decreased gradually and plateaued during the remained surgical procedure.
The frequency of administration of intra-operative analgesics was 0.19 ± 0.46 vs. 0.53 ± 0.86 and that of hypotensive agents was 0.67 ± 0.94 vs. 0.85 ± 1.06 in groups A and B, respectively. The frequency of administered analgesics was significantly higher in group B than in group A (p = 0.003, Fig. 4). However, no statistically significant intergroup difference was observed in the hypotensive agents administered to maintain haemodynamic stability (p = 0.287, Fig. 4). The VCS was significantly improved in group A at stage 2 (p < 0.001) and stage 3 (p = 0.035) of the operative procedures. However, no significant difference was observed at stage 1 (p = 0.713) and stage 4 (p = 0.116). No IBPB- or procedure-related systemic adverse reactions were observed in either group.
Discussion
According to analysis of current trend of anesthetic method of shoulder surgery done by Ende et al., combination of general and regional anaesthesia is becoming predominant anaesthesia method of choice for shoulder arthroscopy [13]. The IBPB resulted in a significant decrease in both, the post-operative pain score and the need for supplemental analgesia in patients undergoing shoulder arthroscopy [14]. Several studies describing IBPB have focused on post-operative analgesia and the cost-effectiveness of alternative modalities of general anaesthesia for shoulder surgery. No study has compared the intra-operative effects of IBPB combined with general anaesthesia with those of general anaesthesia alone in patients undergoing shoulder arthroscopy. We additionally assessed the intra-operative effects of IBPB including the amount of bleeding, visualization quality, medications required for BP control, and operative time.
There is general consensus that IBPB effectively maintains haemodynamic stability during shoulder arthroscopy. Lee et al. reported that intra-operative haemodynamic stability was well maintained in patients who underwent IBPB before shoulder arthroscopy [15]. Our study revealed that patients who underwent pre-operative IBPB showed lower BP even without the frequent intra-operative administration of hypotensive medications. Marked bleeding obscures the operative field and necessitates lowering BP. However, increased usage of hypotensive agents may cause significant adverse effects, particularly in patients with cardiovascular disease. Haemodynamic instability can compromise cerebral perfusion with clinically significant cerebral ischaemia and consequent stroke, visual or neurological sequelae, or even death [16]. IBPB effectively reduces the intra-operative usage of hypotensive agents and the accompanying adverse effects.
Jesen et al. evaluated arthroscopic visualization using a surgeon-rated VAS (1–10) and the haemoglobin concentration of the irrigation fluid [1]. Harris et al. used a 3-score rating system (1, unimpaired visualization; 2, some impairment during specific parts of the procedure; and 3, significantly impaired visualization) [17]. In our study, a 5-point VCS was used to evaluate arthroscopic visualization, as scored by the surgeon based on surgical working conditions. We modified the VCS proposed by Harris et al. with a detailed description provided for reproduction (Table 2). As anticipated, the arthroscopic operative view evaluated using the VCS was clearer in patients undergoing pre-operative IBPB. It is verified that pre-operative IBPB with general anesthesia for arthroscopic rotator cuff repair effectively reduces haemodynamic instability and improves intra-operative VCS. A clear bloodless operative field facilitates smooth surgery without necessitating measures to control bleeding and reduces the operative time. Use of epinephrine-mixed saline in shoulder arthroscopy also improves VCS as well [18]. Combination of general and regional anaesthesia can be applied in elderly patients with irreparable rotator cuff tears, who are at potential risk by long period of anaesthesia, for simple arthroscopic debridement or biceps tenotomy for symptomatic alleviation [19].
Contrary to our expectation, statistical analyses did not show a significant reduction in the operative time in group A, which could be attributed to (1) We attempted standardization of the intergroup operative time by selecting only medium-sized rotator cuff tears in all patients. Most medium-sized rotator cuff tears can be repaired arthroscopically within an hour; thus, no significant intergroup difference was observed. (2) Owing to the nature of our study (blinded trial), the surgeon may have requested for BP control more frequently to improve the VCS. The frequency of analgesic administration was higher in group B. Owing to its in vivo state, medications were administered to maintain stable BP to minimize patient risk. Stable BP reduces intra-operative bleeding and shortens the overall operative time. The administration of medications controlled BP and pain identically in both groups; thus, it is reasonable to expect a shorter operative time in group A patients who underwent IBPB.
In our study, analgesics were more frequently administered in group B than in group A. Under general anaesthesia, patients are unconscious but continue to receive nociceptive stimuli, particularly during painful procedures including acromioplasty and greater tuberosity-plasty. Spinal reflexes activate the sympathetic nervous system based on the duration and the magnitude of the stimulus, causing increased peripheral resistance and stroke volume, which impair VCS. It is known that patients under general anaesthesia are more susceptible to painful stimuli and more likely to show higher SBP than those receiving a combination of general and regional anaesthesia [3, 20].
The operative time was divided into four stages based on operative procedures. Analysis of patients’ haemodynamic status showed distinctive elevations in both BP and HR with peaks observed during the acromioplasty. Based on this observation, improving the operative view should include technical measures to avoid conditions that precipitate haemodynamic alterations during acromioplasty or using preventive medications including fentanyl and esmolol to avoid BP elevations.
Clear VCS could be accomplished with the use of IBPB in stages 2 (acromioplasty) and 3 (greater tuberosity plasty with tendon preparation). Acromioplasty and greater tuberosity plasty involve the use of an arthroscopic burr to remove cortical bone and expose cancellous bone, which is more painful than other arthroscopic manipulation and consequently elevates SBP. Bone bleeding, which impairs VCS, cannot be controlled by managing coagulation but requires elevation of intra-articular pressure by increasing inflow of normal saline. However, increased normal saline flow can cause extravasation and consequent soft tissue swelling that interferes with arthroscopy. Preoperative IBPB can reduce elevation of SBP and effectively control intra-articular bone bleeding after acromioplasty and greater tuberosity plasty [21].
Confirming whether the haemodynamic peak is relevant to acromioplasty or is merely a common phenomenon that occurs approximately fiie to ten minutes after the start of surgery is important.
Limitations of this study
-
1.
Our study only included patients with simple medium-sized tears. A medium-sized rotator cuff tear is defined as a full-thickness tear showing 1–3-cm retraction. Tendon quality is classified based on the Goutallier classification [22]. Notably, the degree of fatty infiltration in the rotator cuff affects post-operative results and the re-tear rate and does not affect the operative time itself. Additionally, we only used the double-row suture technique with 2 × 2 medial row suture anchors to standardize the operative time; thus, the correlation between fatty infiltration and operative time would be “irrelevant” in this study. The size of a tear affects operative times and could significantly affect the conclusions of this study. Small-sized tears were excluded from the study because of the relative simplicity of the surgery, a shorter operative time, and negligible effects on the intergroup comparison of operative times. Large-sized and massive tears were also excluded owing to variations in surgical procedures employed based on tear shape, tendon involvement, and reparability, which cannot be generalized to estimate and compare outcomes. Thus, only patients who underwent medium-sized rotator cuff repair were selected as the optimal study population to ensure a standardized operative procedure and appropriate operative time that could be evaluated to assess the effect of IBPB on the surgery. However, since tendon with degeneration requires a certain amount of debridement prior to arthroscopic repair, the subtle discrepancy between pre-operative tear characteristics on MRI and intra-operative debrided tendon characteristics is expected [23].
-
2.
We excluded patients with hypertension, cardiovascular disease, and coagulation abnormalities, who show a greater risk of bleeding during arthroscopy. In our view, these limitations could lead to an underestimation IBPB efficacy.
This study showed that a combination of general and regional anaesthesia requires lesser medication administration to maintain a favourable VCS for arthroscopic procedures. Furthermore, combination of anaesthesia stabilizes SBP and minimizes intra-operative blood loss, which is useful in operations performed in anatomical locations where a tourniquet cannot be applied including the proximal humerus or the femoral neck. Large-scale studies in patients with large-sized rotator cuff tears, hypertension, or cardiovascular disease are warranted.
References
Jensen KH, Werther K, Stryger V, Schultz K, Falkenberg B (2001) Arthroscopic shoulder surgery with epinephrine saline irrigation. Arthroscopy 17:578–581. https://doi.org/10.1053/jars.2001.23590
Morrison DS, Schaefer RK, Friedman RL (1995) The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy 11:557–560
Saccò M, Meschi M, Regolisti G, Detrenis S, Bianchi L, Bertorelli M, Pioli S, Magnano A, Spagnoli F, Giuri PG (2013) The relationship between blood pressure and pain. J Clin Hypertens 15:600–605
Maixner W, Gracely RH, Zuniga JR, Humphrey CB, Bloodworth GR (1990) Cardiovascular and sensory responses to forearm ischemia and dynamic hand exercise. Am J Phys 259:R1156–R1163
Dahl JB, Moiniche S (2004) Pre-emptive analgesia. Br Med Bull 71:13–27. https://doi.org/10.1093/bmb/ldh030
Dalury DF, Lieberman JR, Macdonald SJ (2012) Current and innovative pain management techniques in total knee arthroplasty. Instr Course Lect 61:383–388
Lanna M, Pastore A, Policastro C, Iacovazzo C (2012) Anesthesiological considerations in shoulder surgery. Transl Med UniSa 3:42–48
Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU (1993) Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy 9:295–300
DeOrio JK, Cofield RH (1984) Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 66:563–567
Park SK, Choi YS, Choi SW, Song SW (2015) A comparison of three methods for postoperative pain control in patients undergoing arthroscopic shoulder surgery. Korean J Pain 28:45–51. https://doi.org/10.3344/kjp.2015.28.1.45
Kim DH, ElAttrache NS, Tibone JE, Jun B-J, DeLaMora SN, Kvitne RS, Lee TQ (2006) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 34:407–414. https://doi.org/10.1177/0363546505281238
Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H (2014) Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elb Surg 23:1675–1681. https://doi.org/10.1016/j.jse.2014.02.021
Ende D, Gabriel RA, Vlassakov KV, Dutton RP, Urman RD (2016) Epidemiologic data and trends concerning the use of regional anaesthesia for shoulder arthroscopy in the United States of America. Int Orthop 40:2105–2113
Hughes MS, Matava MJ, Wright RW, Brophy RH, Smith MV (2013) Interscalene brachial plexus block for arthroscopic shoulder surgery: a systematic review. J Bone Joint Surg Am 95:1318–1324. https://doi.org/10.2106/jbjs.l.01116
Lee HY, Kim SH, So KY, Kim DJ (2012) Effects of interscalene brachial plexus block to intra-operative hemodynamics and postoperative pain for arthroscopic shoulder surgery. Korean J Anesthesiol 62:30–34. https://doi.org/10.4097/kjae.2012.62.1.30
Lee JH, Min KT, Chun YM, Kim EJ, Choi SH (2011) Effects of beach-chair position and induced hypotension on cerebral oxygen saturation in patients undergoing arthroscopic shoulder surgery. Arthroscopy 27:889–894. https://doi.org/10.1016/j.arthro.2011.02.027
Ogilvie-Harris DJ, Weisleder L (1995) Fluid pump systems for arthroscopy: a comparison of pressure control versus pressure and flow control. Arthroscopy 11:591–595
Kuo L-T, Chen C-L, Yu P-A, Hsu W-H, Chi C-C, Yoo J-C (2018) Epinephrine in irrigation fluid for visual clarity in arthroscopic shoulder surgery: a systematic review and meta-analysis. Int Orthop:1–9
Pander P, Sierevelt IN, Pecasse GA, van Noort A (2018) Irreparable rotator cuff tears: long-term follow-up, five to ten years, of arthroscopic debridement and tenotomy of the long head of the biceps. Int Orthop:1–6
Kaufman E, Epstein JB, Gorsky M, Jackson DL, Kadari A (2005) Preemptive analgesia and local anesthesia as a supplement to general anesthesia: a review. Anesth Prog 52:29–38
Tetzlaff JE, Yoon HJ, Brems J (1994) Interscalene brachial plexus block for shoulder surgery. Reg Anesth 19:339–343
Melis B, Wall B, Walch G (2010) Natural history of infraspinatus fatty infiltration in rotator cuff tears. J Shoulder Elb Surg 19:757–763
Eren I, Ozben H, Gunerbuyuk C, Koyuncu Ö, Aygün MS, Hatipoglu E, Aydingöz Ü, Demirhan M (2018) Rotator cuff tear characteristics: how comparable are the pre-operative MRI findings with intra-operative measurements following debridement during arthroscopic repair? Int Orthop:1–7
Funding
This work was supported by a research grant from the Jeju National University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All the authors have taken a significant and crucial part in the preparation of the article and that they have read and approved the final version.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study submitted has been reviewed by IRB; after reviewing submitted IRB protocol and other related materials, the participated IRB members agreed upon the “Approval” of the research.
Rights and permissions
About this article
Cite this article
Choi, S., Kim, T., Kwon, Y.S. et al. Intra-operative effect of interscalene brachial plexus block to arthroscopic rotator cuff repair surgery. International Orthopaedics (SICOT) 43, 2117–2124 (2019). https://doi.org/10.1007/s00264-018-4199-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4199-x