Abstract
Purpose
The sacrum is a mechanical nucleus working as the base for the spinal column, as well as the keystone of the pelvic ring. Thus, injuries of the sacrum can lead to biomechanical instability and nerve conduction abnormality.
Methods
The common classification is the Denis classification, but these fractures are often part of a lesion of the posterior pelvic ring and therefore the Tile classification is very useful. The goals of operative intervention are to reduce fracture fragments, protect neurological structures, and provide adequate stability for early mobilization.
Results
The stabilization of these injuries can be difficult even in a patient with adequate bone stock and concomitant medical comorbidities. The posterior-ring tension-band metallic plate and sacroiliac joint screw are two commonly used methods for posterior internal fixation of the pelvis.
Conclusions
In this study, we evaluate the differences, in the treatment of sacral fractures, between the two techniques, revising the literature and our experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sacral fractures are often due to high-energy traumas and are connected to fractures of the pelvic ring (pubic symphysis, sacroiliac joint). They are rarely associated with acetabular fracture [1].
The diagnosis of isolated sacral fracture is often unknown since patients show faint pain, which is often taken for low back pain, and appear neurologically intact [2]. Actually, since patients show no neurological symptoms, in 75% of cases, treatment of these fractures is conservative [3, 4]. Therefore, accurate clinical examination and I and II level imaging exams (X rays, CT imaging and RMN) are fundamental in order to classify and frame the fracture pattern and choose the type of treatment.
The aims of our article are to review the literature on the subject and study our casuistry by evaluating remote results according to the type of fracture and surgical treatment. Retrospective clinical evaluation was performed through two scores (Hannover Poltrauma Score and Sf 36) from January 2012 to December 2017.
The sacrum bone consists of five vertebrae which fuse gradually and completely during adulthood [5]. The only joints that do not fuse are L5-S1 with intervertebral disc interposition, the sacroiliac joint and finally, the sacrum coccyx joint between S5 and the coccyx. With this regard, however, several anatomical variables should be examined while planning synthesis in this anatomical region [6].
The lumbosacral articulation is the part of the vertebral column with most anatomical variables. Such sacral dysmorphiais found in 30%–40% of patients [6, 7]. Actually, the number of vertebrae in the thoraco-lumbar-sacral region is the same, but the levels of sacral fusion may change. “Transition defects” between L5 and S1, that may be total or partial, alter the anatomy of the sacral ala and the inclination of the sacrum bone itself.
Therefore, trans-iliac-sacral screw synthesis must not leave aside accurate, preoperative x-ray imaging, three projections at least (anterior posterior, inlet, outlet), of the hip bone and CT imaging [6,7,8].
For instance, in case of L5 sacralization, that is, when the sacrum fuses cranially with the fifth lumbar vertebra, the level of sacrum fusion and verticalizationis best evaluated by hip outlet projections. With regard to transsacral screw insertion, an increased superior sacral region inclination is important, as well. Actually, a greater inclination of this region, which can be easily seen either with a radiographic projection of the sacrum and an outlet, makes synthesis more difficult. Moreover, because of these variables, the view of the sacral foramina is difficult and the sacral ala inlet projection will show more extended recess on the anterior cortical [6,7,8].
Moreover, intra-operative studies compared the iliac anterior cortical bone density of the sacroiliac articulation (ICD) in patients with and without sacral dysmorphism. Lateral CT cuts emphasize such correlation and non-dysmorphic patients show coplanar sacral and iliac wing cortex at the level of the iliac-sacral articulation [6]. This helps the surgeon to read the projections during synthesis correctly. Otherwise, in patients with this anatomical variable, screw insertion becomes more difficult and carries the risk of inserting the screw on S1 nerve root. The morphology of the sacral cranial region is determining when inserting sacral screws due to the presence of sacral foramina that let out sacral nerve roots that do not appear perfectly spherical on conventional radiography, but elliptical and oval in shape [6].
Consequently, there are different sacral screw-insertion safety zones [9, 10], depending on the presence or not of anatomic dysmorphisms. The position of the patient on the operating table is highly influencing, as well. In a patient in supine position, especially when superior sacral dysmorphisms are present, the correct positioning of the screw requires a slantwise anterior-posterior and caudocranial direction, because dysmorphism produces a more oblique and narrower bone passageway for the screw. It all depends on patient habitus and positioning on the operating room table (more difficult when supine). On the other hand, the absence of dysmorfisms determines anterior, caudal direction [7].
Therefore, careful and deep pre-operative planning with CT imaging is primary for a correct trans-iliac-sacral screw insertion, which, as stated, changes between patients with and without sacral dysmorfisms. For this reason, a standard acquisition of pre-operative CT cuts is necessary. Three projections, at least, are always essential: posterior-anterior and oblique inlet and outlet, according to Judet [6, 7]. The intra-operative lateral projection is always radiology-technician dependent. A clear, pre-operative CT view is, therefore, fundamental.
Materials and methods
Our study considered 40 cases of sacral fractures with an average 21-month follow-up, from January 2012 to December 2017. Patients were aged 47 on average, the oldest 68 and the youngest ten. The study included patients with sacral fractures which were isolated or associated to posterior pelvic ring injury and which were treated surgically in our centre with trans-ileo-sacral screws (19) or percutaneous posterior plate (21). Two cases that initially underwent screw osteosynthesis required revision with plate. Pre-operative assessment was performed on patients by means of X-ray imaging and CT scan.
Treatment choice depends either on the type of fracture (Denis/TILE AO classification) and clinical complexity, as well as on the surgeon’s experience. Of the isolated sacral fractures, six “DANIS I” fractures were treated with trans-ileo-sacral screws and only one was treated with back plate; six “DANIS II” were treated with plate (including the cases treated with screw beforehand and then with plate) and three with screws. All of the “DANIS III” cases were treated with plates, three of them showing pre-operative neurological symptoms (L5-S1 radiculopathy with unilateral dysesthesia and urinary and fecal incontinence. As for sacral fractures associated with posterior pelvic ring lesions, three cases of TILE C1 underwent trans-ileo-sacral screw ostheosynthesis and one plate ostheosynthesis; five cases of TILE C2 were screw-treated and six were plate-treated; a TILE C3 case was treated with trans-ileo-sacral screw and the remaining three were plate-treated (Fig. 1).
Clinical and radiographic assessments took place three, six, 12, and 20 months after surgery. The patients where set in four more groups according to clinical complexity through the Hannover Polytrauma score, a validated scoring system for the treatment and assessment of politrauma patients (social, psylogical, economic status, state of rehabilitation and/or presence of other contextual lesions. The patients’ “Quality of Life” was assessed through an SF-36 standard questionnaire which provides an estimation of physical health (physical activities, limitations in daily activities and physical pain), general health (general well-being and vitality), and psychological-emotional health (limitations because of social and/or emotional reasons and mental health). The SF36 questionnaire was administered six, 12, and 20 months after surgery.
Results
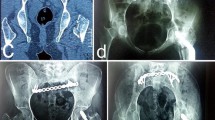
Surgery treatment choice depended on the clinical and radiographic complexity of the lesion. Difficulties arise in a screw-treated case concerning correct screw insertion because of sacrum anatomical variations. One of the patients who underwent trans-ileo-sacral screw osteosynthesis showed L5 deficit symptoms immediately after surgery. Therefore, synthesis was revised and the screw was replaced with a percutaneous posterior plate. Symptmatology was resolved within six months (Fig. 2).
Back-plate treatment proved longer biomechanical stability in the absence of secondary complications (scomposition, breaking or mobilization of synthesis tools).Only in one case treated with a posterior plate with an imperfect fracture reduction was an evolution in pseudoarthrosis, both of the sacral fracture, of the ileopubic and ischio-pubic branch.One of the screw synthesizes failed with nonunion after fracture fragment mobilization and decomposition. Patients with post trauma neurological lesions got better in time until complete recovery. Compared to cases of equal clinical and radigraphic complexity, plate treatment allowed an earlier charging (30 days) than screw treament (45 days). Periodic evaluation (SF36 form) showed a better clinical outcome in younger patients, likely due to initial general clinical conditions and larger bone stock. Clinical and radiographic outcomes in both, trans-ileo-sacral-screw and percutaneous-back-plate-treated patients, are superimposable, even though the latter showed more complex fractures (Tables 1, 2, and 3).
Discussion and literature review
Posterior pelvic injuries strongly affect post traumatic survival and mortality. They very often result in disabling, irreversible outcomes as, for instance, neurological deficits, pelvic obliquity with secondary scoliosis difficulty in ambulation and maintaining sitting posture. All these complications show very slow recovery. They are difficult to treat and therefore disabling for the patient’s daily and working activities. Such lesions represent a challenge from a surgical point of view.
To this regard, several authors have described their casuistry, but unfortunately, they have not reached a unanimous opinion concerning the choice of synthesis tools according to the type of fracture, positioning of the patient in the surgery room, or about when a conservative, bloodless treatment can take place (Fig. 3).
In 1997, Routt et al. [11] enrolled 177 patients in a prospective study on posterior pelvic-ring unstable lesions, in a top level traumatology centre. Patients were aged 11–78. They all showed Tile-classified [12] lesions. A 10-month follow-up involved 159 patients. Recovery was proved by clinical and radiological assessment: clinical recovery was considered complete when asymptomatic, full charge tolerance was proved. Instead, radiological recovery became evident on fracture remodeling and/or dislocation without implant failure. Complications were caused by inadequate imaging, surgical mistakes, and implant fixation defects. Imaging problems were especially due to obesity in nine patients and to abdominal contrast in other nine patients. Oblique projections, not latero-lateral, were employed in all these patients [12]. Poor understanding of the sacral anatomy was the main cause of the wrong positioning of two trans-ileo-sacral screws inside a vertebra, with no further sequelae. The study pointed out a problem, that is, lack of a complete and steady guide to screw insertion through plain ortagonal fluoroscopy. This is the reason why, already in the past, they used CT imaging, in order to avoid misunderstanding and problems with fluoroscopy imaging (Fig. 4).
In 1999, Altman et al. [13] published a case report about a 69-year-old patient who had fallen off his house roof. The patient had a medical history of hypertension and former cerebrovascular accidents. The author reported this case as the first case in literature of trans-ileo-sacral screw osteosynthesis dealing with an upper gluteal artery lesion, probably fostered by the important calcification of the same vessel. Likely, an open procedure could have avoided such emergency.
In 2001, Nork et al. [14] studied 442 patients. Among them, he pointed out 13 patients with U-shaped sacral fracture: a very rare fracture, that must be suspected when backbone axial loading lesions occur. Five patients had further spinal injury, eight showed several lumbar transverse process fractures and three showed bilateral calcaneal fracture. All the patients were treated with trans-ileo-sacral screw osteosynthesis: 11 had bilaterally inserted screws, one got two screws on a single side and another one got only one screw. Post-operative CT imaging proved that the intraosseous insertion of the screws had not damaged the course of the nerve and the cortical in none of the patients who underwent surgery. Actually, neurological alterations are commonly associated to this kind of fracture and show an incidence of about 85%, in line with the outcomes of this study: signs and symptoms of cauda equine, along with sacral nerve root deficits are pretty frequent. The role of osteosynthesis in surgery decompression is defined only to a minimum extent in literature. Instead, the rate of patients with a significantly improved post-operative neurological functionality is surprisingly high. Nork [14] noticed that it concerned 77% of the sample. When completed, the study pointed out that surgical stabilization allows an early and safe mobilization on declivous position. Compared to open procedure, percutaneous intervention reduced blood loss and operative timing, besides preventing progress of kyphotic deformity and associated nerve injuries.
In 2016, Bi et al. [15] published a retrospective and comparative study which compared posterior plate osteosinthesis and trans-ileo-sacral screw osteosynthesis. The study included 46 patients who had been hospitalized between June 2010 and May 2014 because of unstable posterior pelvic-ring lesions. Twenty-four had undergone screw insertion surgery (study group) and 22 compression plate surgery (control group). The outcomes were promoting. First of all, none of the two groups showed iatrogenic neuro-vascular injuries. All the 46 patients had up to 14–33-month follow-up (24.5 months on average) and no breaking or mobilization of the internal fixing implant occurred. On the other hand, a statistical difference (P value < 0.0001) in some of the parameters examined at the beginning of the study was observed. On average, timing of surgery was 22.08 ± 1.91 minutes for screw osteosynthesis, and 38.18 ± 2.97 minutes for plate osteosynthesis. The length of the cut was noteworthy, as well: 3.63 ± 0.49 cm for the group study and 7.70 ± 0.55 for the control group. Finally, intra-operative bleeding resulted in 43.42 ± 4.9 mL for screw osteosynthesis, and 161.59± 21.24 mL for plate osteosynthesis [15]. The study ended up with a few remarks. Back plates are valid and sufficiently strong in bilateral sacroiliac dislocation fixation. However, they do show some weaknesses. First of all, in order to draw the plate near the irregular cortical of the back pelvic-ring, it is necessary to bend the plate: this modification and deformation procedure reduces resistance and may even damage the screw holes and it is often not sufficiently precise. Posterior plates also carry the risk of damaging blood vessels and nerve tissue when soft tissues are exceedingly unstuck. Moreover, a number of patients who underwent plate osteosynthesis feel uncomfortable during supine decubitus position, mainly those with little fat. Actually, in order to avoid problems, plates should be positioned in an area with a substantial amount of subcutaneous fat [15]. Finally, posterior plates are responsible for reduced functionality in patients and they cannot be used for the compression or separation of sacral fractures. The relatively small sample and the lack of follow up and long term functional outcomes are the limiting factors of this study. Of course, the advantages of trans-ileo-sacral screw ostoesynthesis, the significant statistical power and the limitations resulting from the use of plates, are outstanding [15].
A very recent study by Elzohairy et al. (2017) [16] tested posterior pelvic ring injuries on 70 patients, from June 2005 to December 2012. Inclusion criteria selected patients who had been operated with open reduction internal fixation (ORIF) or who had been treated with trans-ileo-sacral screws. The study pointed out the advantages of employing trans-ileo-sacral screws in a closed reduction: better long-term functional outcomes, more significant radiographic reduction, shorter surgery timing, reduction of blood loss in theater and reduction in the request and transfusion of blood units [16].
In 2012, Chen, H et al. [17] produced a retrospective and comparative study on two of the most common osteosynthesis interventions (with plates and with trans-ileo-sacral screws). Between March 2002 and October 2007, they enrolled 58 patients with clear inclusion criteria: unstable dislocation of the sacroiliac joint and vertical sacral fractures, no need for sacral nerve or sacral canal decompression, complete, or at least important post traction repositioning of the fracture. Besides that, the patients should not show mental or nervous, daily life altering disorders. All the enrolled patients showed Tile C [12] posterior pelvic-ring lesions and all underwent complete 12–36-month follow-up. The patients were divided in two groups of 29. Important statistic differences were pointed out: intraoperative bleeding (48.71 ± 17 mL for the group with screws, 168.61 ± 40 mL for the group with plates), length of the procedure (42 ± 7.9 minutes for plate osteosynthesis, 58 ± 9.04 minutes for screw osteosynthesis) and the cut (4.36 ± 0.99 cm plate trated patients, 1.66 ± 0.42 cm for screw treated patients). Clinical assessment of the patients was performed through Majeed score, which considered pain reported, ability to stay in sitting and standing position, sexual dysfunctions and working ability. Plate osteosynthesis scored 62–95 points, while trans-ileo-sacral screw osteosynthesisscored 66–97 points, with 86 and 88% values of excellence respectively. Chen et al. [17] underlined the reduction of nerve tissue and vascular risk factors in plate osteosynthesis, but all clinical and intra-operative assessment parameters explain the wide employment of trans-ileo-sacral screws in the ultimate surgery of these lesions: they are more advantageous from several points of view. Among them, the most important are intra-operative bleeding and long-term outcomes.
In 2014, Acklin et al. [18] published a retrospective study that considered 27 patients, from 2003 to 2011, aiming to the assessement of posterior pelvic-ring lesions type C according to Tile [12], treated with double-plate osteosynthesis. This approach was meant to prove higher implant strength and solidity, but it also pointed out significant limitations. Five patients showed immediate post-operative course infections and five more needed implant removal: besides that, they all complained problems in sitting position. Infection was not that infrequent in consideration of the wide cut due to reduction and the significant slot and exposure of soft-tissues. The advantages of this kind of approach are evident: anatomical direct reduction, clearness of the sacral canal open in front of the surgeon, reduced soft-tissue irritation, and major stability. However, dangerous limitations, especially excessive soft tissue dissection and highly increasing risk of infection, diminished the advantages.
Conclusions
The outcomes of statistics in literature and the values reported in our retrospective study lead to substantial equality in the clinical and radiological outcomes of the two osteosynthesis operations, plate based and trans-ileo-sacral screw based [19]. Of course, plate osteosythesishas been introduced recently, so follow-up data are still poor with regard to clinical assessment of patients. Benefits are recognized about the stability and resistance gained with implants, but available data are still too little to state that this is the operation to be preferred definitely in the long term. Trans-ileo-sacral screw osteosynthesis represents, to date, the first choice in reduction and stabilization interventions. This was the first massively used procedure. Bibliography shows that it is still the most used intervention, the one with wider long-term follow-up. Clinical outcomes are comparable and even higher than plate osteosynthesis outcomes [20]. Collected data validate the theory that it is the best, in consideration of the early and fast restart of daily activities. Notwithstanding, this paper wants to show that the chapter of pelvic ring injuries is not based on the importance of definitive treatment, but on primary treatment performed by the Trauma Team, and how the operating table is reached. We still need a classification allowing emergency surgeons, anaesthetists and orthopaedic doctors to estimate rotational stability/instability of the pelvic ring osteoligamentous segments (there are plenty of morphology and anatomy classifications). Even more, we need classifications that can provide a precise idea of haemodynamic stability/instability, which substantially outline the patient’s surgical and clinical future. It is important to provide a classification or, at least, a diagnostic algorithm that will help in managing this broad, yet marginal topic of traumatology and raise the extremely high data of morbility and mortality carried on by these lesions. Complete team work will help in developing solutions to patients’ complex and severe problems that still lack exhaustive responses.
References
Eastridge BJ, Starr A, Minei JP, O’Keefe GE, Scalea TM (2002) The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. J Trauma 53(3):446–50-1
Poole GV, Ward EF (1994) Causes of mortality in patients with pelvic fractures. Orthopedics 17(8):691–696
Pohlemann T, Bosch U, Gänsslen A, Tscherne H (1994) The Hannover experience in management of pelvic fractures. ClinOrthopRelat Res 305:69–80
Schütz M, Stöckle U, Hoffmann R, Südkamp N, Haas N (1996) Clinical experience with two types of pelvic C-clamps for unstable pelvic ring injuries. Injury 27:p:46–50
Mohamad Bydon, Vance Fredrickson, R de la Garza-Ramos, Yiping L, RA Lehman Jr, GR Trost, ZL Gokaslan, (2014) Sacral fractures. AANS;37 (1)
Miller AN, Chip Routt ML Jr (2012) Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg 20(1):8–16
Conflitti JM, Graves ML, Chip Routt ML Jr (2010) Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma 24:630–636
Futamura K, Baba T, Mogami A, Morohashi I, Obayashi O, Iwase H, Kaneko K (2018) A biomechanical study of sacroiliac rod fixation for unstable pelvic ring injuries: verification of the “within ring” concept. Int Orthop 42(4):909–914. https://doi.org/10.1007/s00264-017-3713-x
Dubory A, Bouloussa H, Riouallon G, Wolff S (2017) A computed tomographic anatomical study of the upper sacrum. Application for a user guide of pelvic fixation with ilioscral screws in adult spinal deformity. Int Orthop 41(12):2543–2553. https://doi.org/10.1007/s00264-017-3580-5
Pishnamaz M, Dienstknecht T, Hoppe B, Garving C, Lange H, Hildebrand F, Kobbe P, Pape HC (2016) Assessment of pelvic injuries treated with ilio-sacral screws: injury severity and accuracy of screw positioning. Int Orthop 40(7):1495–1501. https://doi.org/10.1007/s00264-015-2933-1
Routt MLC, Simonian PT, Mills WJ (1997) Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma 11(8):584–589
Tile M (1996) Acute pelvic fractures: I. Causation and classification. J AmAcadOrthopSurg 4(3):143–151
Altman DT, Jones CB, Routt MLC (1999) Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma 13(3):220–222
Nork SE, Jones CB, Harding SP, Mirza SK, Routt MLC (2001) Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 15(4):238–246
Bi C, Wang Q, Nagelli C, Wu J, Wang Q, Wang J (2016) Treatment of unstable posterior pelvic ring fracture with pedicle screw-rod fixator versus locking compression plate: a comparative study. Med SciMonit 22:3764–3770
Elzohairy MM, Salama AM (2017) Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. OrthopTraumatolSurg Res 103(2):223–227
Chen HW, Liu GD, Fei J et al (2012) Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. J Orthop Sci 17(5):580–587
Acklin Y, Marco G, Sommer G(2014) Double locking plate fixation of sacral fractures in unstable pelvic ring C-type injuries.;(11):p: 1–6. https://doi.org/10.1007/s00064-014-0307-2
Futamura K, Baba T, Mogami A, Kanda A, Obayashi O, Iwase H, Kaneko K (2018) “Within ring”-based sacroiliac rod fixation may overcome the weakness of spinopelvic fixation for unstable pelvic ring injuries: technical notes and clinical outcomes. Int Orthop 42(6):1405–1411. https://doi.org/10.1007/s00264-017-3712-y
Wang H, Fu YH, Ke C, Zhuang Y, Zhang K, Wei X, Li Z, Lei JL, Zhang BF, Liu P (2018) Minimally invasive stabilisation of posterior pelvic ring instabilities with pedicle screws connected to a transverse rod. Int Orthop 42(3):681–686. https://doi.org/10.1007/s00264-017-3714-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board statement
The study was reviewed and approved by the internal ethics committee of orthopedics and traumatology department of Policlinico Gemelli Hospital.
Informed consent statement
All involved persons gave their verbal informed consent prior to being included in the analysis.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liuzza, F., Silluzio, N., Florio, M. et al. Comparison between posterior sacral plate stabilization versus minimally invasive transiliac-transsacral lag-screw fixation in fractures of sacrum: a single-centre experience. International Orthopaedics (SICOT) 43, 177–185 (2019). https://doi.org/10.1007/s00264-018-4144-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4144-z