Abstract
Purpose
To investigate if the stability of minimally invasive screw osteosynthesis of displaced intra-articular calcaneal fractures (DIACF) can be effectively increased by an innovative approach to screw tip augmentation.
Methods
In eight-paired human cadaver hindfoot specimens, DIACF of Sanders type IIB were treated with either standard screw osteosynthesis or with bone cement augmentation of the screw tips in the main fragments. The instrumented specimens were subjected to a cyclic loading protocol (9000 cycles, with stepwise increasing loads, 100–1000 N). The interfragment motions were quantified as tuber fragment tilt (TFT) and posterior facet inclination angle (PFIA) using a 3-D motion analysis system. Böhler’s angle (BA) was evaluated from X-rays. A load-to-failure test was performed after the cyclic loading protocol.
Results
All but one specimen of the augmented group withstood more cycles than the respective specimens of the non-augmented group. Mean cycles to failure for the failure criterion of 5° TFT were 7299 ± 1876 vs. 3864 ± 1810, corresponding to loads of 811 N ± 195 vs. 481 N ± 180, (P = 0.043). There were no significant differences observed in the PFIAs. The failure criterion of 5° BA was reached after a mean of 7929 cycles ± 2004 in the augmented group and 4129 cycles ± 2178 in the non-augmented group, corresponding to loads of 893 N ± 200 vs. 513 N ± 218, (P = 0,090). The mean load-to-failure of the four specimens in the augmented group that completed the cyclic loading was 1969 N over a 1742–2483 N range.
Conclusion
Screw tip augmentation significantly improved the mechanical stability of the calcanei after osteosynthesis in terms of decreased tuber fragment tilts and less changes in Böhler’s angle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneus fractures are life-changing events. Such events are reported to have a similar impact on the quality of life as myocardial infarction or organ transplantation [1,2,3]. The trauma is usually caused by high energy axial directed force, typically as a result of falls from a height or traffic accidents. Approximately three out of four calcaneus fractures fall into the category of displaced intra-articular fractures (DIACF) [4,5,6].
Minimally invasive screw osteosynthesis has become an increasingly attractive alternative to standard side plating through an extended lateral approach. It has been shown to yield excellent results when special care is taken to achieve anatomical reduction at the posterior facet articular surface [7,8,9,10]. This approach decreases soft tissue-related complications such as wound necrosis, delayed wound healing, and deep infection compared to lateral plating [7, 9, 11, 12]. This is especially important for co-morbid and elderly patients [11]. The increasing number of elderly patients with high activity levels poses special challenges to orthopaedic trauma surgeons [5, 13, 14]. The incidence of calcaneal fractures in the eldery has tripled within the last decades [13]. Increases in these numbers will also result in an increase in healthcare costs in years to come.
Minimally invasive screw osteosynthesis has been reported to result in similar fixation strength to lateral plating in Sanders IIB fracture models [14, 15]. However, concerns remain about the mechanical stability of fractures with depression defects, especially if the bone quality is compromised [7]. This may lead to delayed mobilization and impaired clinical outcomes [16, 17].
Therefore, it is important to investigate techniques that may improve the mechanical stability of minimally invasive screw osteosynthesis. With this in mind, the aim of this study was to investigate a novel technique for “minimally invasive” cement augmentation of the screw tips in the main fragments only, using a representative Sanders type IIB fracture model with relevant depression defects under cyclic loading conditions. We hypothesized that this technique could significantly increase the mechanical stability outcomes in terms of interfragment motion, Böhler’s angle (BA), and load to failure.
Materials and methods
Specimens
Eight fresh frozen human hind-foot pairs were harvested from eight body donors. The bodies were donated by people who had given written informed consent for their use for scientific and educational purposes prior to death [18]. Four pairs were from female donors. The mean age at death was 67.3 ± 9.5 years (range, 52–79 years). Bone mineral density (BMD) was assessed through quantitative computed tomography (qCT; LightSpeed VCT, GE Healthcare, Milwaukee, USA) using a calibration phantom. The mean BMD for the calcanei was 161.1 ± 26.8 mg/cm3. Specimens were stored at −20 °C and thawed over night at 4 °C before testing. Before dissection, two perpendicular Kirschner wires were inserted into the talus with the foot in physiological standing position (bare foot in horizontal position, tibia parallel to the frontal and sagittal planes). This ensured correct orientation of the talocalcaneal unit for later embedding and biomechanical testing. Skin and musculature were then removed, leaving the isolated talocalcaneal unit, with most of the subtalar joint capsule intact [19, 20]. Metallic markers were inserted in the bony landmarks to standardize BA measurements, i.e., the most superior portion of the tuber, the posterior facet articular surface and the anterior process (Fig. 1) [21]. For pairwise comparison, left and right talocalcaneal units were randomly allocated to either the augmented or non-augmented groups.
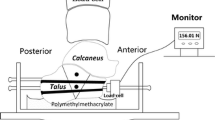
(a) Fracture Model. 1: First cut producing the tuber fragment (TF). 2: Second cut producing the anterior process fragment (APF). 3: Third cut producing the posterior facet fragment (PFF) and the sustentaculum fragment (SF). Hatched area: depression defect and blow-out fragment with a 10-mm base removed from the lateral wall. (b) Instrumented specimen with augmentation: Kirschner wires define the physiological orientation of the talocalcaneal unit. Metallic markers enabled standardized Böhler’s angle measurement (blue lines). Two 4.0 mm sustentaculum screws and two 6.5 mm screws for fixation of the main fragments with cement cloud around the screw tips
Fracture creation and surgical technique
Uniform Sanders IIB fractures with a depression defect were created by placing three cuts that created the main fragments with an oscillating saw, followed by removal of a blow-out fragment with a 10-mm base (Fig. 1A) [5].
All surgical procedures were performed by the same senior orthopaedic surgeon. For fixation of the posterior facet fragment (PFF) to the sustentaculum fragment (SF), two cannulated partially threaded 4.0 mm screws (Synthes, Oberdorf, Switzerland) were inserted from the lateral subchondral aspect of the posterior facet into the sustentaculum tali. For the fixation of the main fragments, two fully threaded 6.5 mm screws were inserted, either in an augmented or a non-augmented fashion, depending on which group the unit had been allocated to. One screw was inserted at the posterolateral calcaneal tuberosity, just posterior to the weight-bearing surface. This screw was oriented along the long axis of the calcaneus, with its tip located centrally in the subchondral zone of the anterior process. The other screw was inserted 15 mm medial to the entry point of the first screw. It was oriented at 90° to the posterior facet of the subtalar joint, with its tip located centrally in the subchondral zone of the posterior facet (Fig. 1B).
For screw augmentation, approximately 1 mL of PMMA bone cement (Mendec Spine, Tecres, Verona, Italy) was injected into the anterior process fragment (APF) and approximately 0.5 mL into the subchondral aspect of the PFF prior to insertion of the screws (Fig. 1B). The screws were tightened manually using the standard AO technique until a firm 3-finger grip was tangible [19, 20, 22]. This approach ensured that the screws were not over-tightened.
Biomechanical testing
Test setup
The specimens were embedded in an epoxy resin (RenCast, Huntsman Advanced Materials, Basel Switzerland). The talus was attached to the actuator of a servohydraulic material testing machine (MTS Mini- Bionix II 858; MTS, Eden Prairie, MN) via a ball and socket joint, which was used to axially push the talus on the subtalar joint. The tuber calcanei were mounted on a custom-made cylindrical jig and the anterior process was mounted via a cylindrical jig on an x-y bearing table. The custom-made jigs facilitated the maintenance of a constant distance between the center of axial force application on the talus and the tuber fragment (TF) and APF centres of rotation respectively (Fig. 2).
Test setup. Right-hand specimen mounted in the test setup in its physiological standing position via two custom made cylindrical jigs for the anterior process and the tuber calcanei. Red arrow: application of cyclic axial force through the talus via a ball and socket joint. Red and green arrows: degrees of freedom of the test setup (6). Three markers of the 3-D motion analysis system were attached to either the jig at the anterior process fragment (APF), at the tuber fragment (TF) or directly to the bone of the posterior facet fragment (PFF), measuring the relative motion of the fragments to each other—tuber fragment tilt (TFT): TF-APF and posterior facet inclination angle (PFIA): PFF-TF
An ultrasound-based 3-D motion analyzing system (Winbiomechanics, Zebris, Isny, Germany) was fixed to the three main fragments. Relative rotational fragment motion was recorded at a sampling rate of 60 Hz: the tuber fragment tilt (TFT) as relative motion of the TF to the APF [4] and the posterior facet inclination angle (PFIA) as relative motion of the PFF to the TF in the sagittal plane respectively (Figs. 1 and 2).
A C-Arm was positioned around the test-setup to capture lateral radiographs of the specimens and to measure BA. X-rays were taken before and after the ramp load and every 1000th cycle at a valley load of 50 N.
Failure criteria for loss of reduction were defined as changes of 5° in any of the aforementioned parameters, i.e., TFT, PFIA, or BA [10, 14].
Cyclic loading
A preload of 50 N was applied, followed by a ramp load to 100 N at 10 N/s. The cyclic loading protocol consisted of intervals of 100 cycles with stepwise increasing peak loads of 10 N per interval and a constant valley load of 50 N until a load of 1000 N was reached (total of 9000 cycles), or until construct failure occurred. The cyclic axial loading was applied through the talus at 0.5 Hz. The specimens that did not show structural fixation failure after the final load level of 1000 N underwent a subsequent load-to-failure test with an axial load applied at 50 mm/min.
Statistical analysis
Descriptive statistics were used to compare baseline characteristics between the groups. Data are presented as means with standard deviation (SD). Differences between the two groups were compared using a Wilcoxon-signed rank test. The significance level was set at P < 0.05. All P values are two-tailed.
Results
There were no significant differences in the BMD of both groups (163.1 ± 29.1 non augmented group vs. 159.2 ± 26.5 augmented group, P = .176). One pair of specimen had to be excluded from the analyses because of non-physiological failure due to separation of the anterior process fragment from the embedding fixation (n = 7 for the following analyses).
Large differences in stability between the specimens after augmentation of the screw tips and those with standard non-augmented screw fixation were evident. All specimens in the non-augmented group presented with complete structural failure during cyclic loading, whereas four subjects from the augmented group sustained all 9000 cycles of loading (1000 N) without structural failure, and were subjected to a subsequent load-to-failure test. In all cases of construct failure, excessive loss of reduction was due to a displacement of the TF in relation to the APF, where TFT was the most sensitive parameter (Figs. 3 and 5).
In the paired comparison, all but one specimen of the augmented group withstood more cycles than the respective specimens in the non-augmented group (P = 0.043)—the mean difference for the failure criterion of 5° TFT was 4492 cycles, range 1320–6302, corresponding to a load of 549.2 N, range 232.0–730.2 N (n = 6), with the difference of the one exceptional case being 2907 cycles, (Fig. 3).
Tuber fragment tilt
Only three specimens in the non-augmented group reached the benchmark of 5000 cycles (600 N load level) with a mean TFT of 1.45° ± 1.07 (n = 3). In the augmented group, six specimens reached this level with a mean TFT of 1.06° ± 0.90 (n = 6), five of which also withstood the 7000-cycle benchmark (800 N load level), with a mean TFT of 2.38° ± 2.16 (n = 5), whereas none of the non-augmented group reached this load-level (Fig. 4).
Posterior facet inclination angle
At construct failure due to excessive TFT, the mean PFIA was 2.50° ± 1.45 in the non-augmented group (max. 5000 cycles), compared to 1.83° ± 1.05 in the augmented group until the end of the cyclic loading after 9000 cycles (1000 N).
Böhler’s angle
In the non-augmented group, the failure criterion of 5° BA was reached after a mean of 4129 cycles ± 2178 (corresponding to a load of 512.9 N ± 217.8), compared to 7929 cycles ± 2004 (892.9 N ± 200.4) in the augmented group (P = 0.090). Four specimens in the augmented group did not reach 5° BA until the end of the cyclic loading, after 9000 cycles at a 1000 N load level, with a mean of 1.32° ± 0.82° (n = 4).
Load-to-failure
Only four specimens (n = 4) in the augmented group completed the cyclic loading and were subjected to a load-to-failure test. The mean load-to-failure was 1969 N with a range of 1742–2483 N.
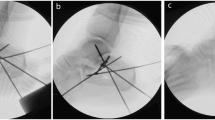
Failure mechanism
In all specimens, of both groups, failure occurred due to excessive TFT. In the non-augmented group, this typically occurred due to complete pull-out of the longitudinal screw from the APF, while in the augmented group, the characteristic failure mechanism was due to partial dislocation of the longitudinal screw together with its surrounding cement cloud.
After construct failure, the posterior facet articular surface was visually inspected after careful dissection of the talo-calcaneal unit. None of the specimens presented with an irregular articular surface of more than 0.5 mm (Fig. 5).
Typical failure mode (a) in a left non-augmented specimen after complete structural failure with pull-out of the longitudinal screw and (b) in a right-augmented specimen with partial dislocation of the screw together with its surrounding cement cloud. (c, d) After dissection for inspection of the posterior facet joint surface no relevant loss of reduction at the joint surface (blue arrows) was detected in the specimens of either group
Discussion
The results of our study confirm the hypothesis that augmentation of the screw tips in the main fragments improves mechanical stability after osteosynthesis procedures in the treatment of DIACF. This approach leads to less TFT and BA during cyclic loading, thus the specimen samples survived more cycles to failure and higher failure loads.
The mean cycles to failure increased by 4492 cycles (corresponding to a load of 549 N) in the augmented screw group, which is in accordance with a previous investigation. Rausch et al. [14] reported that screw fixation with augmentation resulted in similar cycles to failure outcomes for side plating. However, there are some differences to the study design. Their model comprised 5000 cycles, corresponding to a final load of 500 N, there was no lateral cortical defect and the cement for augmentation was injected through the lateral fracture line.
Although there is increasing literature evidence about successful cement augmentation in the treatment of fractures [16], apart from this investigation by Rausch et al. [14], the literature on the biomechanical effect of cement augmentation in fractures of the calcaneus is limited. It is, however, highly desirable to further improve the primary stability achieved by screw fixation of DIACF, as early functional aftercare plays a crucial role in clinical outcomes, especially in elderly patients [7, 16, 17, 23]. Moreover, patients often cannot accurately reproduce a partial weight bearing order and this inaccuracy is known to increase with advancing age [24]. To our knowledge, this is the first study to evaluate the biomechanical efficacy of screw tip augmentation in a Sanders IIB fracture model with a relevant depression defect.
We found changes in TFT to be the most sensitive parameter. Displacement of the TF through an axially directed force in combination with strain of the Achilles tendon has recently been described as a relevant clinical failure mode [4]. In our test set-up, changes in the TFT were detected early and increased continuously until failure, while BA barely changed until failure, after which a sudden increase in BA was observed.
Significant inaccuracies have been reported for BA measurements, with errors of up to 6° [21]. To avoid such measurement errors, metallic markers were used to reproducibly define landmarks for BA-measurement. Nevertheless, in Sanders II fractures, BA is a combination of the dislocation of three fragments and consequently, the late change in BA in our test setup may be partly explained by the fact that fragment fixation proved comparatively strong in the PFF. Thus, although a valued clinical parameter [25], as a single parameter it might not be specific enough for mechanical evaluations of fracture fixations in laboratory experiments [21].
Two screws inserted in the dense bone of the sustentaculum resulted in strong fixation, with no dislocation documented at the inspection of the joint surface after completion of the protocol and dissection of the specimen. This is in agreement with a former biomechanical study on the fixation of SFs [26].
The main failure mechanisms observed in our study with dislocation of the TF and the APF have been reported previously [4, 5, 14, 27]. However and notably, these studies either used fracture models with less severe comminution or compared different types of implants.
We specifically chose the Sanders IIB fracture model with depression defect in accordance with Illert et al. [5]. Since these fractures typically occur after an axially directed force, the depression of the PFF often results in defects at the lateral wall. The reduced cortical support leads to a high degree of instability, which is currently underrepresented in the literature on the mechanical stability of minimally invasive screw osteosynthesis.
While in other studies evaluating the effects of cement augmentation in side plating or in screw fixation versus side plating larger amounts of cement were inserted in the fracture lines [14, 28], we adopted a more “minimally invasive” approach of screw augmentation. To avoid potential drawbacks of cement application at the fracture lines, we augmented only the screw tips in the main fragments. This technique of augmentation has proven to be easily applicable, safe, and effective in other anatomical regions [16].
We consider the cyclic testing model we used to have been particularly well-suited to test our hypothesis. Three-point bending models have been further developed and proven to be successful in previous biomechanical studies on calcaneal fractures [5, 14, 15]. To simulate in vivo loading, the force was applied via a ball and socket joint through the native talus with an intact talocalcaneal unit in a physiological orientation. With sliding-hinge joints allowing fragment dislocation similar to that during injury and the 3-D motion analysis system mounted in the main fragments, the clinically relevant dislocation could be readily assessed.
Notwithstanding the above, it is important to recognize that the complexity of load transmission through the talocalcaneal unit and motion at the adjacent joints are difficult to reproduce and our model can only be an approximation of such. The cadaveric specimens freed of the surrounding soft tissue and fractures created by clean cuts provide less stability and result in higher forces at the screw bone interface and cannot entirely reproduce in vivo conditions. The proposed technique mainly aims to increase primary stability in the minimally invasive treatment of calcaneal fractures in an elderly population and the results should not be generalized to all patients with calcaneal fractures. Variations in the size, location, and number of screws might result in different failure patterns of a percutaneous screw osteosynthesis of the calcaneus. Therefore, the results of the present study should not be generalized for percutaneous screw instrumentations of the calcaneus. Randomized controlled trials will be necessary to evaluate if screw augmentation improves fracture reduction after minimally invasive screw osteosynthesis of DIACF in clinical practice. Until these results are available, our study suggests that screw augmentation may help to optimize early stability of minimally invasive screw osteosynthesis for DIACF treatment, allowing for earlier post-operative mobilization.
Conclusion
Augmentation of the screw tips in the main fragments resulted in increased mechanical stability under cyclic loading conditions regarding interfragment motion and Böhler’s angle and should be considered especially in patients with reduced bone quality.
References
Brunner A, Muller J, Regazzoni P, Babst R (2012) Open reduction and internal fixation of OTA type C2-C4 fractures of the calcaneus with a triple-plate technique. J Foot Ankle Surg 51(3):299–307. https://doi.org/10.1053/j.jfas.2012.01.011
van Tetering EA, Buckley RE (2004) Functional outcome (SF-36) of patients with displaced calcaneal fractures compared to SF-36 normative data. Foot Ankle Int 25(10):733–738
Alexandridis G, Gunning AC, Leenen LP (2015) Patient-reported health-related quality of life after a displaced intra-articular calcaneal fracture: a systematic review. World J Emerg Surg 10:62. https://doi.org/10.1186/s13017-015-0056-z
Ghorbanhoseini M, Ghaheri A, Walley KC, Kwon JY (2016) Superior tuber displacement in intra-articular calcaneus fractures. Foot Ankle Int 37(10):1076–1083. https://doi.org/10.1177/1071100716651965
Illert T, Rammelt S, Drewes T, Grass R, Zwipp H (2011) Stability of locking and non-locking plates in an osteoporotic calcaneal fracture model. Foot Ankle Int 32(3):307–313. https://doi.org/10.3113/FAI.2011.0307
Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures–open reduction and internal fixation (ORIF). Injury 35(Suppl 2):SB46–SB54. https://doi.org/10.1016/j.injury.2004.07.011
Rammelt S, Amlang M, Sands AK, Swords M (2016) New techniques in the operative treatment of calcaneal fractures. Unfallchirurg 119(3):225–236; quiz 236–228. https://doi.org/10.1007/s00113-016-0150-z
Schepers T (2016) Calcaneal fractures: looking beyond the meta-analyses. J Foot Ankle Surg 55(4):897–898. https://doi.org/10.1053/j.jfas.2016.05.009
Tantavisut S, Phisitkul P, Westerlind BO, Gao Y, Karam MD, Marsh JL (2017) Percutaneous reduction and screw fixation of displaced intra-articular fractures of the calcaneus. Foot Ankle Int 38(4):367–374. https://doi.org/10.1177/1071100716679160
Weber M, Lehmann O, Sagesser D, Krause F (2008) Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J Bone Joint Surg (Br) 90(12):1608–1616. https://doi.org/10.1302/0301-620X.90B12.20638
Carow JB, Carow J, Gueorguiev B, Klos K, Herren C, Pishnamaz M, Weber CD, Nebelung S, Kim BS, Knobe M (2018) Soft tissue micro-circulation in the healthy hindfoot: a cross-sectional study with focus on lateral surgical approaches to the calcaneus. Int Orthop. https://doi.org/10.1007/s00264-018-4031-7
Schepers T, Backes M, Dingemans SA, de Jong VM, Luitse JSK (2017) Similar anatomical reduction and lower complication rates with the sinus tarsi approach compared with the extended lateral approach in displaced intra-articular calcaneal fractures. J Orthop Trauma 31(6):293–298. https://doi.org/10.1097/BOT.0000000000000819
Kannus P, Niemi S, Sievanen H, Korhonen N, Parkkari J (2016) Fall-induced fractures of the calcaneus and foot in older people: nationwide statistics in Finland between 1970 and 2013 and prediction for the future. Int Orthop 40(3):509–512. https://doi.org/10.1007/s00264-015-2875-7
Rausch S, Klos K, Wolf U, Gras M, Simons P, Brodt S, Windolf M, Gueorguiev B (2014) A biomechanical comparison of fixed angle locking compression plate osteosynthesis and cement augmented screw osteosynthesis in the management of intra articular calcaneal fractures. Int Orthop 38(8):1705–1710. https://doi.org/10.1007/s00264-014-2334-x
Nelson JD, McIff TE, Moodie PG, Iverson JL, Horton GA (2010) Biomechanical stability of intramedullary technique for fixation of joint depressed calcaneus fracture. Foot Ankle Int 31(3):229–235. https://doi.org/10.3113/FAI.2010.0229
Kammerlander C, Neuerburg C, Verlaan JJ, Schmoelz W, Miclau T, Larsson S (2016) The use of augmentation techniques in osteoporotic fracture fixation. Injury 47(Suppl 2):S36–S43. https://doi.org/10.1016/S0020-1383(16)47007-5
Thordarson DB, Bollinger M (2005) SRS cancellous bone cement augmentation of calcaneal fracture fixation. Foot Ankle Int 26(5):347–352. https://doi.org/10.1177/107110070502600501
Riederer BM, Bolt S, Brenner E, Bueno-López JL, Circulescu ARM, Davies DC, De Caro R, Gerrits PO, McHanwell S, Pais D, Paulsen F, Plaisant O, Sendemir E, Stabile I, Moxham BJ (2012) The legal and ethical framework governing body donation in Europe – 1st update on current practice. Eur J Anat 16(1):1–21
Hungerer S, Eberle S, Lochner S, Maier M, Hogel F, Penzkofer R, Augat P (2013) Biomechanical evaluation of subtalar fusion: the influence of screw configuration and placement. J Foot Ankle Surg 52(2):177–183. https://doi.org/10.1053/j.jfas.2012.11.014
Chuckpaiwong B, Easley ME, Glisson RR (2009) Screw placement in subtalar arthrodesis: a biomechanical study. Foot Ankle Int 30(2):133–141. https://doi.org/10.3113/FAI.2009.0133
Gonzalez TA, Ehrlichman LK, Macaulay AA, Gitajn IL, Toussaint RJ, Zurakowski D, Kwon JY (2016) Determining measurement error for Bohler’s angle and the effect of X-ray obliquity on accuracy. Foot Ankle Spec 9(5):409–416. https://doi.org/10.1177/1938640016656236
Eichinger M, Schmoelz W, Brunner A, Mayr R, Boelderl A (2015) Subtalar arthrodesis stabilisation with screws in an angulated configuration is superior to the parallel disposition: a biomechanical study. Int Orthop 39(11):2275–2280. https://doi.org/10.1007/s00264-015-2944-y
Chen W, Liu B, Lv H, Su Y, Chen X, Zhu Y, Du C, Zhang X, Zhang Y (2017) Radiological study of the secondary reduction effect of early functional exercise on displaced intra-articular calcaneal fractures after internal compression fixation. Int Orthop 41(9):1953–1961. https://doi.org/10.1007/s00264-017-3533-z
Yu S, McDonald T, Jesudason C, Stiller K, Sullivan T (2014) Orthopedic inpatients’ ability to accurately reproduce partial weight bearing orders. Orthopedics 37(1):e10–e18
Qiang M, Chen Y, Jia X, Zhang K, Li H, Jiang Y, Zhang Y (2017) Post-operative radiological predictors of satisfying outcomes occurring after intra-articular calcaneal fractures: a three dimensional CT quantitative evaluation. Int Orthop 41(9):1945–1951. https://doi.org/10.1007/s00264-017-3577-0
Bailey EJ, Waggoner SM, Albert MJ, Hutton WC (1997) Intraarticular calcaneus fractures: a biomechanical comparison or two fixation methods. J Orthop Trauma 11(1):34–37
Goldzak M, Simon P, Mittlmeier T, Chaussemier M, Chiergatti R (2014) Primary stability of an intramedullary calcaneal nail and an angular stable calcaneal plate in a biomechanical testing model of intraarticular calcaneal fracture. Injury 45(Suppl 1):S49–S53. https://doi.org/10.1016/j.injury.2013.10.031
Thordarson DB, Hedman TP, Yetkinler DN, Eskander E, Lawrence TN, Poser RD (1999) Superior compressive strength of a calcaneal fracture construct augmented with remodelable cancellous bone cement. J Bone Joint Surg Am 81(2):239–246
Acknowledgments
We want to thank Nora Klier for assisting with the surgical procedures and testings, Cornelia Qadri for her competent technical support and Clemens Unterwurzacher for photography and illustrations. Martin Eichinger received a research grant by DePuy Synthes, J&J Austria. Additionally, we would like to thank all body donors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eichinger, M., Brunner, A., Stofferin, H. et al. Screw tip augmentation leads to improved primary stability in the minimally invasive treatment of displaced intra-articular fractures of the calcaneus: a biomechanical study. International Orthopaedics (SICOT) 43, 2175–2181 (2019). https://doi.org/10.1007/s00264-018-4171-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4171-9